Monday Poster Session
Category: Liver
P3731 - Exploring Racial and Socioeconomic Disparities in Liver Transplantation for Decompensated Cirrhosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sarah Meribout, MD
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1
1Maimonides Medical Center, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, Brooklyn, NY; 3Jijel University, Jijel, Constantine, Algeria
Introduction: Liver transplantation is the gold standard for decompensated cirrhosis, yet access remains inequitable. Studies suggest racial and socioeconomic disparities, but detailed exploration of these factors among patients hospitalized for decompensated cirrhosis is limited. Understanding these gaps is vital to promoting equitable care.
Methods: Using the National Inpatient Sample (NIS) database (2016–2019), we identified patients admitted for decompensated cirrhosis, excluding those with malignancy or missing data, resulting in a cohort of 830,005 patients. Of these, 2,425 received liver transplants during hospitalization. We analyzed baseline demographics, hospital characteristics, length of stay (LOS), and costs by race. Multivariable logistic regression, adjusted for socioeconomic factors, hospital characteristics, comorbidities, and cirrhosis etiology, was used to determine the impact of race and socioeconomic status on transplant likelihood.
Results: The mean age of transplant recipients varied significantly by race, with Native American patients being the youngest (52.6 years) and Asian/Pacific Islanders the oldest (60.91 years) (p< 0.001). Women were less likely to receive transplants compared to men across all racial groups (p< 0.001). White patients had the highest proportion of private insurance (26.3%), while Medicaid coverage was most common among Black (21.1%) and Hispanic (23.8%) patients. Regional variations existed, with the Midwest demonstrating lower odds (aOR 0.84, p=0.015) compared to the Northeast.
Socioeconomic status was a significant predictor, with patients from the highest income quartile being 45% more likely to receive a transplant than those from the lowest quartile (aOR 1.45, p< 0.001). Hispanic patients were more likely to receive transplants than Whites (aOR 1.23, p< 0.001), while Native American patients had lower odds (aOR 0.62, p=0.037). Despite adjustments, Black patients trended towards lower likelihood, but results did not reach statistical significance (aOR 0.86, p=0.059).
Discussion: Disparities in liver transplantation for decompensated cirrhosis are driven by a complex interplay of racial, socioeconomic, and regional factors. The finding that Hispanic patients had higher odds of transplantation, while Native Americans and potentially Black patients were disadvantaged, warrants further investigation. Addressing these inequities requires targeted policy reforms and public health interventions to address systemic barriers.
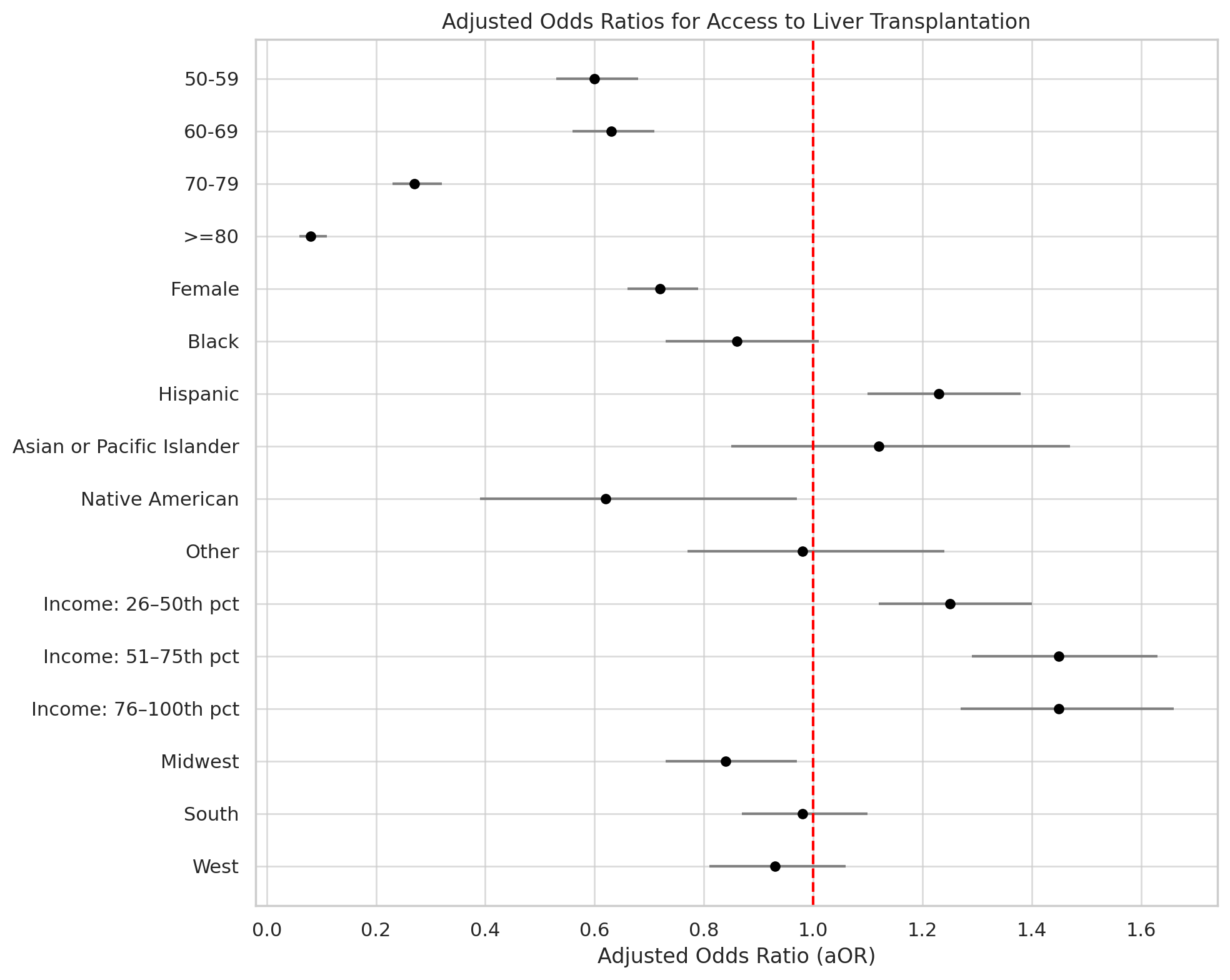
Figure: Table 1. Demographic, Socioeconomic, and Clinical Characteristics of Liver Transplant Candidates with Decompensated Cirrhosis Across Racial Groups
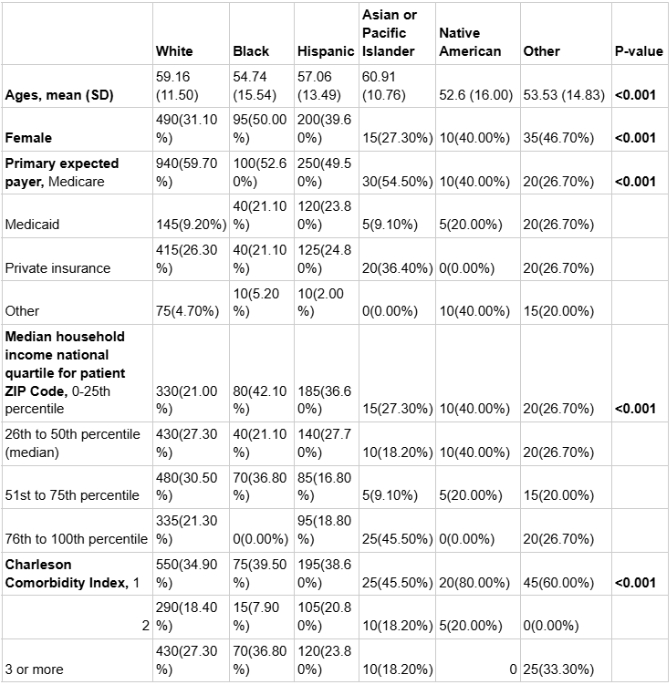
Figure: Figure 1. Forest plot of adjusted odds ratios (aORs) for access to liver transplantation.
Disclosures:
Sarah Meribout indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Anis Meribout indicated no relevant financial relationships.
Saida Benmostefa indicated no relevant financial relationships.
Ovanes Karslyan indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1. P3731 - Exploring Racial and Socioeconomic Disparities in Liver Transplantation for Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Icahn School of Medicine at Mount Sinai, Brooklyn, NY; 3Jijel University, Jijel, Constantine, Algeria
Introduction: Liver transplantation is the gold standard for decompensated cirrhosis, yet access remains inequitable. Studies suggest racial and socioeconomic disparities, but detailed exploration of these factors among patients hospitalized for decompensated cirrhosis is limited. Understanding these gaps is vital to promoting equitable care.
Methods: Using the National Inpatient Sample (NIS) database (2016–2019), we identified patients admitted for decompensated cirrhosis, excluding those with malignancy or missing data, resulting in a cohort of 830,005 patients. Of these, 2,425 received liver transplants during hospitalization. We analyzed baseline demographics, hospital characteristics, length of stay (LOS), and costs by race. Multivariable logistic regression, adjusted for socioeconomic factors, hospital characteristics, comorbidities, and cirrhosis etiology, was used to determine the impact of race and socioeconomic status on transplant likelihood.
Results: The mean age of transplant recipients varied significantly by race, with Native American patients being the youngest (52.6 years) and Asian/Pacific Islanders the oldest (60.91 years) (p< 0.001). Women were less likely to receive transplants compared to men across all racial groups (p< 0.001). White patients had the highest proportion of private insurance (26.3%), while Medicaid coverage was most common among Black (21.1%) and Hispanic (23.8%) patients. Regional variations existed, with the Midwest demonstrating lower odds (aOR 0.84, p=0.015) compared to the Northeast.
Socioeconomic status was a significant predictor, with patients from the highest income quartile being 45% more likely to receive a transplant than those from the lowest quartile (aOR 1.45, p< 0.001). Hispanic patients were more likely to receive transplants than Whites (aOR 1.23, p< 0.001), while Native American patients had lower odds (aOR 0.62, p=0.037). Despite adjustments, Black patients trended towards lower likelihood, but results did not reach statistical significance (aOR 0.86, p=0.059).
Discussion: Disparities in liver transplantation for decompensated cirrhosis are driven by a complex interplay of racial, socioeconomic, and regional factors. The finding that Hispanic patients had higher odds of transplantation, while Native Americans and potentially Black patients were disadvantaged, warrants further investigation. Addressing these inequities requires targeted policy reforms and public health interventions to address systemic barriers.
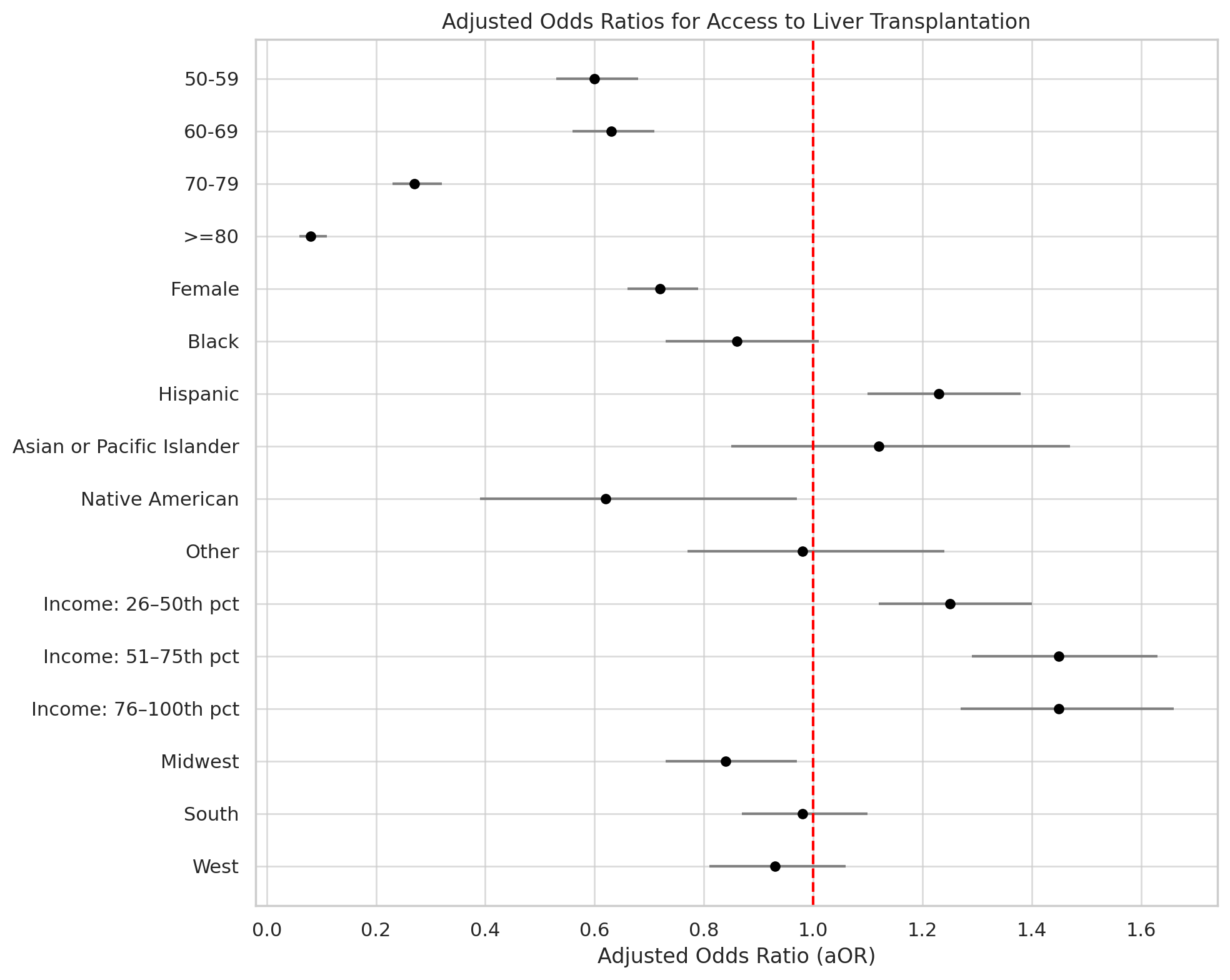
Figure: Table 1. Demographic, Socioeconomic, and Clinical Characteristics of Liver Transplant Candidates with Decompensated Cirrhosis Across Racial Groups
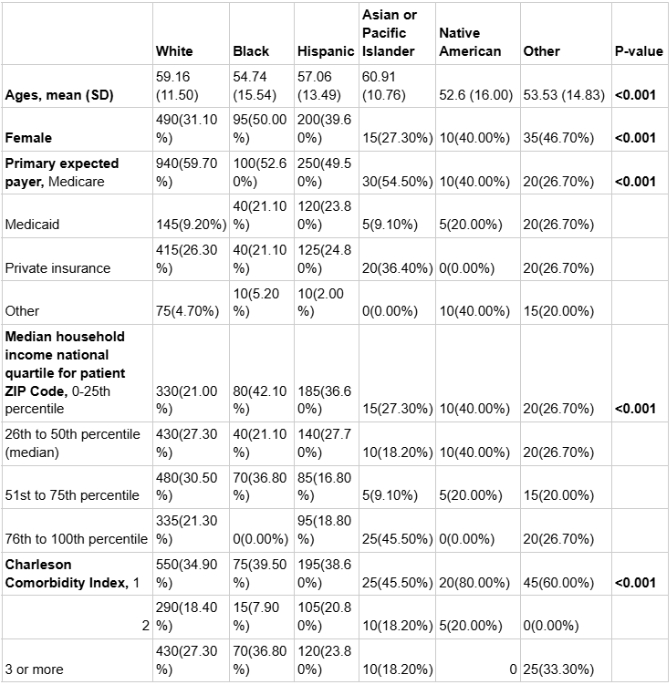
Figure: Figure 1. Forest plot of adjusted odds ratios (aORs) for access to liver transplantation.
Disclosures:
Sarah Meribout indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Anis Meribout indicated no relevant financial relationships.
Saida Benmostefa indicated no relevant financial relationships.
Ovanes Karslyan indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Sarah Meribout, MD1, Ahmed Salem, MD1, Anis Meribout, MD2, Saida Benmostefa, MS3, Ovanes Karslyan, MD1, Fatima Khan, MD1, Nakul Mahajan, MBBS1, Yasutoshi Shiratori, MD1. P3731 - Exploring Racial and Socioeconomic Disparities in Liver Transplantation for Decompensated Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
