Monday Poster Session
Category: Liver
P3742 - Mortality Benefit of Statin Exposure in Patients With Metabolic Dysfunction-Associated Steatohepatitis Cirrhosis and Spontaneous Bacterial Peritonitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Karecia Byfield, MBBS
Jefferson Einstein Hospital
Philadelphia, PA
Presenting Author(s)
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Pojsakorn Danpanichkul, MD2, Laith Alomari, MD3, Danielle Lewis, MBBS4, Megan Johnson, MBBS5, Ghideon Ezaz, MD3
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Department of Internal Medicine, Texas Tech University Healt, Lubbock, TX; 3Thomas Jefferson University, Philadelphia, PA; 4Jefferson Einstein Philadelphia Hospital, Philadelphia, PA; 5Spanish Town Hospital, Kingston, Saint Catherine, Jamaica
Introduction: Spontaneous bacterial peritonitis (SBP) is a complication of decompensated cirrhosis, contributing significantly to the morbidity and mortality associated with chronic liver disease. Statins which have been previously used for cardiovascular disease risk reduction have emerged as a beneficial agent in cirrhosis given their anti-inflammatory properties. Motzkus-Feagans et al. demonstrated reduced infection risks among statin users in a cohort of U.S. Veterans with cirrhosis, suggesting that statins may offer protection against cirrhosis-related complications. While their role in preventing hepatic decompensation is increasingly recognized, a gap exists in the understanding of how statins influence outcomes in specific infections such as SBP. This study aims to address this gap by exploring the association between statin use and SBP-related mortality in patients with MASH cirrhosis.
Methods: Data from the US Collaborative Network-TriNetX was used to evaluate the impact of statins on patients aged 18 years and older with MASH cirrhosis hospitalized for SBP between January 1, 2013 and January 1, 2023 using relevant ICD-10 codes. Patients were divided into two cohorts: those with concurrent statin use, and those without. Both cohorts were propensity score matched based on demographics, comorbidities such as diabetes and hypertension and biochemical values such as serum albumin. They were followed for 30 days post-hospitalization to assess the primary outcome of mortality. Secondary outcomes included sepsis, shock and acute kidney injury (AKI).
Results: Each cohort consisted of 836 patients after propensity-score matching with similar characteristics. The mean age after matching was 66 ± 11 years with 51% being female. Our analysis found that within 30 days post-hospitalization, the cohort without concurrent statin exposure had a significantly higher odds of mortality (HR: 1.56, 95% CI: 1.22-2.00, P: 0.0004). There was no significant difference in the occurrence of sepsis, shock or AKI.
Discussion: Our study demonstrates a significant mortality benefit associated with concurrent statin exposure in patients with MASH cirrhosis hospitalized for SBP. Prior studies have primarily emphasized the role of statins in prevention of decompensated cirrhosis; however, our findings highlight that statins may also confer a survival advantage even after decompensation has occurred. Further longitudinal studies are needed to explore the therapeutic role of statins in decompensated cirrhosis.
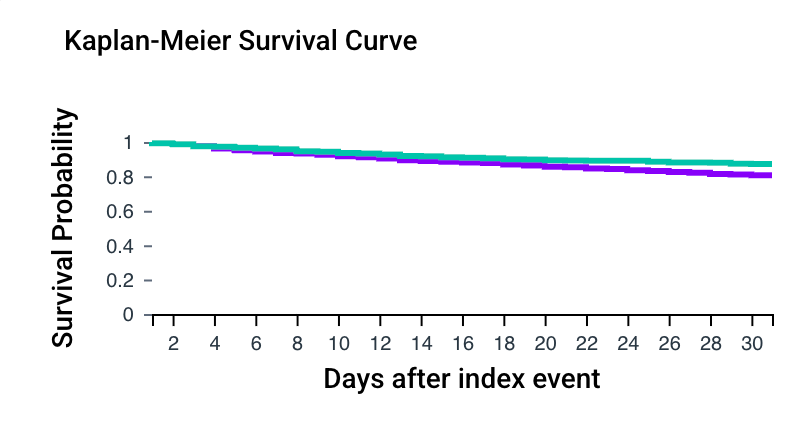
Figure: Kaplan-Meier Survival Curve Highlighting Survival Rate
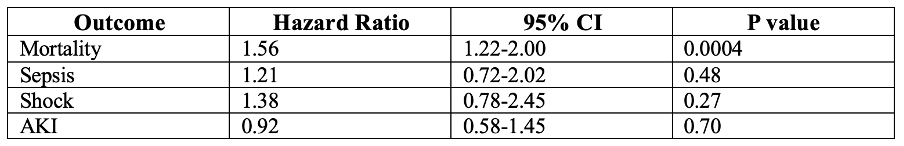
Figure: Table Showing Hazard Ratios of Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Danielle Lewis indicated no relevant financial relationships.
Megan Johnson indicated no relevant financial relationships.
Ghideon Ezaz indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Pojsakorn Danpanichkul, MD2, Laith Alomari, MD3, Danielle Lewis, MBBS4, Megan Johnson, MBBS5, Ghideon Ezaz, MD3. P3742 - Mortality Benefit of Statin Exposure in Patients With Metabolic Dysfunction-Associated Steatohepatitis Cirrhosis and Spontaneous Bacterial Peritonitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA; 2Department of Internal Medicine, Texas Tech University Healt, Lubbock, TX; 3Thomas Jefferson University, Philadelphia, PA; 4Jefferson Einstein Philadelphia Hospital, Philadelphia, PA; 5Spanish Town Hospital, Kingston, Saint Catherine, Jamaica
Introduction: Spontaneous bacterial peritonitis (SBP) is a complication of decompensated cirrhosis, contributing significantly to the morbidity and mortality associated with chronic liver disease. Statins which have been previously used for cardiovascular disease risk reduction have emerged as a beneficial agent in cirrhosis given their anti-inflammatory properties. Motzkus-Feagans et al. demonstrated reduced infection risks among statin users in a cohort of U.S. Veterans with cirrhosis, suggesting that statins may offer protection against cirrhosis-related complications. While their role in preventing hepatic decompensation is increasingly recognized, a gap exists in the understanding of how statins influence outcomes in specific infections such as SBP. This study aims to address this gap by exploring the association between statin use and SBP-related mortality in patients with MASH cirrhosis.
Methods: Data from the US Collaborative Network-TriNetX was used to evaluate the impact of statins on patients aged 18 years and older with MASH cirrhosis hospitalized for SBP between January 1, 2013 and January 1, 2023 using relevant ICD-10 codes. Patients were divided into two cohorts: those with concurrent statin use, and those without. Both cohorts were propensity score matched based on demographics, comorbidities such as diabetes and hypertension and biochemical values such as serum albumin. They were followed for 30 days post-hospitalization to assess the primary outcome of mortality. Secondary outcomes included sepsis, shock and acute kidney injury (AKI).
Results: Each cohort consisted of 836 patients after propensity-score matching with similar characteristics. The mean age after matching was 66 ± 11 years with 51% being female. Our analysis found that within 30 days post-hospitalization, the cohort without concurrent statin exposure had a significantly higher odds of mortality (HR: 1.56, 95% CI: 1.22-2.00, P: 0.0004). There was no significant difference in the occurrence of sepsis, shock or AKI.
Discussion: Our study demonstrates a significant mortality benefit associated with concurrent statin exposure in patients with MASH cirrhosis hospitalized for SBP. Prior studies have primarily emphasized the role of statins in prevention of decompensated cirrhosis; however, our findings highlight that statins may also confer a survival advantage even after decompensation has occurred. Further longitudinal studies are needed to explore the therapeutic role of statins in decompensated cirrhosis.
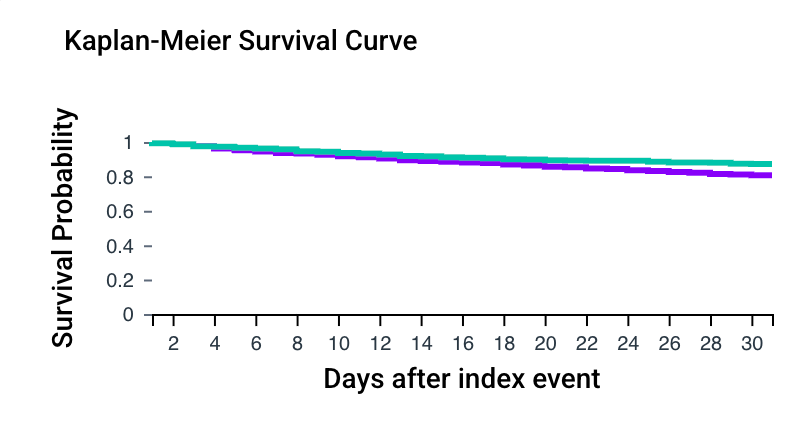
Figure: Kaplan-Meier Survival Curve Highlighting Survival Rate
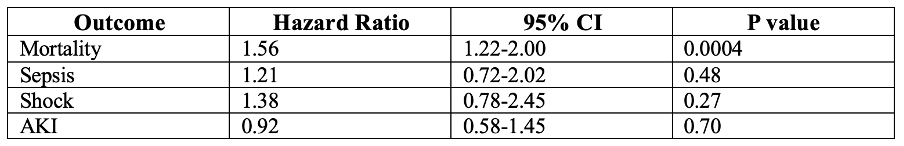
Figure: Table Showing Hazard Ratios of Clinical Outcomes
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Tinsae Anebo indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Danielle Lewis indicated no relevant financial relationships.
Megan Johnson indicated no relevant financial relationships.
Ghideon Ezaz indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Tinsae Anebo, MD1, Pojsakorn Danpanichkul, MD2, Laith Alomari, MD3, Danielle Lewis, MBBS4, Megan Johnson, MBBS5, Ghideon Ezaz, MD3. P3742 - Mortality Benefit of Statin Exposure in Patients With Metabolic Dysfunction-Associated Steatohepatitis Cirrhosis and Spontaneous Bacterial Peritonitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
