Monday Poster Session
Category: Liver
P3734 - Association of NAFLD Severity With Major Adverse Cardiovascular Events: A Meta-Analysis of Cohort Studies
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abubakar Gapizov, MD, MBA (he/him/his)
NewYork-Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Abubakar Gapizov, MD, MBA1, Bhavna Singla, MD2, Shivam Singla, MBBS, MD3, Saad Manzoor, MBBS4, Muhammad Subhan, MBBS, MD5, Minhal Chaudhry, MBBS6, Maria Fatima, MD7
1NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2Erie County Medical Center/ Apogee Physician, Buffalo, NY; 3Tidal Health Peninsula Regional, Salisbury, MD, Salisbury, MD; 4Lahore Medical and Dental College, Lahore, Punjab, Pakistan; 5Allama Iqbal Medical College Lahore, Lahore, Punjab, Pakistan; 6King Edward Medical University, Lahore, Pakistan, Pittsburgh, PA; 7Wayne State University School of Medicine /John D. Dingell VA Medical Center, Southfield, MI
Introduction: Non-alcoholic fatty liver disease (NAFLD), a primary hepatic manifestation of metabolic syndrome, is now recognized as a significant contributor to cardiovascular disease burden. It is unclear whether advanced NAFLD severity independently predicts major adverse cardiovascular events (MACE) because severity has not been consistently defined, and few considered potential confounding factors.
Methods: Following the PRISMA 2020 guidelines, we looked through the Cochrane Library, Web of Science, Embase, and PubMed till January 2025 for longitudinal cohort studies assessing MACE incidence according to NAFLD severity. Eligible studies included adults with biopsy-verified (NASH or fibrosis ≥F2) or imaging-verified (MRI-PDFF ≥10% or CAP ≥280 dB/m) NAFLD and stratified as mild vs moderate/severe, with an average follow-up of 1 year or greater. Two reviewers separately conducted the data extraction and assessed for bias using the Newcastle-Ottawa Scale. 95% confidence intervals (CI) and pooled risk ratios (RR) were determined using a random-effects model. Heterogeneity (I²) and small-study effects (Egger's test) were assessed. Sensitivity analyses were performed to exclude studies at high risk of bias.
Results: Three cohort studies met inclusion criteria for MACE outcomes (N=136,789; mean age: 52–58; duration: 5.2–8.1 years). One study on advanced (F3 – F4/NASH) and mild (F0 – F1/steatosis) NAFLD calculated a fully adjusted RR of 1.50 (95% CI 0.97–2.32; p=0.07), indicating a trend towards greater MACE risk. The pooled RR for NAFLD, compared to no NAFLD, was 1.19 (95% CI 0.80 - 1.79; I²=94%) with sensitivity analysis RR (95% CI) 1.12 (0.85 - 1.48). There is a pooled RR for MACE among NAFLD cases across all severity strata of 1.26 (95% CI 0.92 - 1.73; I²=88%). Egger's test did not report evidence of publication bias (p=0.34). Only one study controlled for diabetes and dyslipidemia, and none for visceral adiposity.
Discussion: This meta-analysis suggests that histologically or imaging-defined advanced NAFLD may be associated with a clinically meaningful but statistically insignificant increased risk of MACE. Substantial heterogeneity and residual confounding affect definitive interpretations. Future studies should employ standardized severity cutoffs (such as MRI-PDFF ≥10% or fibrosis stage ≥F2), adjust for cardiometabolic risk factors, and distinguish the atherosclerotic and non-atherosclerotic MACE components to strengthen the prediction of cardiovascular risk in NAFLD.
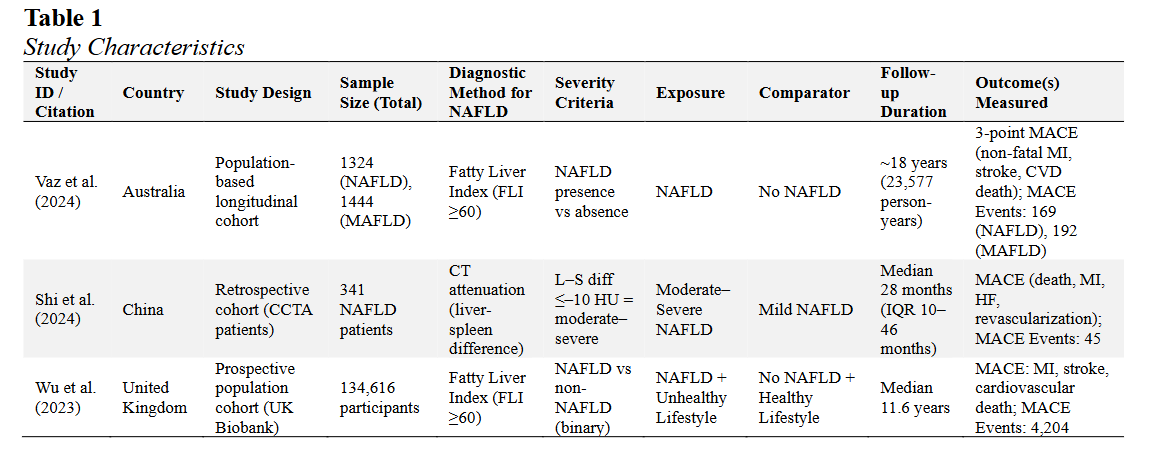
Figure: Characteristic Summary of Selected Studies
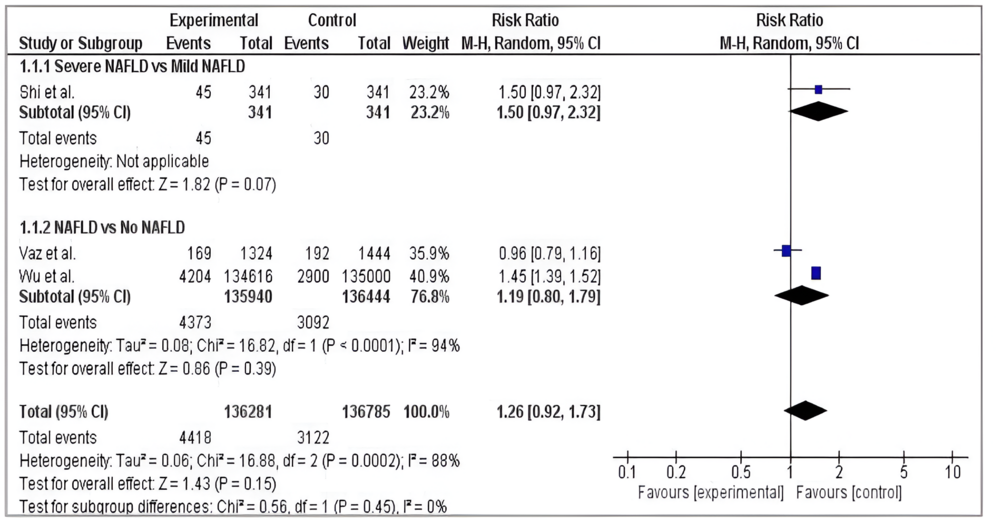
Figure: Forest Plot of MACE Risk Associated with NAFLD Severity and Presence
Disclosures:
Abubakar Gapizov indicated no relevant financial relationships.
Bhavna Singla indicated no relevant financial relationships.
Shivam Singla indicated no relevant financial relationships.
Saad Manzoor indicated no relevant financial relationships.
Muhammad Subhan indicated no relevant financial relationships.
Minhal Chaudhry indicated no relevant financial relationships.
Maria Fatima indicated no relevant financial relationships.
Abubakar Gapizov, MD, MBA1, Bhavna Singla, MD2, Shivam Singla, MBBS, MD3, Saad Manzoor, MBBS4, Muhammad Subhan, MBBS, MD5, Minhal Chaudhry, MBBS6, Maria Fatima, MD7. P3734 - Association of NAFLD Severity With Major Adverse Cardiovascular Events: A Meta-Analysis of Cohort Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2Erie County Medical Center/ Apogee Physician, Buffalo, NY; 3Tidal Health Peninsula Regional, Salisbury, MD, Salisbury, MD; 4Lahore Medical and Dental College, Lahore, Punjab, Pakistan; 5Allama Iqbal Medical College Lahore, Lahore, Punjab, Pakistan; 6King Edward Medical University, Lahore, Pakistan, Pittsburgh, PA; 7Wayne State University School of Medicine /John D. Dingell VA Medical Center, Southfield, MI
Introduction: Non-alcoholic fatty liver disease (NAFLD), a primary hepatic manifestation of metabolic syndrome, is now recognized as a significant contributor to cardiovascular disease burden. It is unclear whether advanced NAFLD severity independently predicts major adverse cardiovascular events (MACE) because severity has not been consistently defined, and few considered potential confounding factors.
Methods: Following the PRISMA 2020 guidelines, we looked through the Cochrane Library, Web of Science, Embase, and PubMed till January 2025 for longitudinal cohort studies assessing MACE incidence according to NAFLD severity. Eligible studies included adults with biopsy-verified (NASH or fibrosis ≥F2) or imaging-verified (MRI-PDFF ≥10% or CAP ≥280 dB/m) NAFLD and stratified as mild vs moderate/severe, with an average follow-up of 1 year or greater. Two reviewers separately conducted the data extraction and assessed for bias using the Newcastle-Ottawa Scale. 95% confidence intervals (CI) and pooled risk ratios (RR) were determined using a random-effects model. Heterogeneity (I²) and small-study effects (Egger's test) were assessed. Sensitivity analyses were performed to exclude studies at high risk of bias.
Results: Three cohort studies met inclusion criteria for MACE outcomes (N=136,789; mean age: 52–58; duration: 5.2–8.1 years). One study on advanced (F3 – F4/NASH) and mild (F0 – F1/steatosis) NAFLD calculated a fully adjusted RR of 1.50 (95% CI 0.97–2.32; p=0.07), indicating a trend towards greater MACE risk. The pooled RR for NAFLD, compared to no NAFLD, was 1.19 (95% CI 0.80 - 1.79; I²=94%) with sensitivity analysis RR (95% CI) 1.12 (0.85 - 1.48). There is a pooled RR for MACE among NAFLD cases across all severity strata of 1.26 (95% CI 0.92 - 1.73; I²=88%). Egger's test did not report evidence of publication bias (p=0.34). Only one study controlled for diabetes and dyslipidemia, and none for visceral adiposity.
Discussion: This meta-analysis suggests that histologically or imaging-defined advanced NAFLD may be associated with a clinically meaningful but statistically insignificant increased risk of MACE. Substantial heterogeneity and residual confounding affect definitive interpretations. Future studies should employ standardized severity cutoffs (such as MRI-PDFF ≥10% or fibrosis stage ≥F2), adjust for cardiometabolic risk factors, and distinguish the atherosclerotic and non-atherosclerotic MACE components to strengthen the prediction of cardiovascular risk in NAFLD.
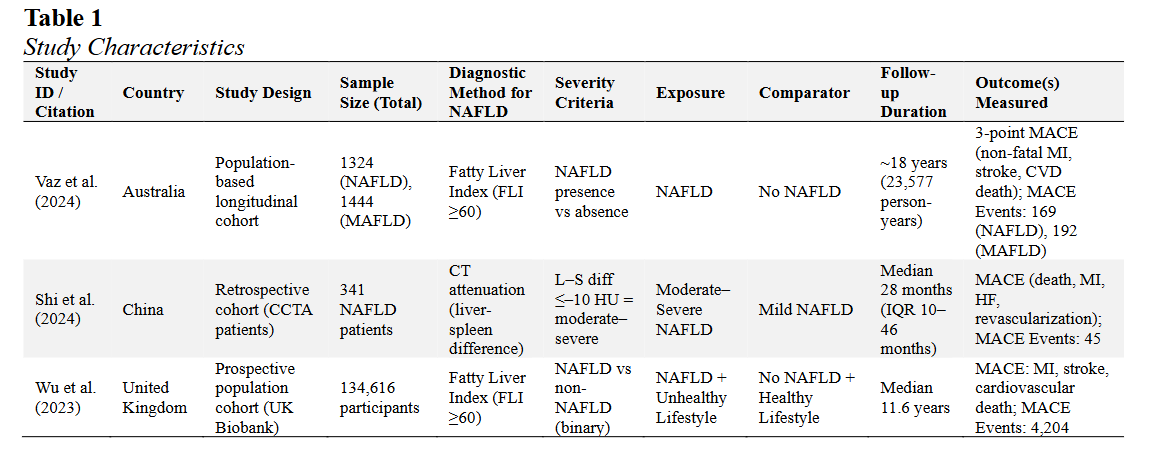
Figure: Characteristic Summary of Selected Studies
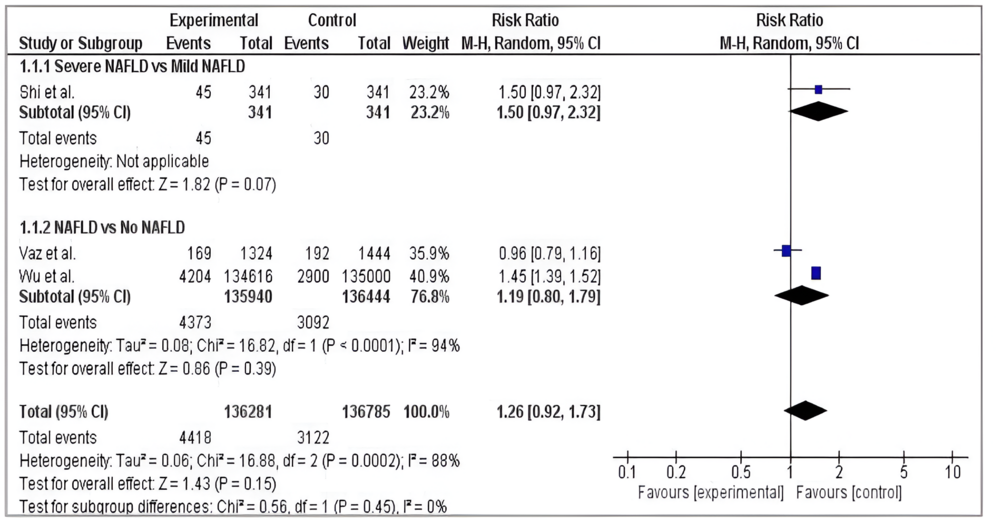
Figure: Forest Plot of MACE Risk Associated with NAFLD Severity and Presence
Disclosures:
Abubakar Gapizov indicated no relevant financial relationships.
Bhavna Singla indicated no relevant financial relationships.
Shivam Singla indicated no relevant financial relationships.
Saad Manzoor indicated no relevant financial relationships.
Muhammad Subhan indicated no relevant financial relationships.
Minhal Chaudhry indicated no relevant financial relationships.
Maria Fatima indicated no relevant financial relationships.
Abubakar Gapizov, MD, MBA1, Bhavna Singla, MD2, Shivam Singla, MBBS, MD3, Saad Manzoor, MBBS4, Muhammad Subhan, MBBS, MD5, Minhal Chaudhry, MBBS6, Maria Fatima, MD7. P3734 - Association of NAFLD Severity With Major Adverse Cardiovascular Events: A Meta-Analysis of Cohort Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
