Monday Poster Session
Category: Liver
P3761 - SGLT-2 Inhibitors Are Associated With Lower Risk of Hepatic Decompensation in Metabolic Dysfunction Associated Steatotic Liver Disease: Real-World Evidence
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JF
Jake D. Fanizza, BS (he/him/his)
Drexel University College of Medicine
Harrisburg, PA
Presenting Author(s)
Jake D. Fanizza, BS1, Sarah A. Taekman, BA2, Babak Mirminachi, MD3, Anas Atrash, MD3
1Drexel University College of Medicine, Harrisburg, PA; 2Drexel University College of Medicine, Ardmore, PA; 3University of Pittsburgh Medical Center, Harrisburg, PA
Introduction: Sodium-Glucose Cotransporter-2 (SGLT-2) Inhibitors are primarily known for their glucose-lowering properties and favorable cardiovascular outcomes, including reduced cardiovascular events and hospitalizations for heart failure. However, evidence regarding their effects in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) remains limited. While some studies suggest a beneficial impact on liver fibrosis, others do not. This study aims to evaluate liver-related outcomes associated with SGLT-2 inhibitor use in patients with MASLD using real-world data.
Methods: This retrospective cohort study was conducted using the nationwide deidentified TriNetX database. We included patients diagnosed with fatty liver disease between 2015 and 2025 who had at least one cardiometabolic risk factor. Patients with pre-existing compensated or decompensated cirrhosis were excluded. Participants were stratified based on first time exposure to SGLT-2 inhibitors within 1 year of MASLD diagnosis versus no exposure to SGLT-2 inhibitors within 1 year of MASLD diagnosis. The primary outcome was the incidence of decompensated cirrhosis at 5 year follow up. Propensity score matching was employed to balance baseline characteristics, including diabetes and cardiovascular disease as well as exposure to antidiabetic medications between the SGLT-2 exposed and unexposed groups.
Results: We identified 911,706 patients who met the criteria for MASLD. After propensity score matching, SGLT-2 therapy was associated with a significant reduction in the risk of incident decompensated cirrhosis (RR 0.924; 95% CI, (0.865, 0.987); p< 0.01). As expected, SGLT-2 use was also linked to a significant reduction in 5 year mortality (RR 0.50; 95% CI, (0.464, 0.539); p< 0.01). At the end of the 5 year follow-up period, mean laboratory changes were significantly greater in patients receiving SGLT-2 inhibitors 1 year after diagnosis: AST (-5.163 vs -0.201, p< 0.01), ALT (-10.074 vs -5.163, p< 0.01), and HbA1c (-0.602 vs -0.176, p< 0.01).
Discussion: SGLT-2 inhibitor use is associated with a reduced incidence of hepatic decompensation in patients with MASLD. These findings highlight the need for prospective, randomized clinical trials to further investigate the potential therapeutic benefits of SGLT-2 inhibitors in this population.
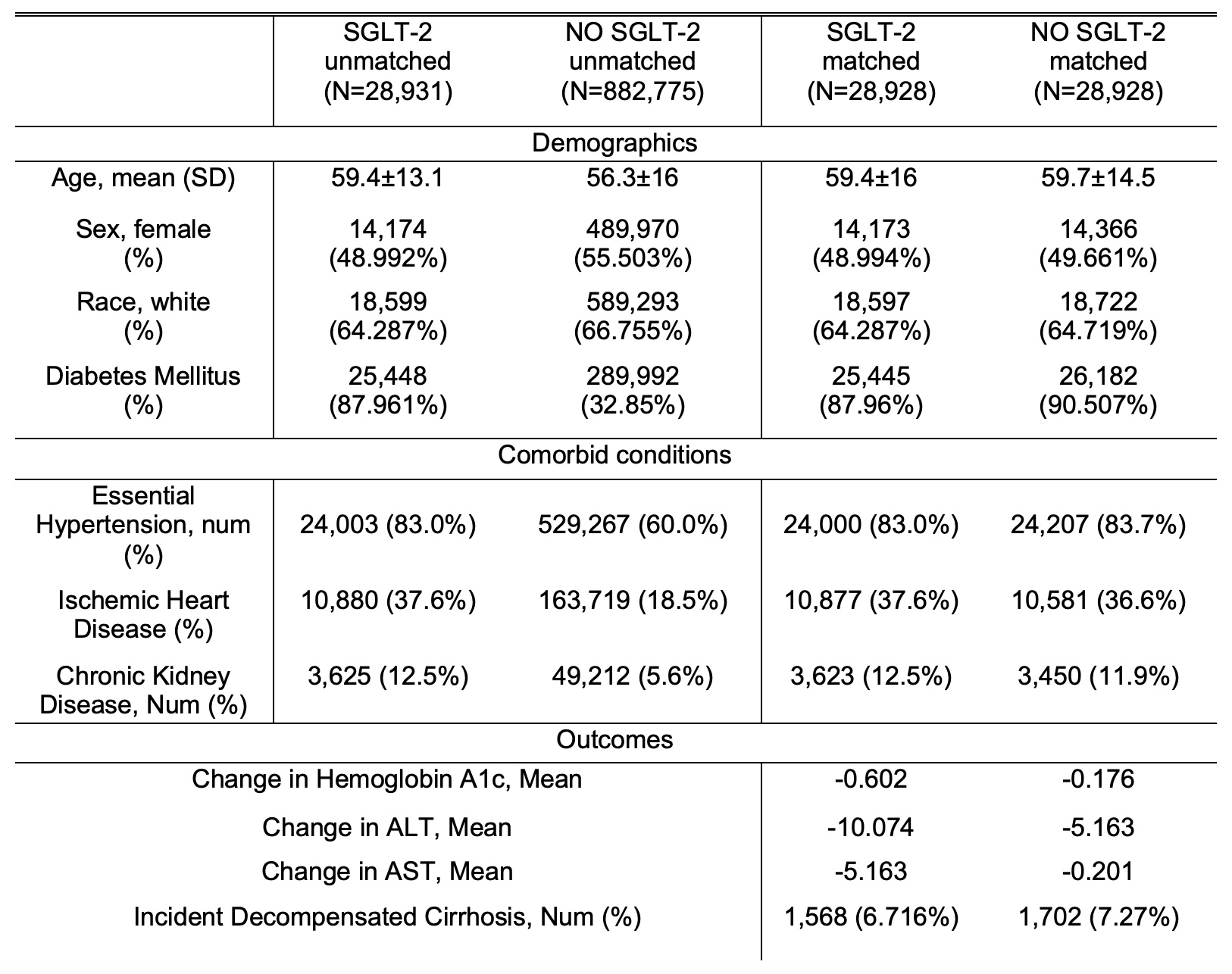
Figure: Demographics and Outcomes of Metabolic Dysfunction Associated Steatotic Liver Disease in Patients with SGLT-2 Exposure and with NO SGLT-2 Exposure

Figure: Kaplan-Meier Survival Curve for Decompensated Liver Cirrhosis in Patients with Metabolic Dysfunction Associated Steatotic Liver Disease
Disclosures:
Jake Fanizza indicated no relevant financial relationships.
Sarah Taekman indicated no relevant financial relationships.
Babak Mirminachi indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Jake D. Fanizza, BS1, Sarah A. Taekman, BA2, Babak Mirminachi, MD3, Anas Atrash, MD3. P3761 - SGLT-2 Inhibitors Are Associated With Lower Risk of Hepatic Decompensation in Metabolic Dysfunction Associated Steatotic Liver Disease: Real-World Evidence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Drexel University College of Medicine, Harrisburg, PA; 2Drexel University College of Medicine, Ardmore, PA; 3University of Pittsburgh Medical Center, Harrisburg, PA
Introduction: Sodium-Glucose Cotransporter-2 (SGLT-2) Inhibitors are primarily known for their glucose-lowering properties and favorable cardiovascular outcomes, including reduced cardiovascular events and hospitalizations for heart failure. However, evidence regarding their effects in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) remains limited. While some studies suggest a beneficial impact on liver fibrosis, others do not. This study aims to evaluate liver-related outcomes associated with SGLT-2 inhibitor use in patients with MASLD using real-world data.
Methods: This retrospective cohort study was conducted using the nationwide deidentified TriNetX database. We included patients diagnosed with fatty liver disease between 2015 and 2025 who had at least one cardiometabolic risk factor. Patients with pre-existing compensated or decompensated cirrhosis were excluded. Participants were stratified based on first time exposure to SGLT-2 inhibitors within 1 year of MASLD diagnosis versus no exposure to SGLT-2 inhibitors within 1 year of MASLD diagnosis. The primary outcome was the incidence of decompensated cirrhosis at 5 year follow up. Propensity score matching was employed to balance baseline characteristics, including diabetes and cardiovascular disease as well as exposure to antidiabetic medications between the SGLT-2 exposed and unexposed groups.
Results: We identified 911,706 patients who met the criteria for MASLD. After propensity score matching, SGLT-2 therapy was associated with a significant reduction in the risk of incident decompensated cirrhosis (RR 0.924; 95% CI, (0.865, 0.987); p< 0.01). As expected, SGLT-2 use was also linked to a significant reduction in 5 year mortality (RR 0.50; 95% CI, (0.464, 0.539); p< 0.01). At the end of the 5 year follow-up period, mean laboratory changes were significantly greater in patients receiving SGLT-2 inhibitors 1 year after diagnosis: AST (-5.163 vs -0.201, p< 0.01), ALT (-10.074 vs -5.163, p< 0.01), and HbA1c (-0.602 vs -0.176, p< 0.01).
Discussion: SGLT-2 inhibitor use is associated with a reduced incidence of hepatic decompensation in patients with MASLD. These findings highlight the need for prospective, randomized clinical trials to further investigate the potential therapeutic benefits of SGLT-2 inhibitors in this population.
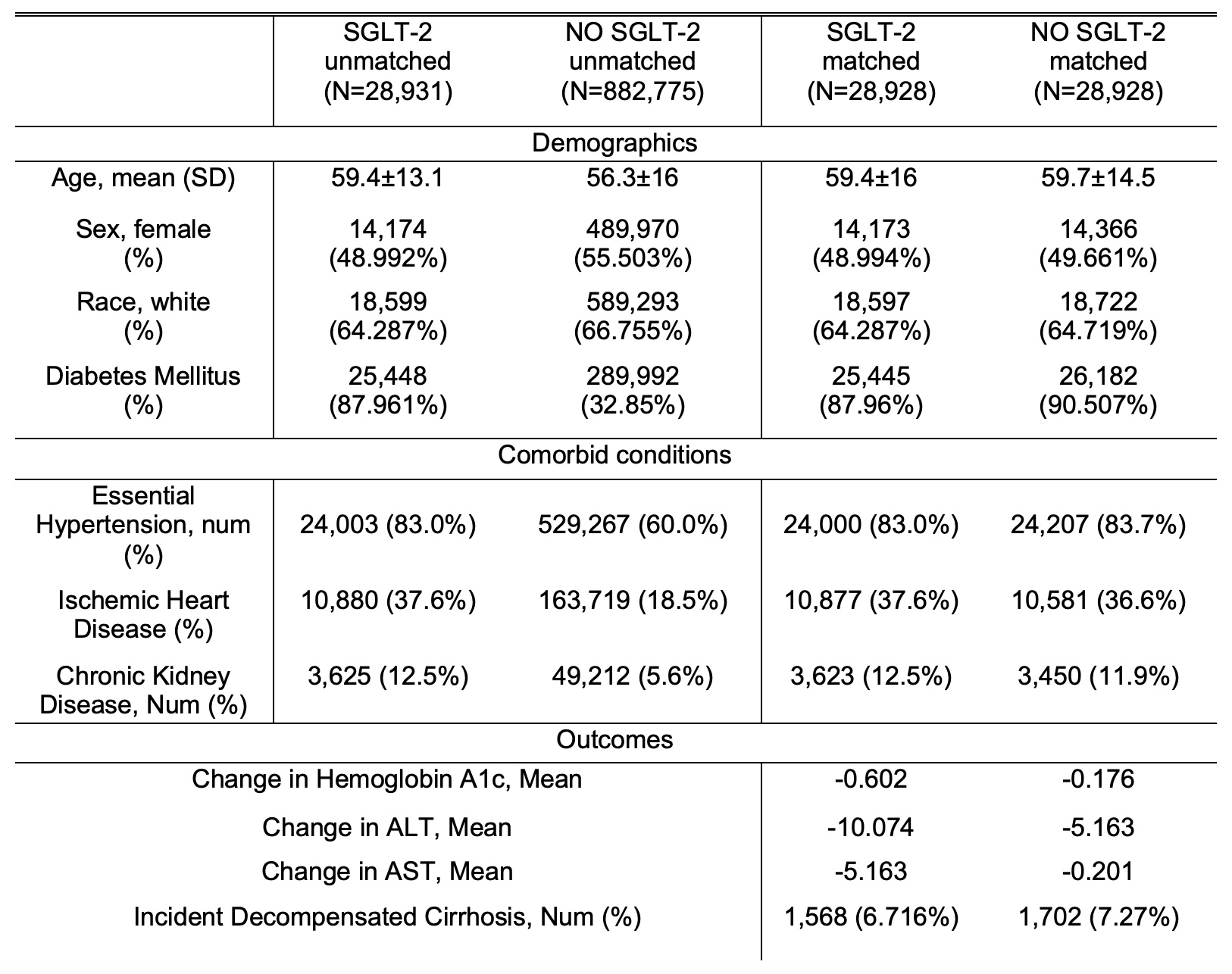
Figure: Demographics and Outcomes of Metabolic Dysfunction Associated Steatotic Liver Disease in Patients with SGLT-2 Exposure and with NO SGLT-2 Exposure

Figure: Kaplan-Meier Survival Curve for Decompensated Liver Cirrhosis in Patients with Metabolic Dysfunction Associated Steatotic Liver Disease
Disclosures:
Jake Fanizza indicated no relevant financial relationships.
Sarah Taekman indicated no relevant financial relationships.
Babak Mirminachi indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Jake D. Fanizza, BS1, Sarah A. Taekman, BA2, Babak Mirminachi, MD3, Anas Atrash, MD3. P3761 - SGLT-2 Inhibitors Are Associated With Lower Risk of Hepatic Decompensation in Metabolic Dysfunction Associated Steatotic Liver Disease: Real-World Evidence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
