Monday Poster Session
Category: Liver
P3727 - Prevalence and Outcomes of Eating Disorders in Patients With Metabolic-Associated Steatotic Liver Disease Following Introduction of DSM V
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Alexander Malik, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Alexander Malik, MD1, Thai Hau Koo, MD2, Morgan R. Starkey, MD3, Adrian S. Lindsey, MD1
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3MetroHealth Medical Center, Cleveland, OH
Introduction: Previous studies have shown a potential link between MASLD and eating disorders (EDs), which include binge eating disorder (BED), anorexia nervosa (AN), and bulimia nervosa (BN). We aimed to assess the prevalence and outcomes associated with EDs in patients with MASLD.
Methods: We conducted a retrospective cohort study using de-identified patient data from the global TriNetX database (2013–2025; since DSM-5 was introduced in May 2013), including all adults (≥18 years) with MASLD. Data were collected from 134 healthcare organizations in 14 different countries. Cohorts with MASLD with/without any ED (AN, BN, BED) and a control cohort (without MASLD) were created. Propensity score matching (1:1) was used to adjust for demographic and confounding variables. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of mortality and hepatic decompensation (ascites, hepatic encephalopathy [HE], and variceal hemorrhage (VH)) within 3, 6, and 12 months. Subgroup analyses were assessed by ED subtypes.
Results: Among the 1,303,113 adults with MASLD, 2,176 (0.17%) had a coexisting diagnosis of ED. BED was the most common (75%), followed by BN (12%) and AN (8%). Compared to those without EDs, MASLD patients with EDs were younger (46 vs. 58 years, p< 0.0001), more likely to be female (75% vs. 53%, p< 0.0001), and had higher mean BMIs (39 vs. 32.9, p< 0.0001). Patients with ED also had higher rates of mood and anxiety disorders (p< 0.0001). Following PSM, patients with MASLD and any ED had significantly lower odds of HE (OR 0.579, 95% CI, 0.370–0.905; p=0.015) and mortality (OR 0.689, 95% CI, 0.460–1.031; p=0.049). BED use was independently associated with lower mortality (OR 0.363, p=0.0008) and HE (OR 0.411, p=0.003). There were no statistically significant differences in ascites or VH between matched cohorts. Notably, the incidence of BED in patients with MASLD more than doubled following the COVID-19 pandemic (0.06% to 0.13%), with the largest increase among younger adults and females.
Discussion: Contrary to our initial hypothesis, patients with MASLD and comorbid EDs did not experience higher rates of adverse hepatic outcomes. Instead, several ED subgroups had significantly lower rates of HE and mortality than those without EDs. These findings may reflect earlier diagnosis, more frequent healthcare engagement, or differential treatment access among patients with EDs, especially those already receiving psychiatric or weight management care.
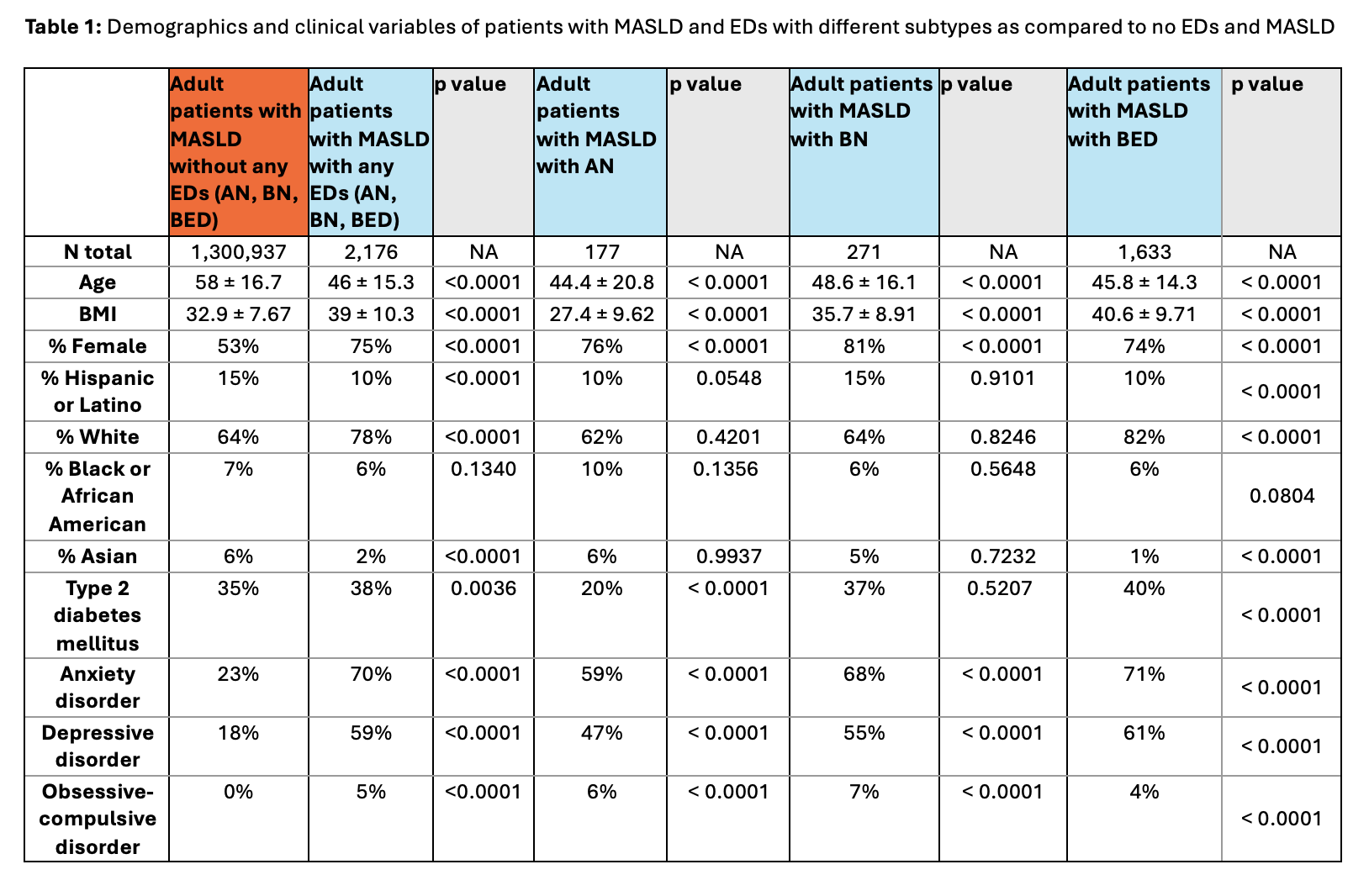
Figure: Table 1: Demographics and clinical variables of patients with MASLD and EDs with different subtypes as compared to no EDs and MASLD
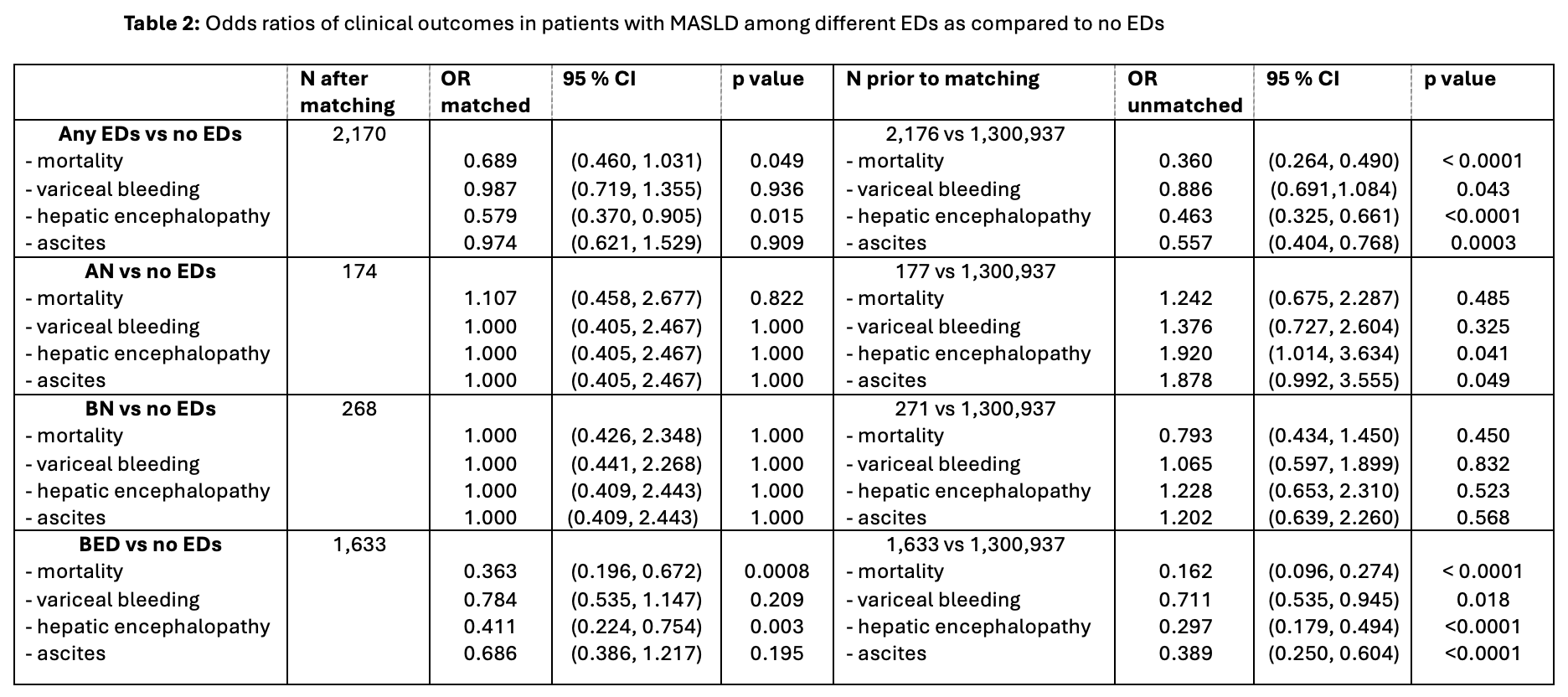
Figure: Table 2: Odds ratios of clinical outcomes in patients with MASLD among different EDs as compared to no EDs
Disclosures:
Alexander Malik indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Morgan Starkey indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Alexander Malik, MD1, Thai Hau Koo, MD2, Morgan R. Starkey, MD3, Adrian S. Lindsey, MD1. P3727 - Prevalence and Outcomes of Eating Disorders in Patients With Metabolic-Associated Steatotic Liver Disease Following Introduction of DSM V, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3MetroHealth Medical Center, Cleveland, OH
Introduction: Previous studies have shown a potential link between MASLD and eating disorders (EDs), which include binge eating disorder (BED), anorexia nervosa (AN), and bulimia nervosa (BN). We aimed to assess the prevalence and outcomes associated with EDs in patients with MASLD.
Methods: We conducted a retrospective cohort study using de-identified patient data from the global TriNetX database (2013–2025; since DSM-5 was introduced in May 2013), including all adults (≥18 years) with MASLD. Data were collected from 134 healthcare organizations in 14 different countries. Cohorts with MASLD with/without any ED (AN, BN, BED) and a control cohort (without MASLD) were created. Propensity score matching (1:1) was used to adjust for demographic and confounding variables. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of mortality and hepatic decompensation (ascites, hepatic encephalopathy [HE], and variceal hemorrhage (VH)) within 3, 6, and 12 months. Subgroup analyses were assessed by ED subtypes.
Results: Among the 1,303,113 adults with MASLD, 2,176 (0.17%) had a coexisting diagnosis of ED. BED was the most common (75%), followed by BN (12%) and AN (8%). Compared to those without EDs, MASLD patients with EDs were younger (46 vs. 58 years, p< 0.0001), more likely to be female (75% vs. 53%, p< 0.0001), and had higher mean BMIs (39 vs. 32.9, p< 0.0001). Patients with ED also had higher rates of mood and anxiety disorders (p< 0.0001). Following PSM, patients with MASLD and any ED had significantly lower odds of HE (OR 0.579, 95% CI, 0.370–0.905; p=0.015) and mortality (OR 0.689, 95% CI, 0.460–1.031; p=0.049). BED use was independently associated with lower mortality (OR 0.363, p=0.0008) and HE (OR 0.411, p=0.003). There were no statistically significant differences in ascites or VH between matched cohorts. Notably, the incidence of BED in patients with MASLD more than doubled following the COVID-19 pandemic (0.06% to 0.13%), with the largest increase among younger adults and females.
Discussion: Contrary to our initial hypothesis, patients with MASLD and comorbid EDs did not experience higher rates of adverse hepatic outcomes. Instead, several ED subgroups had significantly lower rates of HE and mortality than those without EDs. These findings may reflect earlier diagnosis, more frequent healthcare engagement, or differential treatment access among patients with EDs, especially those already receiving psychiatric or weight management care.
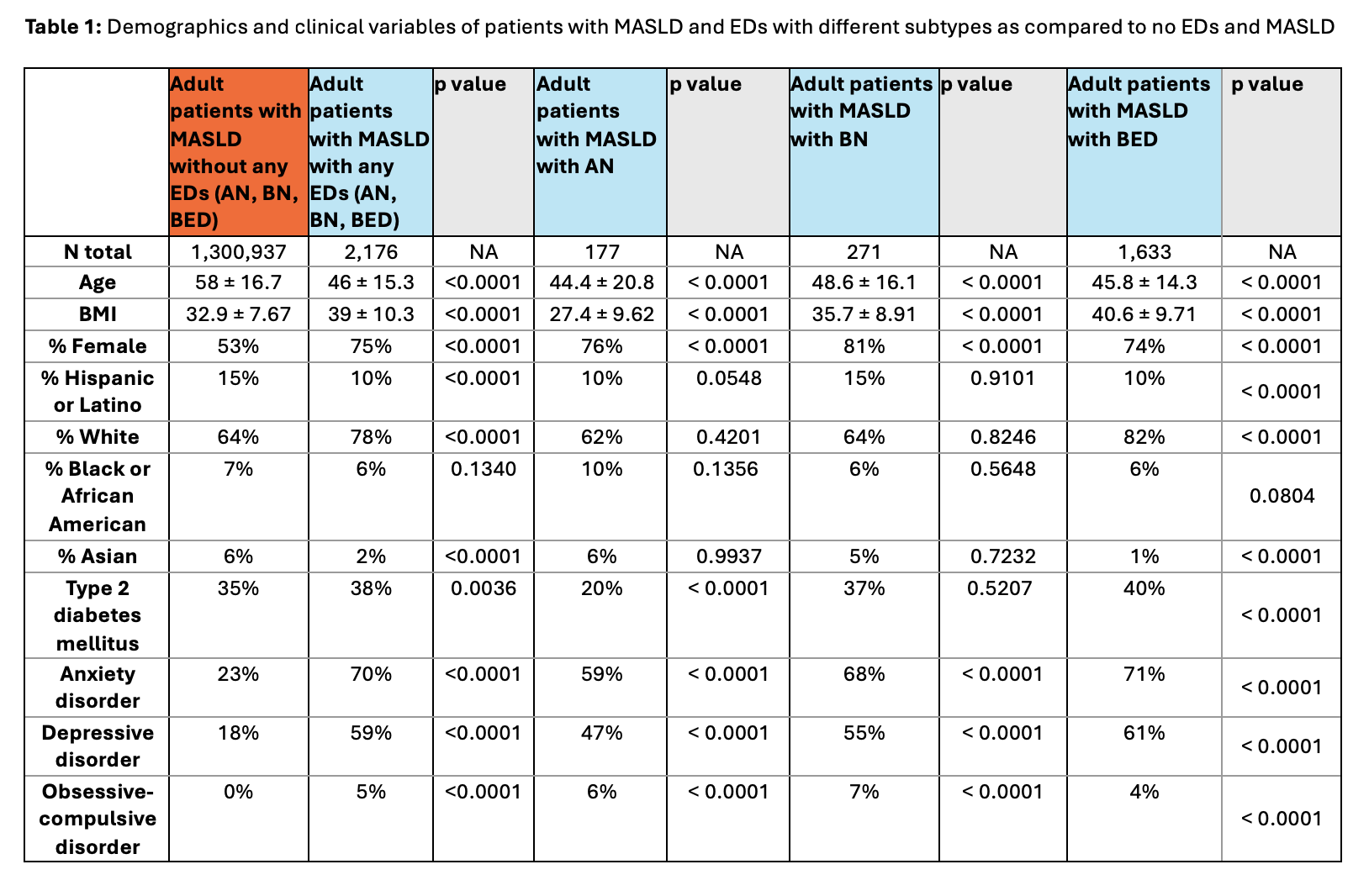
Figure: Table 1: Demographics and clinical variables of patients with MASLD and EDs with different subtypes as compared to no EDs and MASLD
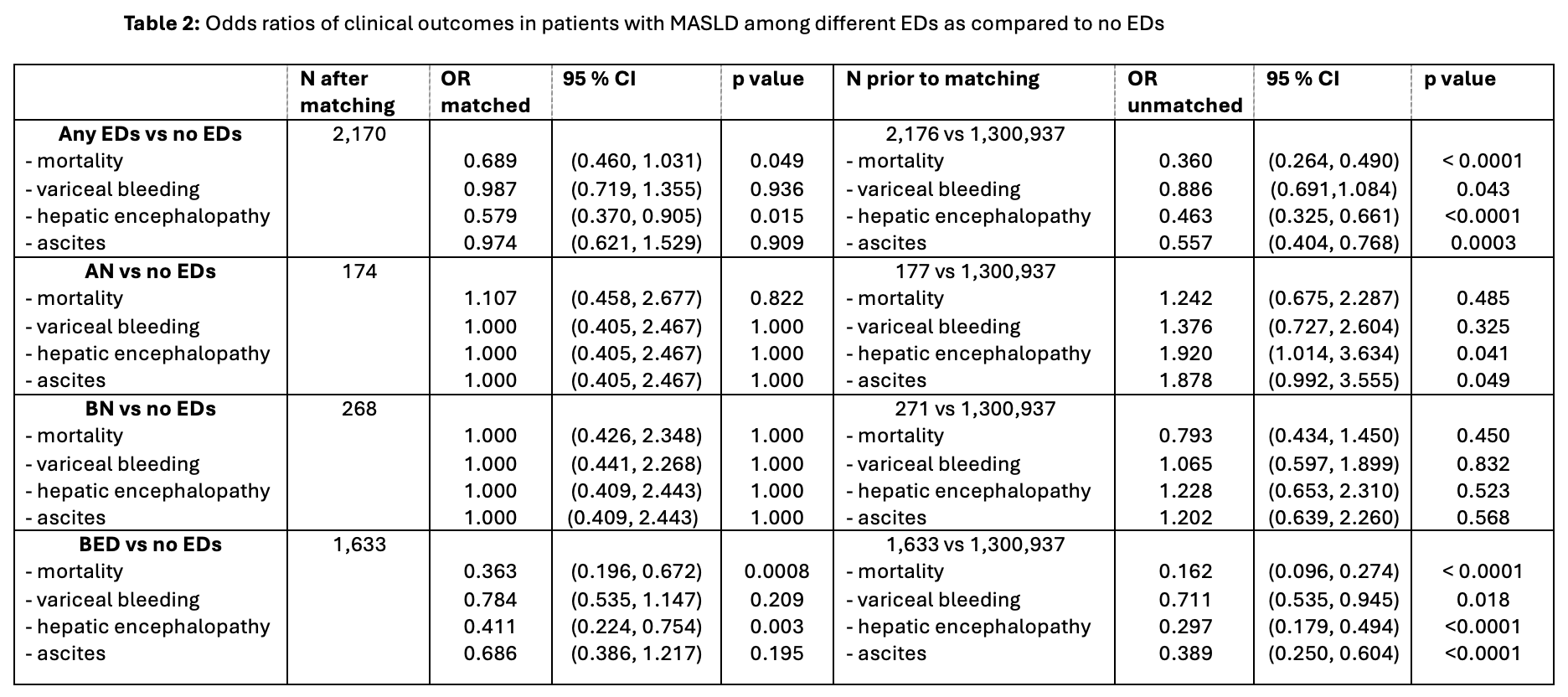
Figure: Table 2: Odds ratios of clinical outcomes in patients with MASLD among different EDs as compared to no EDs
Disclosures:
Alexander Malik indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Morgan Starkey indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Alexander Malik, MD1, Thai Hau Koo, MD2, Morgan R. Starkey, MD3, Adrian S. Lindsey, MD1. P3727 - Prevalence and Outcomes of Eating Disorders in Patients With Metabolic-Associated Steatotic Liver Disease Following Introduction of DSM V, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
