Tuesday Poster Session
Category: Biliary/Pancreas
P4293 - Diabetes- and Pancreatitis-Related Mortality in the US Population Aged ≥45 Years (2010-2020): Temporal Trends, Demographic Disparities, and Subtype-Specific Mortality Drivers
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AK
Anum Khakwani, MD (she/her/hers)
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Moiz Ul Haq Hashmi, MBBS1, Ayesha Khan, MBBS1, Azka Aisha, MBBS1, Aqsa Komel, MBBS1, Anum Khakwani, MD2, Muhammad Hassan, MBBS1, Laiba Yumn, MBBS1, Kinza Asghar, MBBS1, Muneeb Khawar, MBBS3
1Nishtar Medical University, Multan, Punjab, Pakistan; 2Charleston Area Medical Center, Charleston, WV; 3King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Emerging data underscores the association of diabetes mellitus (DM) with pancreatitis. Our study identifies trends and disparities in DM with pancreatitis-related mortalities across the U.S. adult population with focus on the differences of acute and chronic pancreatitis (AP and CP)subtypes.
Methods: We obtained data for adults aged ≥45 from the multiple causes of death files using CDC WONDER spanning 2010 to 2020. ICD-10 codes were used to identify mortality cases. Age-adjusted mortality rates (AAMRs) per 100,000 individuals were categorized as per demographic and regional distribution, and Joinpoint regression analysis was performed to calculate annual percent changes (APCs) with 95% confidence intervals (CIs).
Results: From 2010 to 2020, pancreatitis and DM caused 9,857 deaths in U.S. adults aged ≥45. Age-adjusted mortality rates (AAMRs) for AP-DM and CP-DM increased, peaking in 2020 (AP-DM: 0.5771; CP-DM: 0.2702). CP-DM AAMRs rose significantly from 0.205 in 2015 to 0.270 in 2020 (APC: 6.25), while AP-DM surged from 0.422 in 2019 to 0.577 in 2020 (APC: 42.51). Overall, males had higher AAMRs than females; CP-DM- related AAMRs in males ≥65 increased from 0.3 (2017) to 0.519 (2020; APC: 17.33). Rural areas had higher AAMRs than urban areas. States with the highest AAMRs were Oklahoma (AP-DM: 1.072), West Virginia (AP-DM: 0.905; CP-DM: 0.383), and the District of Columbia (CP-DM: 0.502). Black and White populations had higher AAMRs, with sharp increases from 2019 to 2020 (Black APC: 47; White APC: 45.14).
Discussion: AP-DM contributed to more deaths than CP-DM across the decade. The highest AAMRs were observed in older males, urban populations, and African Americans/Blacks and Whites. The results suggest an increasing trend in mortality due to DM and pancreatitis, especially at the end of the decade. These findings emphasize the need for targeted interventions aimed at reducing mortality due to pancreatitis and DM, particularly among the susceptible populations.
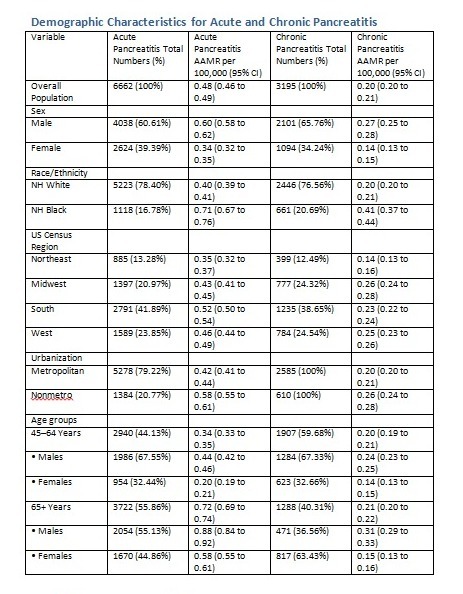
Figure: Demographic Characteristics for Acute and Chronic Pancreatitis
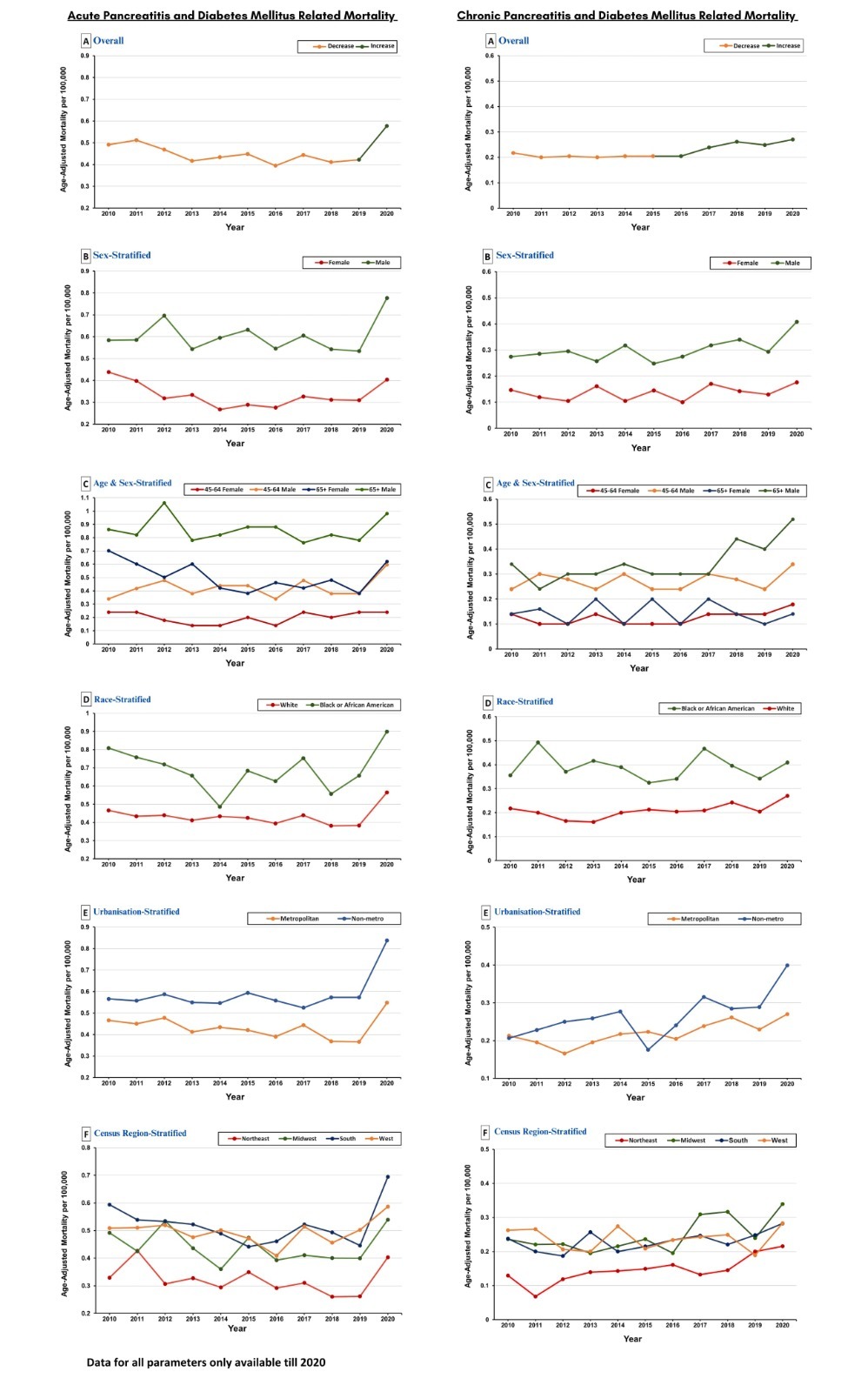
Figure: Pancreatitis and Diabetes related Mortality
Disclosures:
Moiz Ul Haq Hashmi indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Azka Aisha indicated no relevant financial relationships.
Aqsa Komel indicated no relevant financial relationships.
Anum Khakwani indicated no relevant financial relationships.
Muhammad Hassan indicated no relevant financial relationships.
Laiba Yumn indicated no relevant financial relationships.
Kinza Asghar indicated no relevant financial relationships.
Muneeb Khawar indicated no relevant financial relationships.
Moiz Ul Haq Hashmi, MBBS1, Ayesha Khan, MBBS1, Azka Aisha, MBBS1, Aqsa Komel, MBBS1, Anum Khakwani, MD2, Muhammad Hassan, MBBS1, Laiba Yumn, MBBS1, Kinza Asghar, MBBS1, Muneeb Khawar, MBBS3. P4293 - Diabetes- and Pancreatitis-Related Mortality in the US Population Aged ≥45 Years (2010-2020): Temporal Trends, Demographic Disparities, and Subtype-Specific Mortality Drivers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nishtar Medical University, Multan, Punjab, Pakistan; 2Charleston Area Medical Center, Charleston, WV; 3King Edward Medical University, Lahore, Punjab, Pakistan
Introduction: Emerging data underscores the association of diabetes mellitus (DM) with pancreatitis. Our study identifies trends and disparities in DM with pancreatitis-related mortalities across the U.S. adult population with focus on the differences of acute and chronic pancreatitis (AP and CP)subtypes.
Methods: We obtained data for adults aged ≥45 from the multiple causes of death files using CDC WONDER spanning 2010 to 2020. ICD-10 codes were used to identify mortality cases. Age-adjusted mortality rates (AAMRs) per 100,000 individuals were categorized as per demographic and regional distribution, and Joinpoint regression analysis was performed to calculate annual percent changes (APCs) with 95% confidence intervals (CIs).
Results: From 2010 to 2020, pancreatitis and DM caused 9,857 deaths in U.S. adults aged ≥45. Age-adjusted mortality rates (AAMRs) for AP-DM and CP-DM increased, peaking in 2020 (AP-DM: 0.5771; CP-DM: 0.2702). CP-DM AAMRs rose significantly from 0.205 in 2015 to 0.270 in 2020 (APC: 6.25), while AP-DM surged from 0.422 in 2019 to 0.577 in 2020 (APC: 42.51). Overall, males had higher AAMRs than females; CP-DM- related AAMRs in males ≥65 increased from 0.3 (2017) to 0.519 (2020; APC: 17.33). Rural areas had higher AAMRs than urban areas. States with the highest AAMRs were Oklahoma (AP-DM: 1.072), West Virginia (AP-DM: 0.905; CP-DM: 0.383), and the District of Columbia (CP-DM: 0.502). Black and White populations had higher AAMRs, with sharp increases from 2019 to 2020 (Black APC: 47; White APC: 45.14).
Discussion: AP-DM contributed to more deaths than CP-DM across the decade. The highest AAMRs were observed in older males, urban populations, and African Americans/Blacks and Whites. The results suggest an increasing trend in mortality due to DM and pancreatitis, especially at the end of the decade. These findings emphasize the need for targeted interventions aimed at reducing mortality due to pancreatitis and DM, particularly among the susceptible populations.
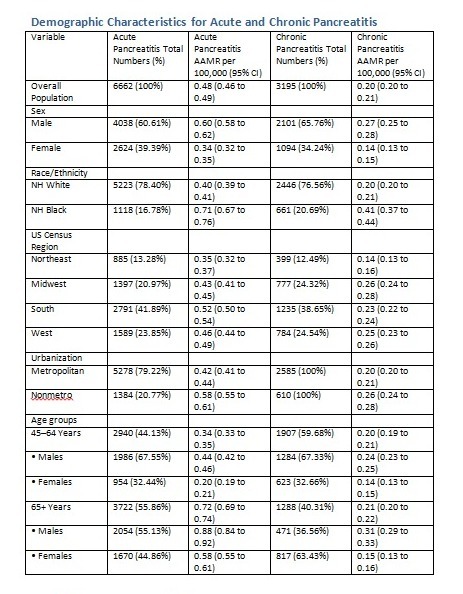
Figure: Demographic Characteristics for Acute and Chronic Pancreatitis
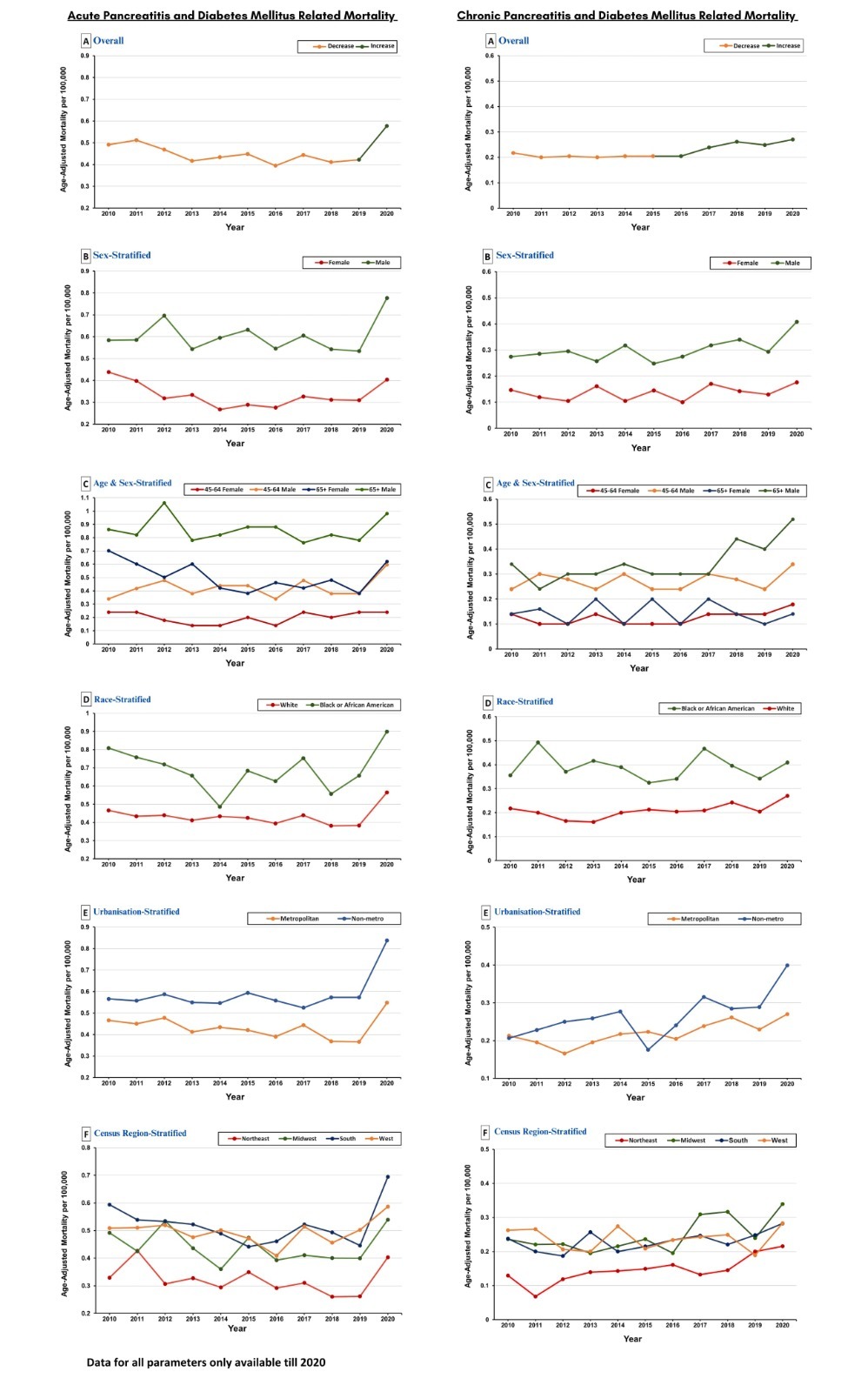
Figure: Pancreatitis and Diabetes related Mortality
Disclosures:
Moiz Ul Haq Hashmi indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Azka Aisha indicated no relevant financial relationships.
Aqsa Komel indicated no relevant financial relationships.
Anum Khakwani indicated no relevant financial relationships.
Muhammad Hassan indicated no relevant financial relationships.
Laiba Yumn indicated no relevant financial relationships.
Kinza Asghar indicated no relevant financial relationships.
Muneeb Khawar indicated no relevant financial relationships.
Moiz Ul Haq Hashmi, MBBS1, Ayesha Khan, MBBS1, Azka Aisha, MBBS1, Aqsa Komel, MBBS1, Anum Khakwani, MD2, Muhammad Hassan, MBBS1, Laiba Yumn, MBBS1, Kinza Asghar, MBBS1, Muneeb Khawar, MBBS3. P4293 - Diabetes- and Pancreatitis-Related Mortality in the US Population Aged ≥45 Years (2010-2020): Temporal Trends, Demographic Disparities, and Subtype-Specific Mortality Drivers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
