Monday Poster Session
Category: Liver
P3745 - A Comparative Analysis of Rural and Urban Disparities in Alcohol-Associated Cirrhosis Outcomes: Insights From the National Inpatient Sample Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pooja Viswanath, MS, DO
University of New Mexico Health Sciences Center
Albuquerque, NM
Presenting Author(s)
Pooja Viswanath, MS, DO1, Niloy Ghosh, MD1, Niven Wang, DO2, Muhammad A. Nadeem, MD3, Mohammed Quazi, PhD4, Amir Sohail, MD, MSc5, Abu Baker Sheikh, MD1
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico Hospital, Albuquerque, NM; 3Cleveland Clinic, Cleveland, OH; 4West Virginia University, Morgantown, WV; 5University of New Mexico, Albuquerque, NM
Introduction: Rural-urban disparities in outcomes among patients with alcohol-associated liver disease (ALD) remain understudied at the national level. This study evaluated differences in inpatient outcomes, complications, and healthcare utilization among hospitalized adults with alcoholic cirrhosis across rural and urban populations in the United States.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2021), identifying adult hospitalizations with a primary diagnosis of alcoholic cirrhosis using ICD-10-CM codes. Rural-urban status was determined using patient residence data. Multivariable logistic and linear regression models were used to compare in-hospital mortality, complications, length of stay (LOS), and total hospitalization costs, adjusting for demographic, hospital-level, and clinical covariates.
Results: Among 422,670 hospitalizations for alcoholic cirrhosis, 13.2% were from rural areas. Rural patients were more likely to be older (mean age: 53.9 vs. 52.3 years), White (79.1% vs. 64.3%), from lower-income zip codes (household income ≤ $51,999: 56.6% vs. 30.0%), and have higher rates of smoking (56.7% vs. 52.3%) and obesity (14.3% vs. 12.6%) compared to urban patients. In-hospital mortality was significantly higher in rural patients (5.9% vs. 4.7%; adjusted odds ratio [aOR] 1.23, 95% CI: 1.12–1.34, p< 0.001). Rural patients also had increased odds of spontaneous bacterial peritonitis (aOR 1.19, 95% CI: 1.08–1.30) and variceal bleeding (aOR 1.18, 95% CI: 1.12–1.24). No significant differences were found in LOS or use of mechanical ventilation. Total hospitalization costs were significantly lower in rural patients ($64,690 vs. $82,236; p< 0.001).
Discussion: Rural patients hospitalized with alcoholic cirrhosis face higher risks of inpatient mortality and complications despite similar lengths of stay and lower hospitalization costs. These findings highlight persistent geographic disparities in cirrhosis care and underscore the need for targeted clinical and policy interventions in rural health systems. By leveraging a large, nationally representative dataset, this study adds important evidence on how rural residence is associated with worse inpatient outcomes in alcohol-associated liver disease, supporting the need for more equitable resource allocation and care models in hepatology.
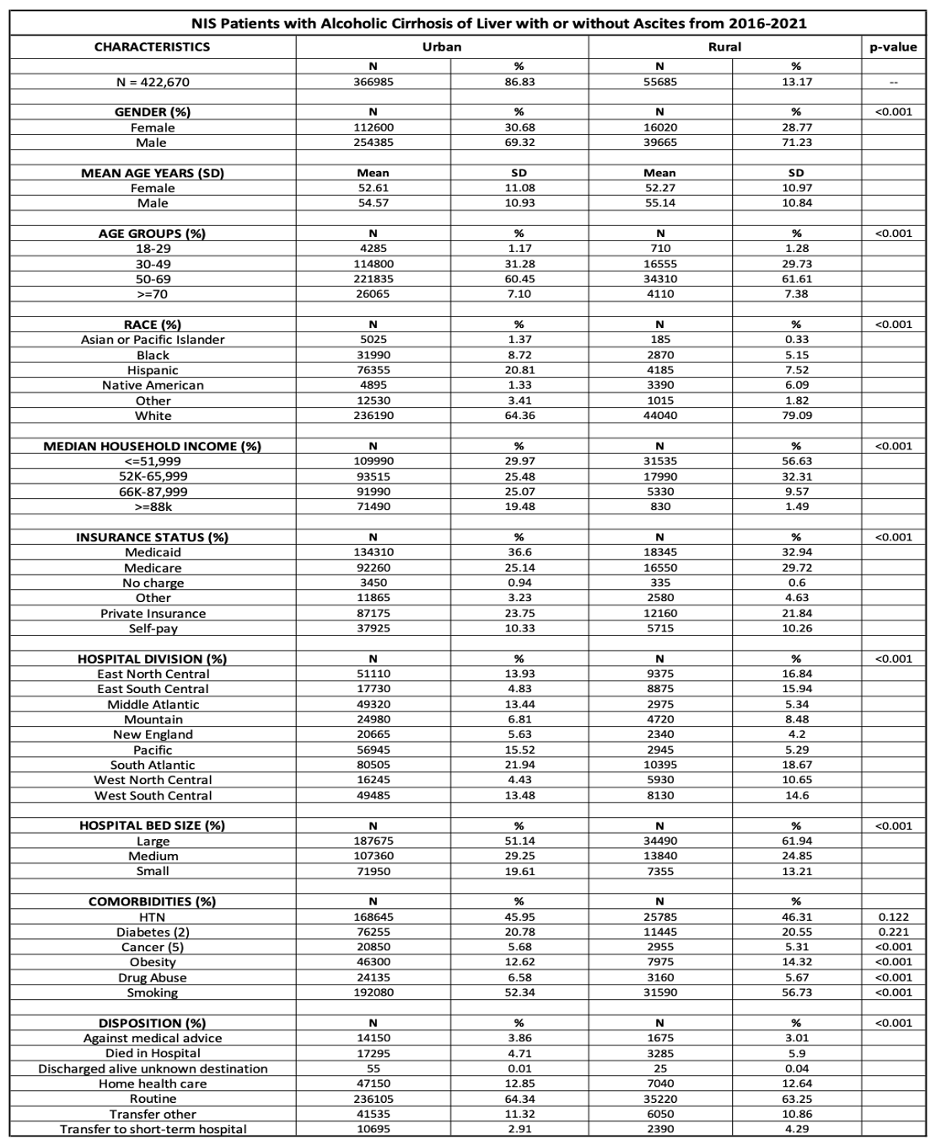
Figure: Table 1: Demographic characteristics of patients with alcoholic cirrhosis including gender, mean age years, age groups, race, median household income, insurance status, hospital division, hospital bed size, comorbidities and disposition in urban and rural settings.

Figure: Table 2: Inpatient outcomes of patients with alcoholic cirrhosis in urban and rural settings.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Niloy Ghosh indicated no relevant financial relationships.
Niven Wang indicated no relevant financial relationships.
Muhammad Nadeem indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Niloy Ghosh, MD1, Niven Wang, DO2, Muhammad A. Nadeem, MD3, Mohammed Quazi, PhD4, Amir Sohail, MD, MSc5, Abu Baker Sheikh, MD1. P3745 - A Comparative Analysis of Rural and Urban Disparities in Alcohol-Associated Cirrhosis Outcomes: Insights From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico Health Sciences Center, Albuquerque, NM; 2University of New Mexico Hospital, Albuquerque, NM; 3Cleveland Clinic, Cleveland, OH; 4West Virginia University, Morgantown, WV; 5University of New Mexico, Albuquerque, NM
Introduction: Rural-urban disparities in outcomes among patients with alcohol-associated liver disease (ALD) remain understudied at the national level. This study evaluated differences in inpatient outcomes, complications, and healthcare utilization among hospitalized adults with alcoholic cirrhosis across rural and urban populations in the United States.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2021), identifying adult hospitalizations with a primary diagnosis of alcoholic cirrhosis using ICD-10-CM codes. Rural-urban status was determined using patient residence data. Multivariable logistic and linear regression models were used to compare in-hospital mortality, complications, length of stay (LOS), and total hospitalization costs, adjusting for demographic, hospital-level, and clinical covariates.
Results: Among 422,670 hospitalizations for alcoholic cirrhosis, 13.2% were from rural areas. Rural patients were more likely to be older (mean age: 53.9 vs. 52.3 years), White (79.1% vs. 64.3%), from lower-income zip codes (household income ≤ $51,999: 56.6% vs. 30.0%), and have higher rates of smoking (56.7% vs. 52.3%) and obesity (14.3% vs. 12.6%) compared to urban patients. In-hospital mortality was significantly higher in rural patients (5.9% vs. 4.7%; adjusted odds ratio [aOR] 1.23, 95% CI: 1.12–1.34, p< 0.001). Rural patients also had increased odds of spontaneous bacterial peritonitis (aOR 1.19, 95% CI: 1.08–1.30) and variceal bleeding (aOR 1.18, 95% CI: 1.12–1.24). No significant differences were found in LOS or use of mechanical ventilation. Total hospitalization costs were significantly lower in rural patients ($64,690 vs. $82,236; p< 0.001).
Discussion: Rural patients hospitalized with alcoholic cirrhosis face higher risks of inpatient mortality and complications despite similar lengths of stay and lower hospitalization costs. These findings highlight persistent geographic disparities in cirrhosis care and underscore the need for targeted clinical and policy interventions in rural health systems. By leveraging a large, nationally representative dataset, this study adds important evidence on how rural residence is associated with worse inpatient outcomes in alcohol-associated liver disease, supporting the need for more equitable resource allocation and care models in hepatology.
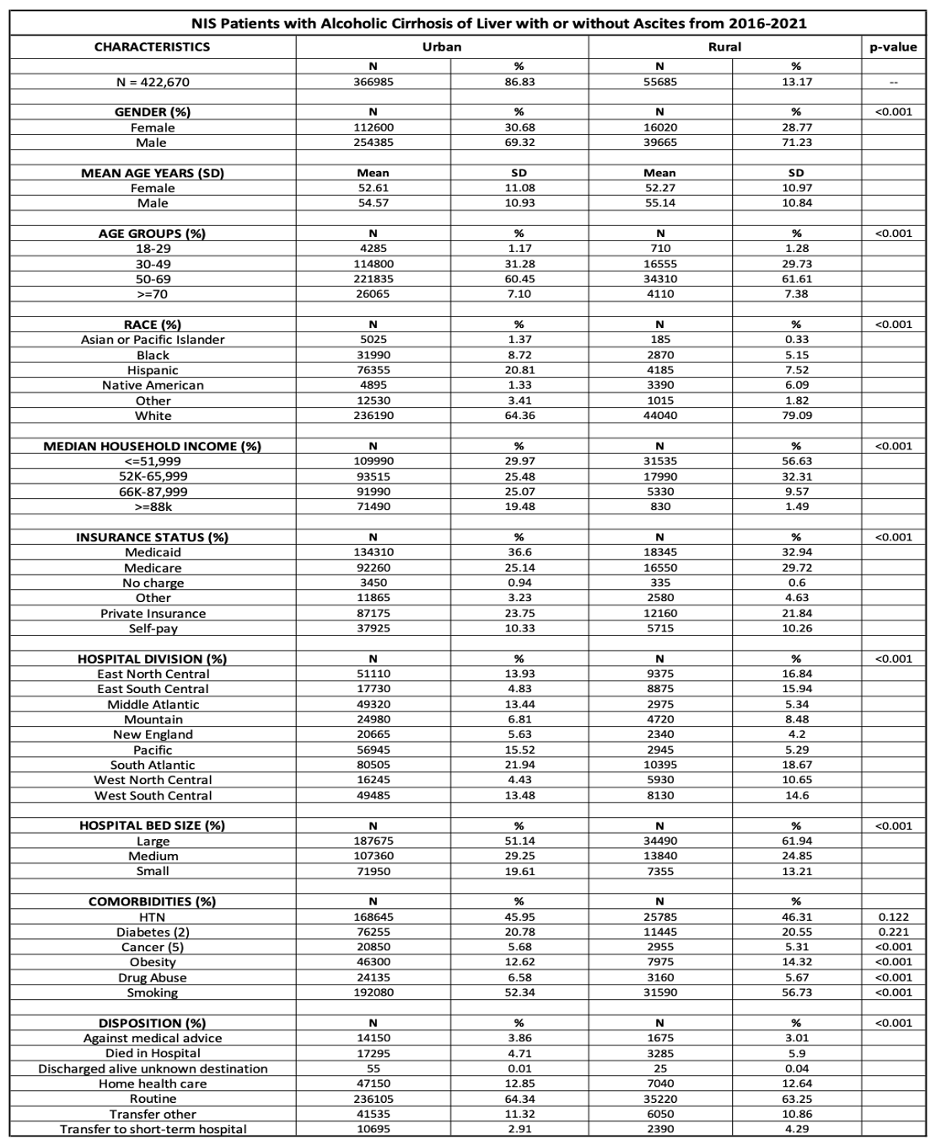
Figure: Table 1: Demographic characteristics of patients with alcoholic cirrhosis including gender, mean age years, age groups, race, median household income, insurance status, hospital division, hospital bed size, comorbidities and disposition in urban and rural settings.

Figure: Table 2: Inpatient outcomes of patients with alcoholic cirrhosis in urban and rural settings.
Disclosures:
Pooja Viswanath indicated no relevant financial relationships.
Niloy Ghosh indicated no relevant financial relationships.
Niven Wang indicated no relevant financial relationships.
Muhammad Nadeem indicated no relevant financial relationships.
Mohammed Quazi indicated no relevant financial relationships.
Amir Sohail indicated no relevant financial relationships.
Abu Baker Sheikh indicated no relevant financial relationships.
Pooja Viswanath, MS, DO1, Niloy Ghosh, MD1, Niven Wang, DO2, Muhammad A. Nadeem, MD3, Mohammed Quazi, PhD4, Amir Sohail, MD, MSc5, Abu Baker Sheikh, MD1. P3745 - A Comparative Analysis of Rural and Urban Disparities in Alcohol-Associated Cirrhosis Outcomes: Insights From the National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
