Monday Poster Session
Category: Liver
P3736 - Influence of Inflammatory Bowel Disease on In-Hospital Outcomes of Patients With Alcoholic Hepatitis: A Nationwide Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Raj H. Patel, MD
St. Mary Medical Center
Langhorne, PA
Presenting Author(s)
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Yash Shah, MD2, Bradley D. Confer, DO5, Harshit S. Khara, MD6
1St. Mary Medical Center, Langhorne, PA; 2Mercy Catholic Medical Center, Darby, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Geisinger Health System, Danville, PA; 6Geisinger Health System, Danville, NJ
Introduction: Alcoholic hepatitis (AH) is an advanced form of alcohol-related liver disease and presents with the sudden onset of jaundice and hepatic dysfunction. Recent data reveals rising trends in hospital admissions and resource utilization in patients with AH. Similarly, IBD, a chronic debilitating condition, imposes a significant burden on healthcare in today’s world. In this study, we aim to analyze outcomes of AH in patients with and without IBD with an emphasis on mortality trends, resource utilization, and related complications.
Methods: We used the National Inpatient Sample (NIS) database from 2016 to 2020 and identified adults ( > 18 years) hospitalized patients with AH. Patients were stratified into 2 cohorts based on the presence or absence of IBD. Propensity score matching was conducted to adjust for baseline characteristics. We used SAS 9.4 and performed a Chi-square test, t-test, along with multivariate logistic regression to analyze the effect of IBD on inpatient outcomes, including length of stay, inpatient mortality, and total hospital expenses (THC; inflation-adjusted to 2020 USD), as well as other secondary outcomes.
Results: A total of 9,880 patients with alcoholic hepatitis (AH) were stratified into 2 groups: those with IBD (n=4,940; mean age 46.9 years; 40.6% female) and those without IBD (n=4,940; mean age 47.7 years; 59.4% female). Patients with IBD had longer hospital stays (6.68 vs. 6.13 days, p < 0.05) and higher THC (mean $17,180 vs. $15,181, p < 0.05). Inpatient mortality was higher among patients with IBD but did not reach statistical significance (4.8% vs. 4.0%; p=0.0861).
IBD was associated with significantly higher complications, including septic shock (6.2% vs. 3.7%; p< 0.0001), septicemia (15.1% vs. 11.3%; p< 0.0001), and thrombocytopenia (21.5% vs. 19.4%; p=0.0126). In reverse, the incidence of peritonitis was lower in the IBD group (2.3% vs. 3.5%; p=0.0003). SBP (1.6% vs. 2.6%; p=0.0005) was also less common in IBD patients. AKI (16.8% vs. 18.7%; p=0.0124) was lower in the IBD cohort, while HRS and ascites showed no significant differences. Predictors of mortality included Native American ethnicity, age > 64 years, individuals in the upper 25th income quartile, and the presence of AKI or thrombocytopenia.
Discussion: Based on our analysis, IBD in AH is associated with increased healthcare costs, longer hospital stays, and worse clinical outcomes. Targeted interventions are required to improve the outcomes in concurrent AH and IBD.
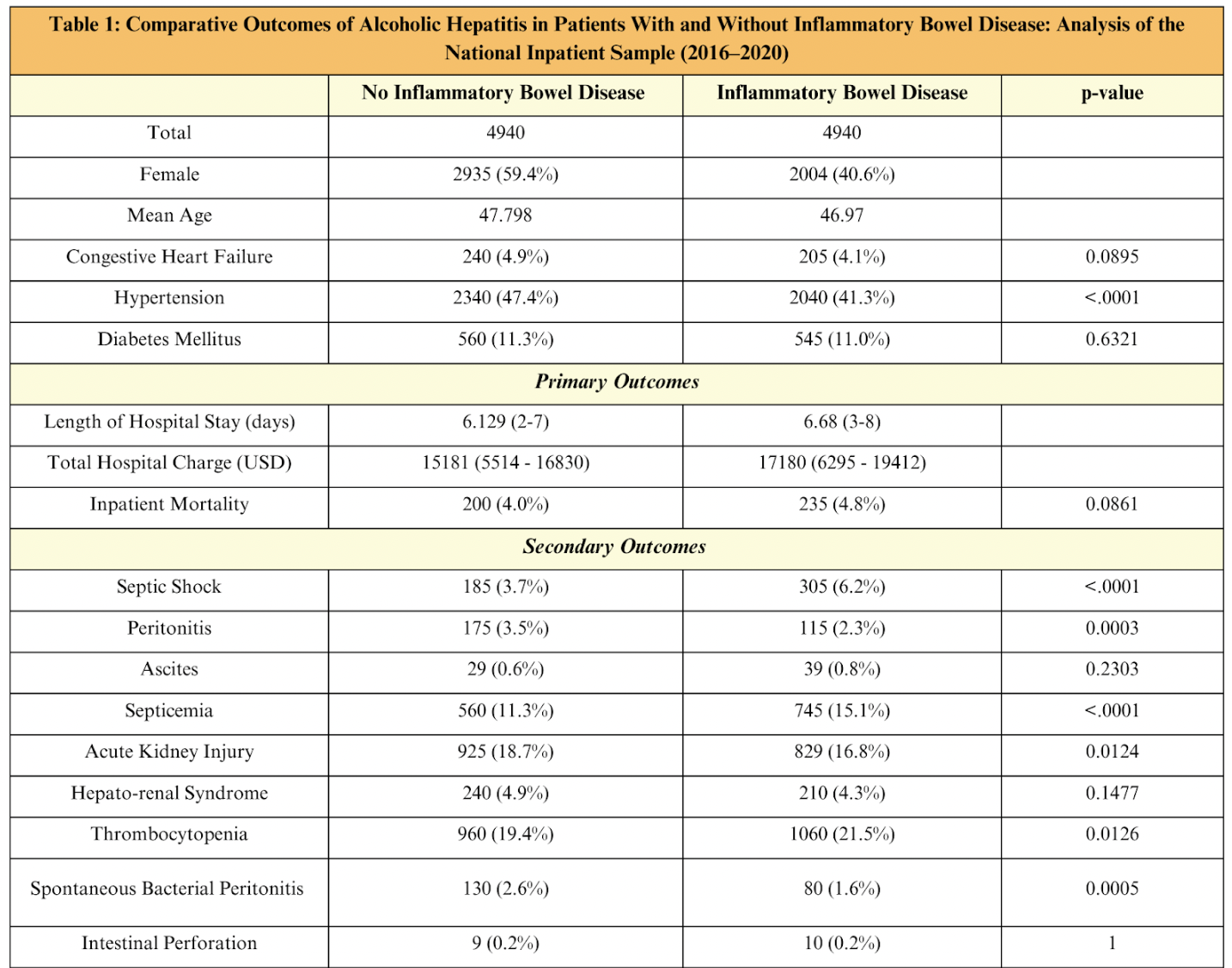
Figure: Comparative Outcomes of Alcoholic Hepatitis in Patients with and without IBD
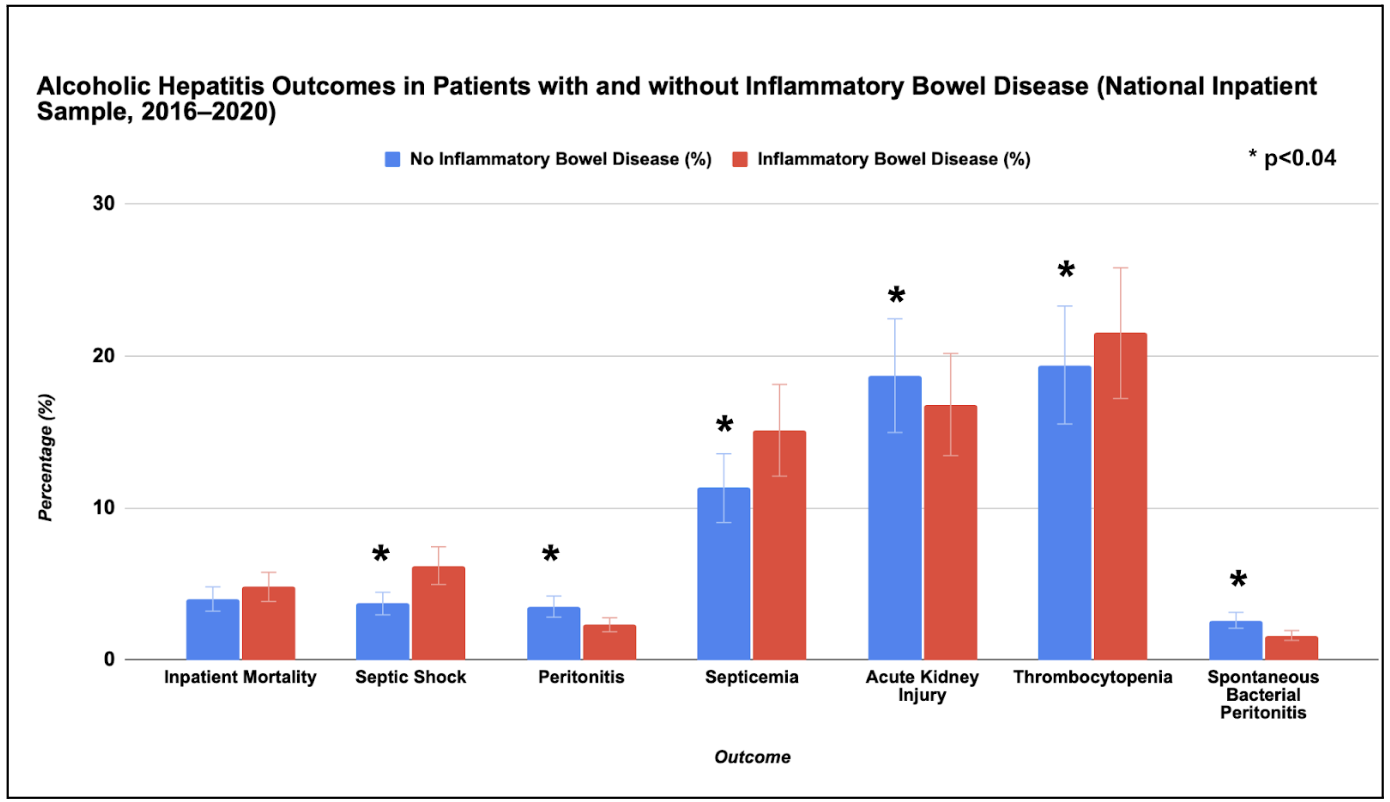
Figure: Alcoholic Hepatitis Outcomes in Patients with and without IBD (Graphical comparison)
Disclosures:
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Yash Shah, MD2, Bradley D. Confer, DO5, Harshit S. Khara, MD6. P3736 - Influence of Inflammatory Bowel Disease on In-Hospital Outcomes of Patients With Alcoholic Hepatitis: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Mary Medical Center, Langhorne, PA; 2Mercy Catholic Medical Center, Darby, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Geisinger Health System, Danville, PA; 6Geisinger Health System, Danville, NJ
Introduction: Alcoholic hepatitis (AH) is an advanced form of alcohol-related liver disease and presents with the sudden onset of jaundice and hepatic dysfunction. Recent data reveals rising trends in hospital admissions and resource utilization in patients with AH. Similarly, IBD, a chronic debilitating condition, imposes a significant burden on healthcare in today’s world. In this study, we aim to analyze outcomes of AH in patients with and without IBD with an emphasis on mortality trends, resource utilization, and related complications.
Methods: We used the National Inpatient Sample (NIS) database from 2016 to 2020 and identified adults ( > 18 years) hospitalized patients with AH. Patients were stratified into 2 cohorts based on the presence or absence of IBD. Propensity score matching was conducted to adjust for baseline characteristics. We used SAS 9.4 and performed a Chi-square test, t-test, along with multivariate logistic regression to analyze the effect of IBD on inpatient outcomes, including length of stay, inpatient mortality, and total hospital expenses (THC; inflation-adjusted to 2020 USD), as well as other secondary outcomes.
Results: A total of 9,880 patients with alcoholic hepatitis (AH) were stratified into 2 groups: those with IBD (n=4,940; mean age 46.9 years; 40.6% female) and those without IBD (n=4,940; mean age 47.7 years; 59.4% female). Patients with IBD had longer hospital stays (6.68 vs. 6.13 days, p < 0.05) and higher THC (mean $17,180 vs. $15,181, p < 0.05). Inpatient mortality was higher among patients with IBD but did not reach statistical significance (4.8% vs. 4.0%; p=0.0861).
IBD was associated with significantly higher complications, including septic shock (6.2% vs. 3.7%; p< 0.0001), septicemia (15.1% vs. 11.3%; p< 0.0001), and thrombocytopenia (21.5% vs. 19.4%; p=0.0126). In reverse, the incidence of peritonitis was lower in the IBD group (2.3% vs. 3.5%; p=0.0003). SBP (1.6% vs. 2.6%; p=0.0005) was also less common in IBD patients. AKI (16.8% vs. 18.7%; p=0.0124) was lower in the IBD cohort, while HRS and ascites showed no significant differences. Predictors of mortality included Native American ethnicity, age > 64 years, individuals in the upper 25th income quartile, and the presence of AKI or thrombocytopenia.
Discussion: Based on our analysis, IBD in AH is associated with increased healthcare costs, longer hospital stays, and worse clinical outcomes. Targeted interventions are required to improve the outcomes in concurrent AH and IBD.
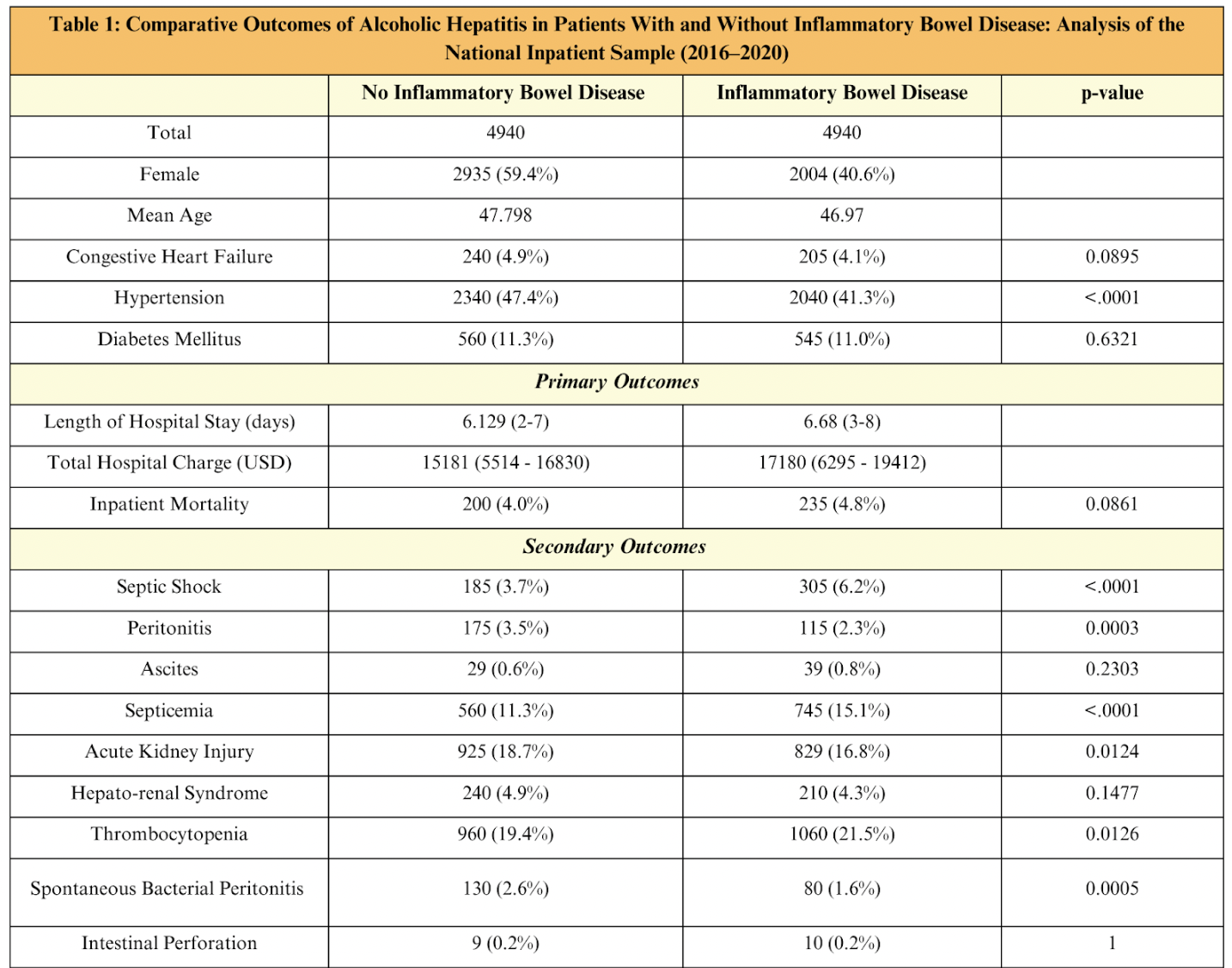
Figure: Comparative Outcomes of Alcoholic Hepatitis in Patients with and without IBD
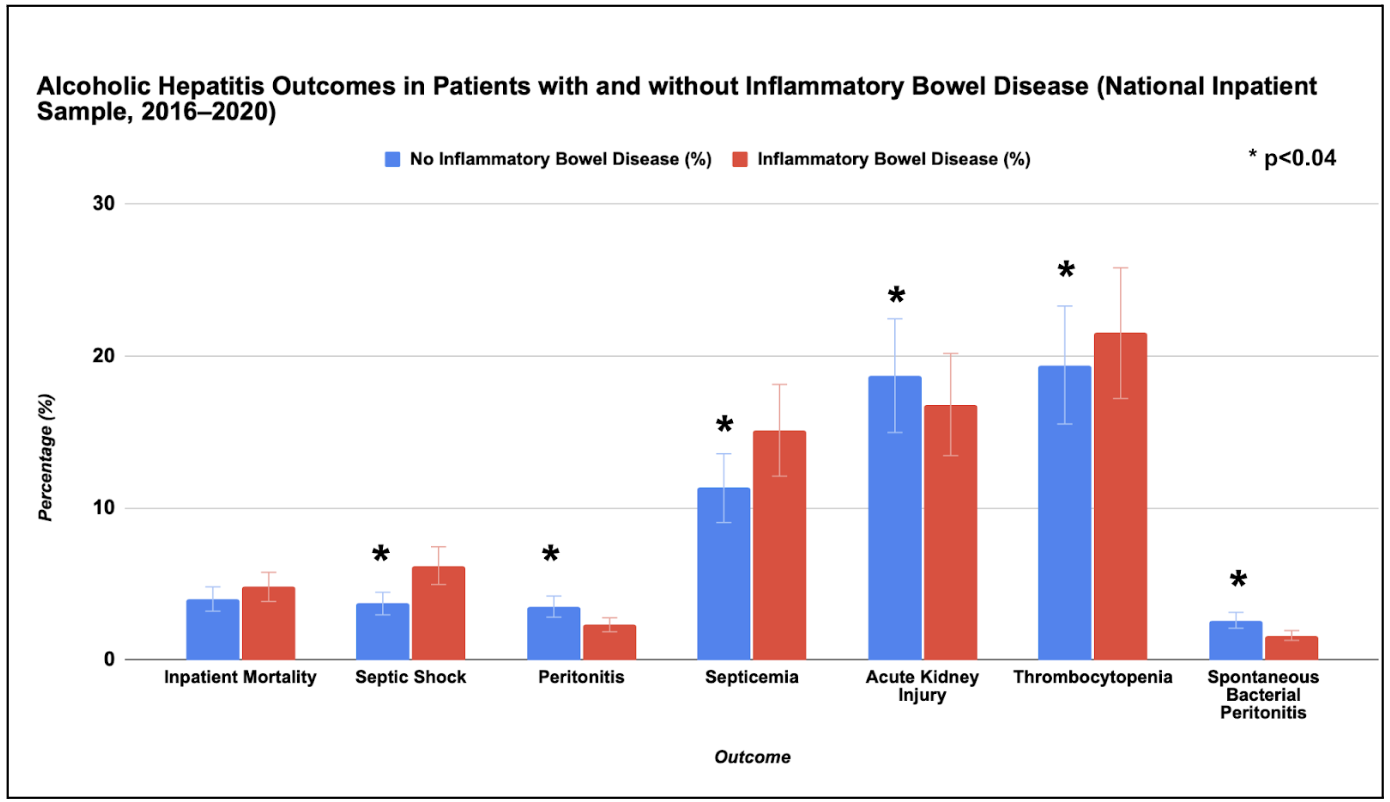
Figure: Alcoholic Hepatitis Outcomes in Patients with and without IBD (Graphical comparison)
Disclosures:
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Pranav Patel, MD5, Yash Shah, MD2, Bradley D. Confer, DO5, Harshit S. Khara, MD6. P3736 - Influence of Inflammatory Bowel Disease on In-Hospital Outcomes of Patients With Alcoholic Hepatitis: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
