Monday Poster Session
Category: Liver
P3726 - Unveiling Pseudocirrhosis: A Review of Clinical and Diagnostic Characteristics
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tessa Doolittle, MD (she/her/hers)
SUNY Upstate Medical University Hospital
Syracuse, NY
Presenting Author(s)
Tessa Doolittle, MD1, Amanda Eisinger, DO2, Mark M. Aloysius, PhD, ABOM, NBPNS3, Bishnu Sapkota, MD, FACG3, Ayorinde Soipe, MD, MSc4, Savio John, MD, FACG3, Ganesh Aswath, MD1, Amy Slutzky, PhD, MSLIS3
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Cooper Health Gastroenterology, Philadelphia, PA; 3SUNY Upstate Medical University, Syracuse, NY; 4Peachtree Nephrology, Buford, GA
Introduction: Pseudocirrhosis (PC) is a morphological liver finding described in the setting of metastatic cancer that lacks diagnostic criteria. In this review, we aim to identify characteristics of patients with PC (table 1), criteria used to diagnose PC (table 3) and features of those who developed evidence of portal hypertension (table 4).
Methods: We queried 3 databases, PubMed, CINAHL and Embase for relevant articles using the phrases “pseudocirrhosis” OR “pseudo-cirrhosis”. We included abstracts written in English that identified cases of malignancy-associated PC. Demographics, malignancy, therapeutic agents used, liver imaging findings and defining criteria for PC were extracted. Descriptive statistics for categorical variables were reported as counts and proportions. Median and interquartile range [IQR] were calculated for continuous variables that were not normally distributed.
Results: 34 case reports and 7 case series met inclusion criteria which totaled 57 cases with a median age of 52.5 years [IQR 45-64]. Females comprise 80.7% of cases. 12 primary malignancies were identified with breast cancer as the most common (n=41, 71.8%). 87.8% of cases had evidence of portal hypertension. 49 unique therapeutic agents were reported across 252 agent exposures. Radiographic and histologic evidence of PC were reported in 92.7% and 56.1% of cases respectively.
Discussion: PC is described in metastatic cancer as the radiologic appearance of cirrhosis without associated histopathologic findings. Consistent with some patterns in existing literature, we found most patients with PC had a primary breast cancer (table 1) and were treated with multiple lines of chemotherapeutic agents. Notably, 87.8% of total cases showed evidence of portal hypertension or its sequelae (table 4). Of those cases of patients with PC with no evidence of portal hypertension, 42.9% of patients had a primary breast cancer and received an average of 3.28 therapeutic agents (compared to 71.8% and 4.4 agents respectively in patients who did have evidence of portal hypertension). No patients had a history of alcohol use or viral hepatitis, risk factors for cirrhosis (table 2). PC was described radiologically in 92.7% of total cases and histologically in 56.1% of total cases (table 3). Establishing diagnostic criteria and risk factors for PC and portal hypertension could lead to early diagnosis of PC, allowing for interventions to prevent or slow progression of the liver disease and improve QoL for those with a life-limiting cancer.
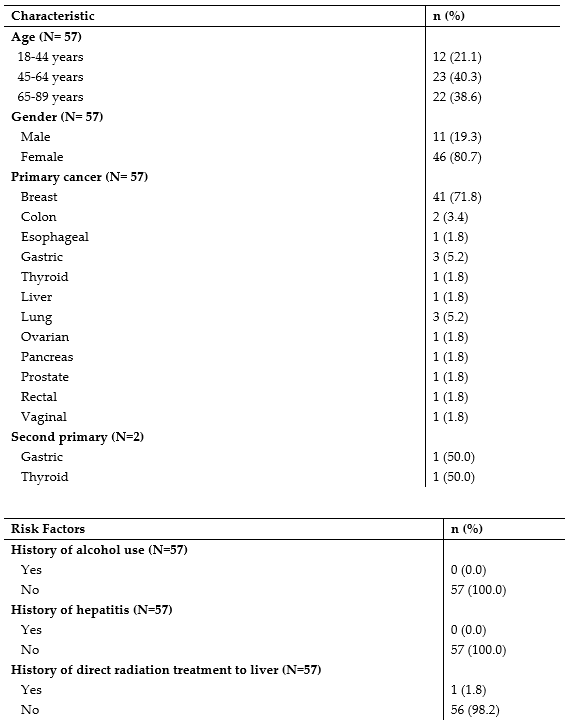
Figure: Table 1. Patient Characteristics
Table 2. Risk Factors for Liver Disease
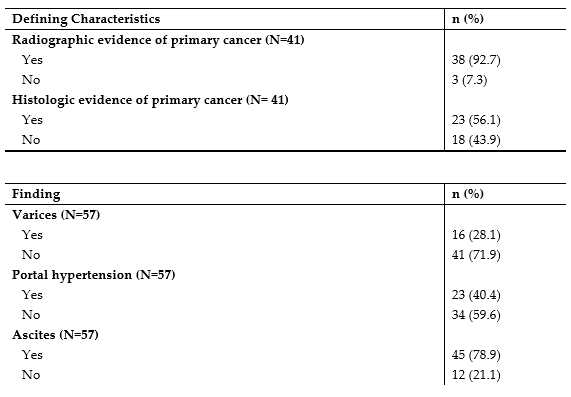
Figure: Table 3. Characteristics Utilized in Defining Pseudocirrhosis
Table 4. Evidence of Portal Hypertension
Disclosures:
Tessa Doolittle indicated no relevant financial relationships.
Amanda Eisinger indicated no relevant financial relationships.
Mark Aloysius indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Ayorinde Soipe indicated no relevant financial relationships.
Savio John indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Amy Slutzky indicated no relevant financial relationships.
Tessa Doolittle, MD1, Amanda Eisinger, DO2, Mark M. Aloysius, PhD, ABOM, NBPNS3, Bishnu Sapkota, MD, FACG3, Ayorinde Soipe, MD, MSc4, Savio John, MD, FACG3, Ganesh Aswath, MD1, Amy Slutzky, PhD, MSLIS3. P3726 - Unveiling Pseudocirrhosis: A Review of Clinical and Diagnostic Characteristics, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Cooper Health Gastroenterology, Philadelphia, PA; 3SUNY Upstate Medical University, Syracuse, NY; 4Peachtree Nephrology, Buford, GA
Introduction: Pseudocirrhosis (PC) is a morphological liver finding described in the setting of metastatic cancer that lacks diagnostic criteria. In this review, we aim to identify characteristics of patients with PC (table 1), criteria used to diagnose PC (table 3) and features of those who developed evidence of portal hypertension (table 4).
Methods: We queried 3 databases, PubMed, CINAHL and Embase for relevant articles using the phrases “pseudocirrhosis” OR “pseudo-cirrhosis”. We included abstracts written in English that identified cases of malignancy-associated PC. Demographics, malignancy, therapeutic agents used, liver imaging findings and defining criteria for PC were extracted. Descriptive statistics for categorical variables were reported as counts and proportions. Median and interquartile range [IQR] were calculated for continuous variables that were not normally distributed.
Results: 34 case reports and 7 case series met inclusion criteria which totaled 57 cases with a median age of 52.5 years [IQR 45-64]. Females comprise 80.7% of cases. 12 primary malignancies were identified with breast cancer as the most common (n=41, 71.8%). 87.8% of cases had evidence of portal hypertension. 49 unique therapeutic agents were reported across 252 agent exposures. Radiographic and histologic evidence of PC were reported in 92.7% and 56.1% of cases respectively.
Discussion: PC is described in metastatic cancer as the radiologic appearance of cirrhosis without associated histopathologic findings. Consistent with some patterns in existing literature, we found most patients with PC had a primary breast cancer (table 1) and were treated with multiple lines of chemotherapeutic agents. Notably, 87.8% of total cases showed evidence of portal hypertension or its sequelae (table 4). Of those cases of patients with PC with no evidence of portal hypertension, 42.9% of patients had a primary breast cancer and received an average of 3.28 therapeutic agents (compared to 71.8% and 4.4 agents respectively in patients who did have evidence of portal hypertension). No patients had a history of alcohol use or viral hepatitis, risk factors for cirrhosis (table 2). PC was described radiologically in 92.7% of total cases and histologically in 56.1% of total cases (table 3). Establishing diagnostic criteria and risk factors for PC and portal hypertension could lead to early diagnosis of PC, allowing for interventions to prevent or slow progression of the liver disease and improve QoL for those with a life-limiting cancer.
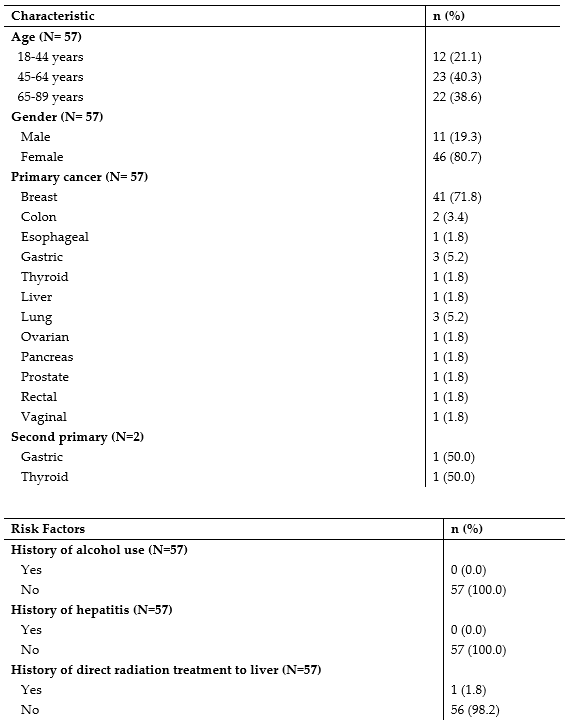
Figure: Table 1. Patient Characteristics
Table 2. Risk Factors for Liver Disease
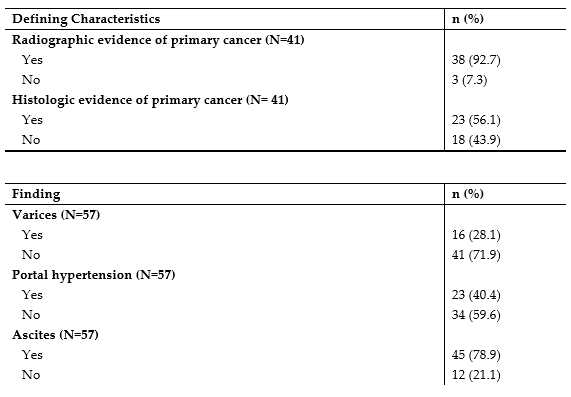
Figure: Table 3. Characteristics Utilized in Defining Pseudocirrhosis
Table 4. Evidence of Portal Hypertension
Disclosures:
Tessa Doolittle indicated no relevant financial relationships.
Amanda Eisinger indicated no relevant financial relationships.
Mark Aloysius indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Ayorinde Soipe indicated no relevant financial relationships.
Savio John indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Amy Slutzky indicated no relevant financial relationships.
Tessa Doolittle, MD1, Amanda Eisinger, DO2, Mark M. Aloysius, PhD, ABOM, NBPNS3, Bishnu Sapkota, MD, FACG3, Ayorinde Soipe, MD, MSc4, Savio John, MD, FACG3, Ganesh Aswath, MD1, Amy Slutzky, PhD, MSLIS3. P3726 - Unveiling Pseudocirrhosis: A Review of Clinical and Diagnostic Characteristics, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
