Monday Poster Session
Category: Liver
P3748 - Exploring Costs, Demographics and Causative Agent in Patients Hospitalized for Drug-Induced Liver Injury
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Megan Kozar, MS, BS
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Megan Kozar, MS, BS1, Danielle Zolotnitsky, BS, RD1, Yunisse Gonzalez, MD2, Dina Halegoua-DeMarzio, MD2
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Drug-induced liver injury (DILI) is a leading cause of acute liver injury in the U.S., yet data quantifying its economic burden remains limited. This study characterizes DILI healthcare utilization within a single, large hospital system. Demographics and implicated agents were correlated with length of stay (LOS) and admission costs. LOS and cost were then compared to benchmarks from the Vizient Clinical database, a platform containing patient outcome data from > 1300 facilities nationwide.
Methods: We conducted a retrospective cohort study using data from a 32-hospital healthcare system using Epic EHR from October 2020 to January 2025. Patients were identified using diagnostic codes indicating DILI: K710, K711, K712, K716, K719, K720, K729, K759, and K762. Paired t-tests compared average observed LOS and cost among all cases to expected values from Vizient. Average LOS and cost were further compared to expected values in specific populations and among causative agents.
Results: A total of 48 admissions with a diagnosis of DILI were captured at relevant sites during the time period. This accounts for 0.01% of all admissions. When comparing DILI-related admissions to Vizient benchmarks, costs were significantly higher than expected (mean difference $2723.08; p=0.038). Observed LOS trended longer than expected but was not statistically significant (mean difference 1.41 days; p=0.051).
As noted in Table 1, females had a higher average difference in cost and LOS than males. Those who identified as black had the highest average difference in cost and LOS. Average cost differences were highest for cases involving multiple DILI-causing agents and antimicrobials and lowest for herbal and dietary supplements (HDS).
Discussion: DILI-related hospital admissions showed increased cost when compared to benchmarks provided by Vizient. This may reflect increased testing, interventions, or complexity in patients diagnosed with DILI. Notably, healthcare utilization among women and those identifying as black raise important questions about equity in diagnosis and care delivery. Cases involving antimicrobials and multiple agents were associated with the highest average LOS and cost, likely reflecting diagnostic uncertainty or complexity. A major study limitation was the low number of admissions for DILI, most likely due to lack of medical coding. This study indicates that DILI patients require extensive healthcare resources and suggests greater utilization in key populations and underlying causative agents.
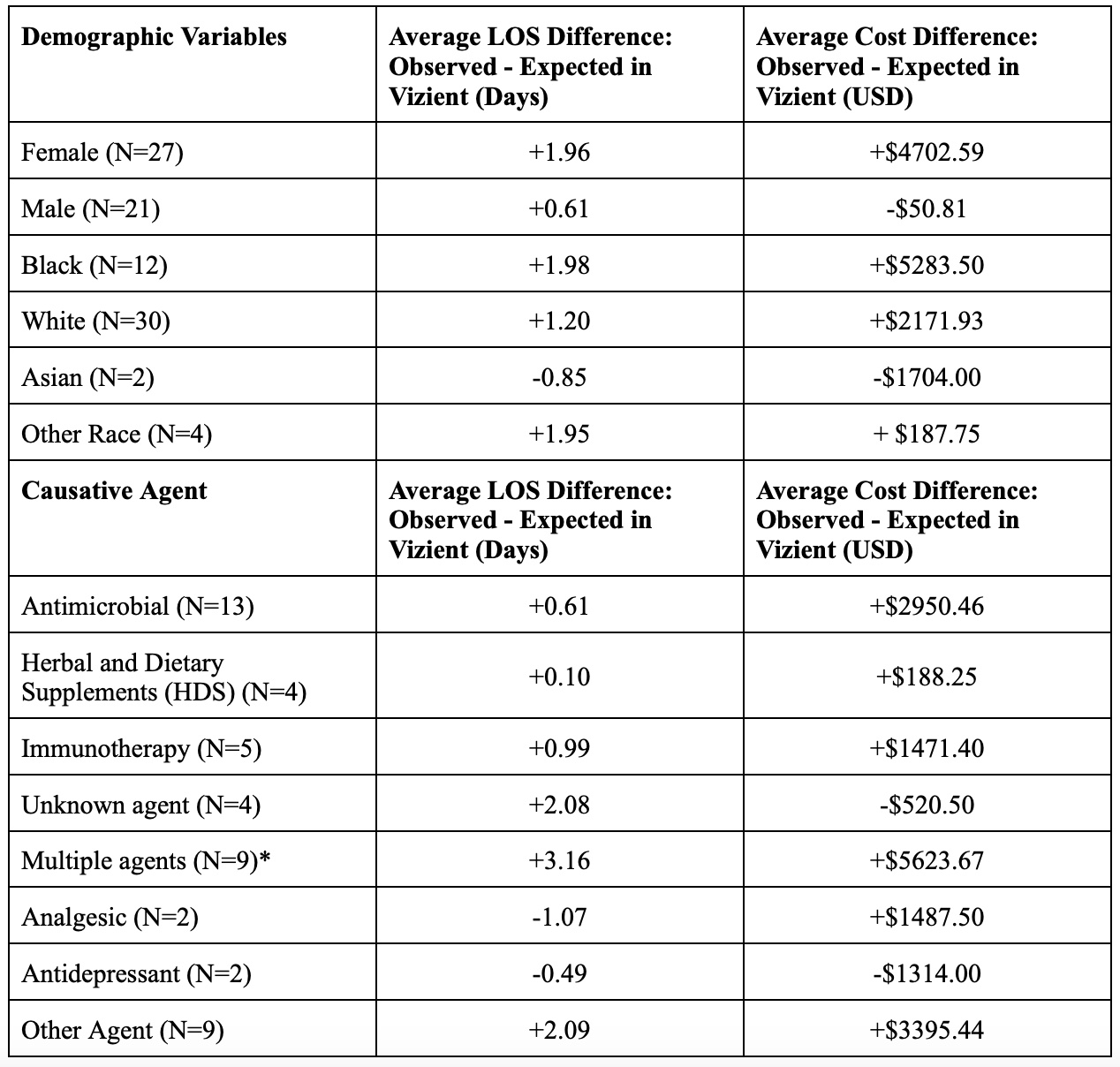
Figure: Table 1: Healthcare Utilization by Demographic and Causative Agent.
*More than one DILI-causing agent implicated.
Disclosures:
Megan Kozar indicated no relevant financial relationships.
Danielle Zolotnitsky indicated no relevant financial relationships.
Yunisse Gonzalez indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: 89BIO – Grant/Research Support. Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Novo Nordisk – Grant/Research Support. Vertex – Advisor or Review Panel Member.
Megan Kozar, MS, BS1, Danielle Zolotnitsky, BS, RD1, Yunisse Gonzalez, MD2, Dina Halegoua-DeMarzio, MD2. P3748 - Exploring Costs, Demographics and Causative Agent in Patients Hospitalized for Drug-Induced Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Drug-induced liver injury (DILI) is a leading cause of acute liver injury in the U.S., yet data quantifying its economic burden remains limited. This study characterizes DILI healthcare utilization within a single, large hospital system. Demographics and implicated agents were correlated with length of stay (LOS) and admission costs. LOS and cost were then compared to benchmarks from the Vizient Clinical database, a platform containing patient outcome data from > 1300 facilities nationwide.
Methods: We conducted a retrospective cohort study using data from a 32-hospital healthcare system using Epic EHR from October 2020 to January 2025. Patients were identified using diagnostic codes indicating DILI: K710, K711, K712, K716, K719, K720, K729, K759, and K762. Paired t-tests compared average observed LOS and cost among all cases to expected values from Vizient. Average LOS and cost were further compared to expected values in specific populations and among causative agents.
Results: A total of 48 admissions with a diagnosis of DILI were captured at relevant sites during the time period. This accounts for 0.01% of all admissions. When comparing DILI-related admissions to Vizient benchmarks, costs were significantly higher than expected (mean difference $2723.08; p=0.038). Observed LOS trended longer than expected but was not statistically significant (mean difference 1.41 days; p=0.051).
As noted in Table 1, females had a higher average difference in cost and LOS than males. Those who identified as black had the highest average difference in cost and LOS. Average cost differences were highest for cases involving multiple DILI-causing agents and antimicrobials and lowest for herbal and dietary supplements (HDS).
Discussion: DILI-related hospital admissions showed increased cost when compared to benchmarks provided by Vizient. This may reflect increased testing, interventions, or complexity in patients diagnosed with DILI. Notably, healthcare utilization among women and those identifying as black raise important questions about equity in diagnosis and care delivery. Cases involving antimicrobials and multiple agents were associated with the highest average LOS and cost, likely reflecting diagnostic uncertainty or complexity. A major study limitation was the low number of admissions for DILI, most likely due to lack of medical coding. This study indicates that DILI patients require extensive healthcare resources and suggests greater utilization in key populations and underlying causative agents.
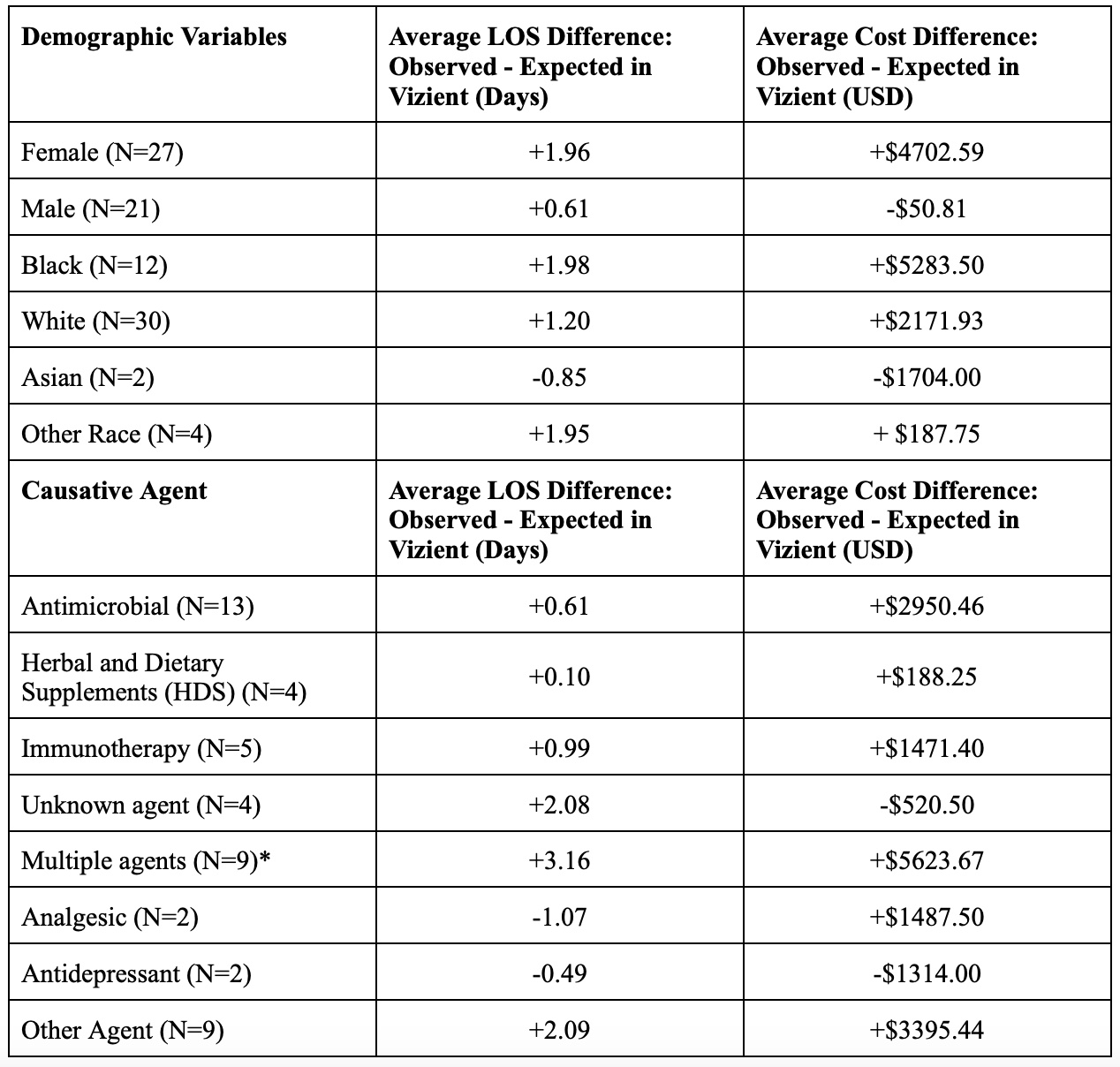
Figure: Table 1: Healthcare Utilization by Demographic and Causative Agent.
*More than one DILI-causing agent implicated.
Disclosures:
Megan Kozar indicated no relevant financial relationships.
Danielle Zolotnitsky indicated no relevant financial relationships.
Yunisse Gonzalez indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: 89BIO – Grant/Research Support. Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Novo Nordisk – Grant/Research Support. Vertex – Advisor or Review Panel Member.
Megan Kozar, MS, BS1, Danielle Zolotnitsky, BS, RD1, Yunisse Gonzalez, MD2, Dina Halegoua-DeMarzio, MD2. P3748 - Exploring Costs, Demographics and Causative Agent in Patients Hospitalized for Drug-Induced Liver Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
