Tuesday Poster Session
Category: Biliary/Pancreas
P4294 - Morphine Use and Clinical Outcomes in Acute Pancreatitis: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AI
Abdulrahman Ibn Awadh, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abdulrahman Ibn Awadh, MD1, Renad Alharbi, MD2, Mohannad Abuobaid, 3, Musthafa Peedikayli, MD2
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 3College of Medicine, Almaarefa University, Riyadh, Ar Riyad, Saudi Arabia
Introduction: The safety of morphine in acute pancreatitis (AP) remains debated due to theoretical risks of exacerbating complications. This study evaluated whether early morphine use correlates with clinical deterioration in AP.
Methods: In this retrospective cohort study, 154 patients with AP (diagnosed per Revised Atlanta Criteria) treated at a tertiary center (2012–2024) were stratified by morphine use within 48 hours of admission. Outcomes included clinical deterioration (30-day mortality, mechanical ventilation, vasopressor use, surgery, prolonged hospitalization, CRP doubling, or new organ failure). Logistic regression models were adjusted for age, sex, disease severity, ICU admission, and inflammatory markers.
Results: Of 154 patients, 53 received early morphine. Baseline characteristics showed no age/sex differences, but morphine recipients had lower mechanical ventilation rates (17.0% vs. 35.6%, p=0.02) and higher hemoglobin (131.0 vs. 122.0 g/L, p=0.01). Clinical deterioration occurred in 49.1% (morphine) vs. 62.4% (non-morphine), with no significant difference (adjusted OR=0.61, 95% CI: 0.29–1.28, p=0.19). High-dose opioids (MME ≥100, n=24) showed no association with deterioration (p >0.05). Severity-adjusted analyses confirmed these findings.
Discussion: Early morphine/Opioids use in AP was not associated with increased risk of clinical deterioration, even at higher doses. These findings challenge historical concerns and support cautious opioid analgesia in AP, though prospective trials are needed to confirm safety.
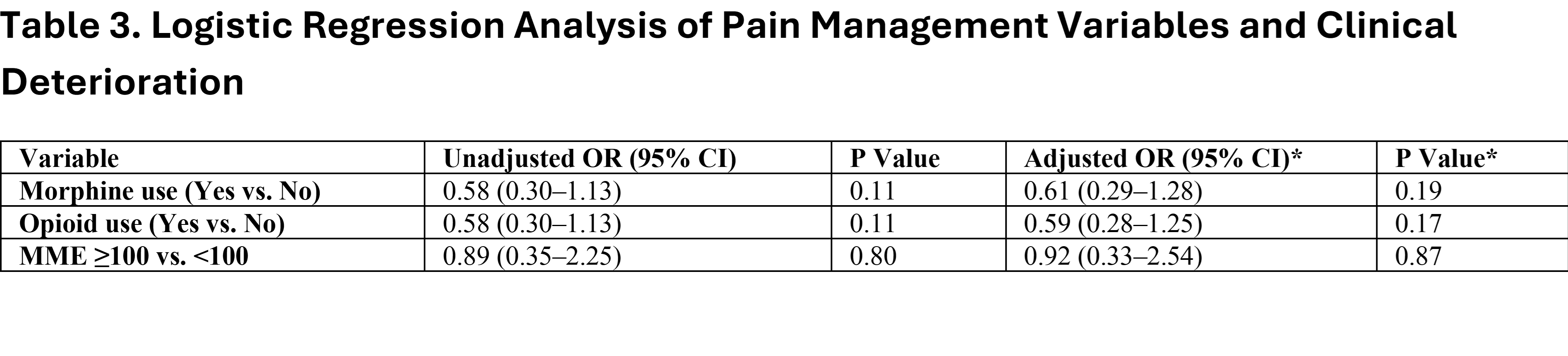
Figure: *Data are median (IQR) or No. (%). CRP = C-reactive protein; ICU = intensive care unit; WBC = white blood cell count.
**P values for continuous variables (Wilcoxon rank-sum test) and categorical variables (chi-square test).
‡"Other" includes etiologies with <5% prevalence (e.g., hypertriglyceridemia, ERCP, genetic). Nationality (100% Saudi) omitted due to lack of variation.*
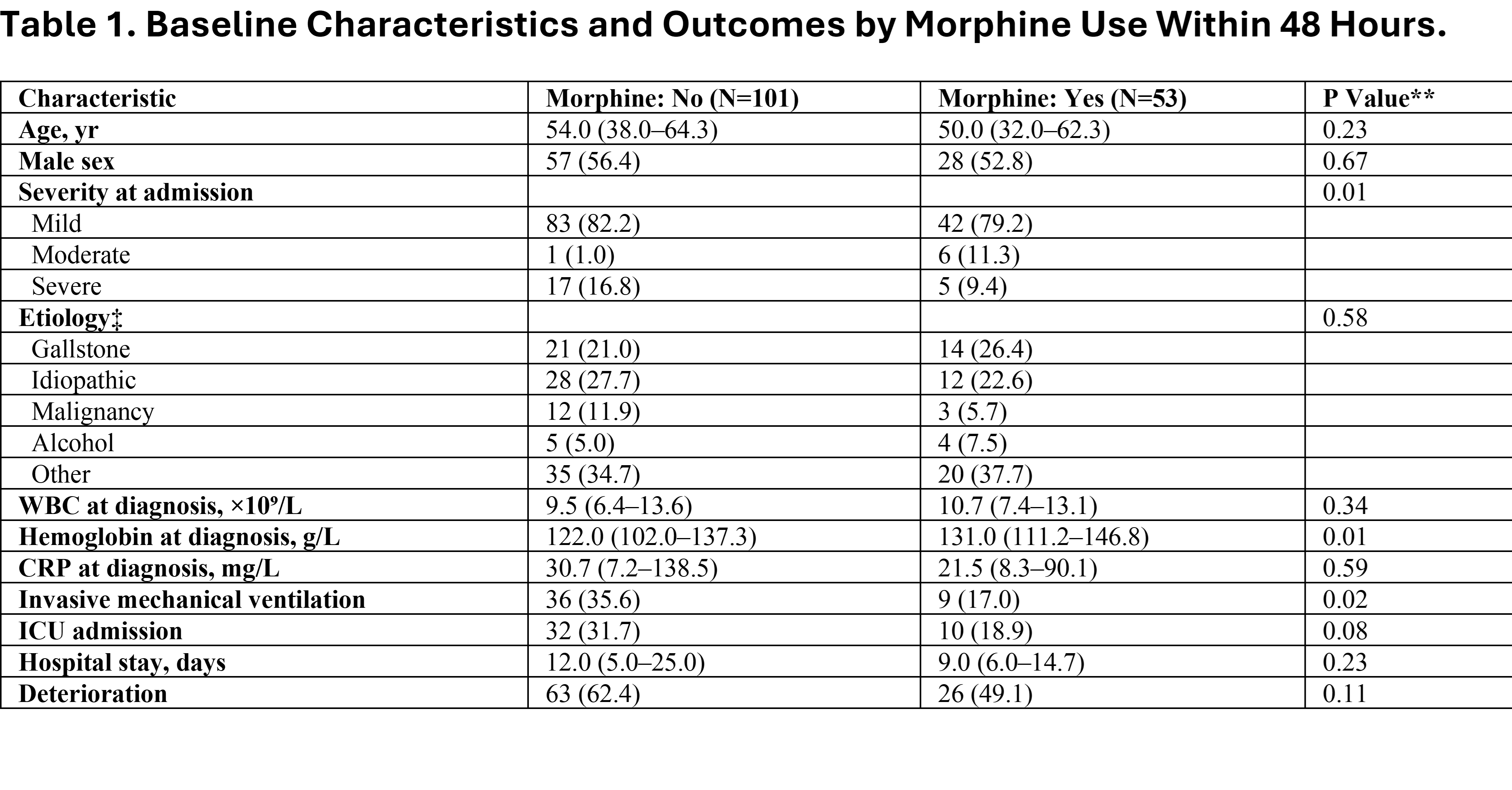
Figure: OR: Odds Ratio; CI: Confidence Interval; WBC: White Blood Cell Count; CRP: C-Reactive Protein; ICU: Intensive Care Unit.*Adjusted for age, sex, severity at admission, ICU admission, invasive mechanical ventilation, and CRP.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Renad Alharbi indicated no relevant financial relationships.
Mohannad Abuobaid indicated no relevant financial relationships.
Musthafa Peedikayli indicated no relevant financial relationships.
Abdulrahman Ibn Awadh, MD1, Renad Alharbi, MD2, Mohannad Abuobaid, 3, Musthafa Peedikayli, MD2. P4294 - Morphine Use and Clinical Outcomes in Acute Pancreatitis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia; 3College of Medicine, Almaarefa University, Riyadh, Ar Riyad, Saudi Arabia
Introduction: The safety of morphine in acute pancreatitis (AP) remains debated due to theoretical risks of exacerbating complications. This study evaluated whether early morphine use correlates with clinical deterioration in AP.
Methods: In this retrospective cohort study, 154 patients with AP (diagnosed per Revised Atlanta Criteria) treated at a tertiary center (2012–2024) were stratified by morphine use within 48 hours of admission. Outcomes included clinical deterioration (30-day mortality, mechanical ventilation, vasopressor use, surgery, prolonged hospitalization, CRP doubling, or new organ failure). Logistic regression models were adjusted for age, sex, disease severity, ICU admission, and inflammatory markers.
Results: Of 154 patients, 53 received early morphine. Baseline characteristics showed no age/sex differences, but morphine recipients had lower mechanical ventilation rates (17.0% vs. 35.6%, p=0.02) and higher hemoglobin (131.0 vs. 122.0 g/L, p=0.01). Clinical deterioration occurred in 49.1% (morphine) vs. 62.4% (non-morphine), with no significant difference (adjusted OR=0.61, 95% CI: 0.29–1.28, p=0.19). High-dose opioids (MME ≥100, n=24) showed no association with deterioration (p >0.05). Severity-adjusted analyses confirmed these findings.
Discussion: Early morphine/Opioids use in AP was not associated with increased risk of clinical deterioration, even at higher doses. These findings challenge historical concerns and support cautious opioid analgesia in AP, though prospective trials are needed to confirm safety.
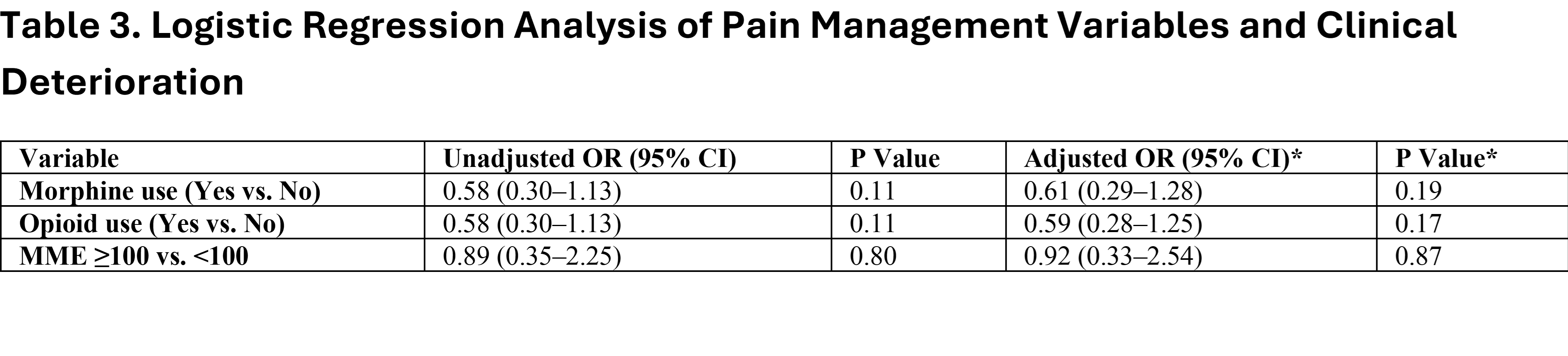
Figure: *Data are median (IQR) or No. (%). CRP = C-reactive protein; ICU = intensive care unit; WBC = white blood cell count.
**P values for continuous variables (Wilcoxon rank-sum test) and categorical variables (chi-square test).
‡"Other" includes etiologies with <5% prevalence (e.g., hypertriglyceridemia, ERCP, genetic). Nationality (100% Saudi) omitted due to lack of variation.*
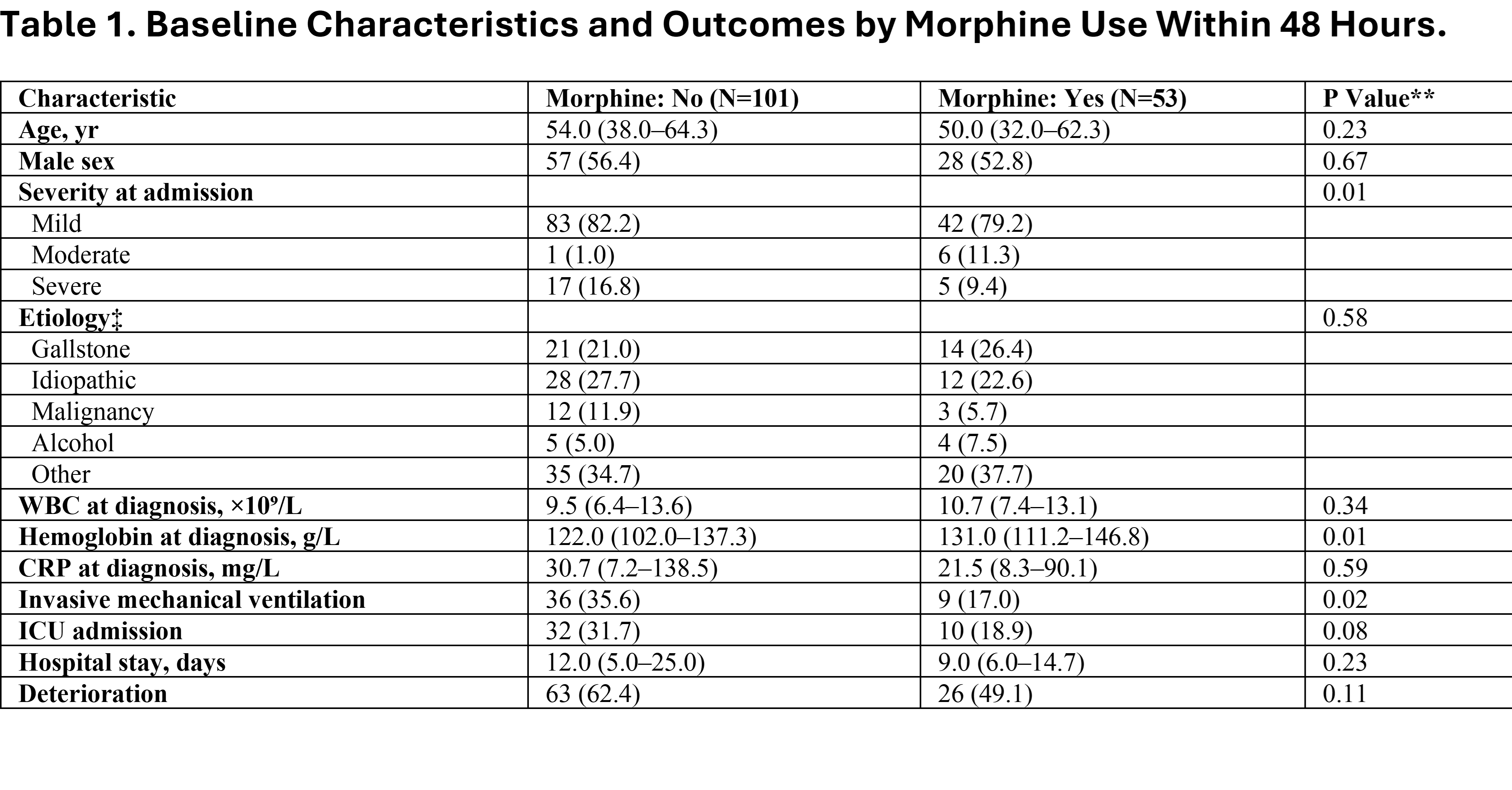
Figure: OR: Odds Ratio; CI: Confidence Interval; WBC: White Blood Cell Count; CRP: C-Reactive Protein; ICU: Intensive Care Unit.*Adjusted for age, sex, severity at admission, ICU admission, invasive mechanical ventilation, and CRP.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Renad Alharbi indicated no relevant financial relationships.
Mohannad Abuobaid indicated no relevant financial relationships.
Musthafa Peedikayli indicated no relevant financial relationships.
Abdulrahman Ibn Awadh, MD1, Renad Alharbi, MD2, Mohannad Abuobaid, 3, Musthafa Peedikayli, MD2. P4294 - Morphine Use and Clinical Outcomes in Acute Pancreatitis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
