Tuesday Poster Session
Category: Biliary/Pancreas
P4292 - Increased Odds of Developing Diabetes Following Sentinel Episode of Acute Pancreatitis in Patients With Obesity: A Propensity-Matched Population Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GH
Gordon Hong, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Gordon Hong, MD1, Abbinaya Elangovan, MD2, Elleson Harper, BS1, Jaime A. Perez, PhD1, Stacey Culp, PhD3, Hamza Shah, DO3, Mitchell L. Ramsey, MD3, Peter Lee, MBBCh3, Somashekar Krishna, MD, MPH3, Kathleen Dungan, MD3, Georgios I. Papachristou, MD, PhD3, Philip A. Hart, MD3, Raj Shah, MD3
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Acute pancreatitis (AP) is among the most common causes of diabetes mellitus (DM) secondary to diseases of the exocrine pancreas. Obesity is a shared risk factor for both AP and DM; however, the longitudinal risk of developing DM after AP in patients with obesity is not well understood. In this study, we assess the risk of developing DM following a sentinel episode of AP in patients with obesity.
Methods: A retrospective cohort study was conducted using TriNetX, a multi-institutional research network. The study population was limited to patients with obesity based on ICD codes or BMI ≥ 30 kg/m2. Cases with AP (based on ICD code K85) and controls without a history of AP were selected. Patients with DM, prediabetes (based on ICD codes or HbA1c ≥5.7%), or use of diabetes medications prior to index AP episode or the diagnosis of obesity for controls were excluded. Patients with glucagon-like peptide-1 (GLP-1) medications, alcohol-related pancreatitis, alcohol-related disorders, pancreatic cancer, pancreatic surgery, and cystic fibrosis were also excluded. Patients were required to have at least one outpatient visit following the index episode of AP (cases) or diagnosis of obesity (controls). Propensity score matching was performed on the basis of age, sex, race, ethnicity, and BMI. New diagnosis of diabetes between groups was compared at multiple timepoints (within 1, 3, 6, 12, 36, and 60 months) following the index event.
Results: A total of 11,466 patients were identified in the AP group and 6,378,842 patients were identified in the control group. Propensity matching was successful with 11,464 cases and 11,464 controls (SMD< 0.1), Baseline characteristics were similar in regard to age, sex, race, ethnicity, BMI (Table 1). Odds ratios (OR) for new diagnosis of DM in the AP group compared to propensity matched controls were 3.13, 2.66, 2.52, 2.12, 1.96, and 1.77 within 1, 3, 6, 12, 36, and 60 months, respectively (Table 2).
Discussion: In this large retrospective cohort study, odds of developing DM in the AP group when compared to a matched control cohort with obesity were highest at timepoints immediately following the index event. Furthermore, odds of developing DM exceeded what was observed in matched controls at each timepoint, suggesting there may be additional mechanisms underlying DM following AP beyond shared risk factors. Further investigations are needed to identify opportunities for risk factor reduction and prevention strategies.
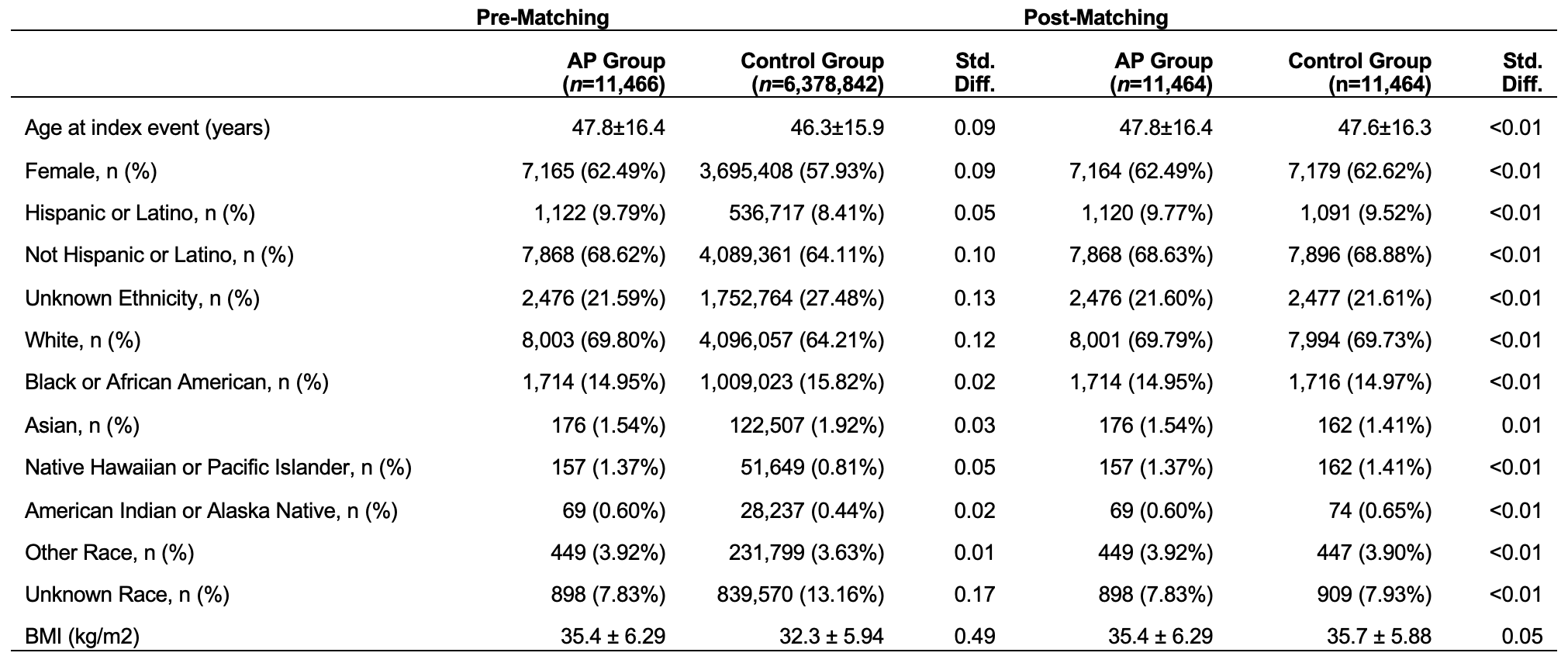
Figure: Table 1:
Patients in the AP group and control group were propensity score matched 1:1 for age at time of index event, gender, ethnicity, race and BMI. Groups were well matched with standard mean difference (std. diff.) less than 0.1.

Figure: Table 2:
Patients in the AP group had significantly higher rate of new diagnosis of DM compared to the control group at each timepoint, with p-values <0.0001. Odds ratios at each time interval also demonstrate higher odds of developing DM in the AP group with greater odds at timepoints closest to the time of index event.
Disclosures:
Gordon Hong indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Stacey Culp indicated no relevant financial relationships.
Hamza Shah indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Peter Lee indicated no relevant financial relationships.
Somashekar Krishna indicated no relevant financial relationships.
Kathleen Dungan: Eli Lilly and Company – Consultant. Insulet – Grant/Research Support. Oppenheimer – Consultant.
Georgios Papachristou: AbbVie – Grant/Research Support.
Philip Hart indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Gordon Hong, MD1, Abbinaya Elangovan, MD2, Elleson Harper, BS1, Jaime A. Perez, PhD1, Stacey Culp, PhD3, Hamza Shah, DO3, Mitchell L. Ramsey, MD3, Peter Lee, MBBCh3, Somashekar Krishna, MD, MPH3, Kathleen Dungan, MD3, Georgios I. Papachristou, MD, PhD3, Philip A. Hart, MD3, Raj Shah, MD3. P4292 - Increased Odds of Developing Diabetes Following Sentinel Episode of Acute Pancreatitis in Patients With Obesity: A Propensity-Matched Population Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Virginia Tech Carilion School of Medicine, Roanoke, VA; 3The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Acute pancreatitis (AP) is among the most common causes of diabetes mellitus (DM) secondary to diseases of the exocrine pancreas. Obesity is a shared risk factor for both AP and DM; however, the longitudinal risk of developing DM after AP in patients with obesity is not well understood. In this study, we assess the risk of developing DM following a sentinel episode of AP in patients with obesity.
Methods: A retrospective cohort study was conducted using TriNetX, a multi-institutional research network. The study population was limited to patients with obesity based on ICD codes or BMI ≥ 30 kg/m2. Cases with AP (based on ICD code K85) and controls without a history of AP were selected. Patients with DM, prediabetes (based on ICD codes or HbA1c ≥5.7%), or use of diabetes medications prior to index AP episode or the diagnosis of obesity for controls were excluded. Patients with glucagon-like peptide-1 (GLP-1) medications, alcohol-related pancreatitis, alcohol-related disorders, pancreatic cancer, pancreatic surgery, and cystic fibrosis were also excluded. Patients were required to have at least one outpatient visit following the index episode of AP (cases) or diagnosis of obesity (controls). Propensity score matching was performed on the basis of age, sex, race, ethnicity, and BMI. New diagnosis of diabetes between groups was compared at multiple timepoints (within 1, 3, 6, 12, 36, and 60 months) following the index event.
Results: A total of 11,466 patients were identified in the AP group and 6,378,842 patients were identified in the control group. Propensity matching was successful with 11,464 cases and 11,464 controls (SMD< 0.1), Baseline characteristics were similar in regard to age, sex, race, ethnicity, BMI (Table 1). Odds ratios (OR) for new diagnosis of DM in the AP group compared to propensity matched controls were 3.13, 2.66, 2.52, 2.12, 1.96, and 1.77 within 1, 3, 6, 12, 36, and 60 months, respectively (Table 2).
Discussion: In this large retrospective cohort study, odds of developing DM in the AP group when compared to a matched control cohort with obesity were highest at timepoints immediately following the index event. Furthermore, odds of developing DM exceeded what was observed in matched controls at each timepoint, suggesting there may be additional mechanisms underlying DM following AP beyond shared risk factors. Further investigations are needed to identify opportunities for risk factor reduction and prevention strategies.
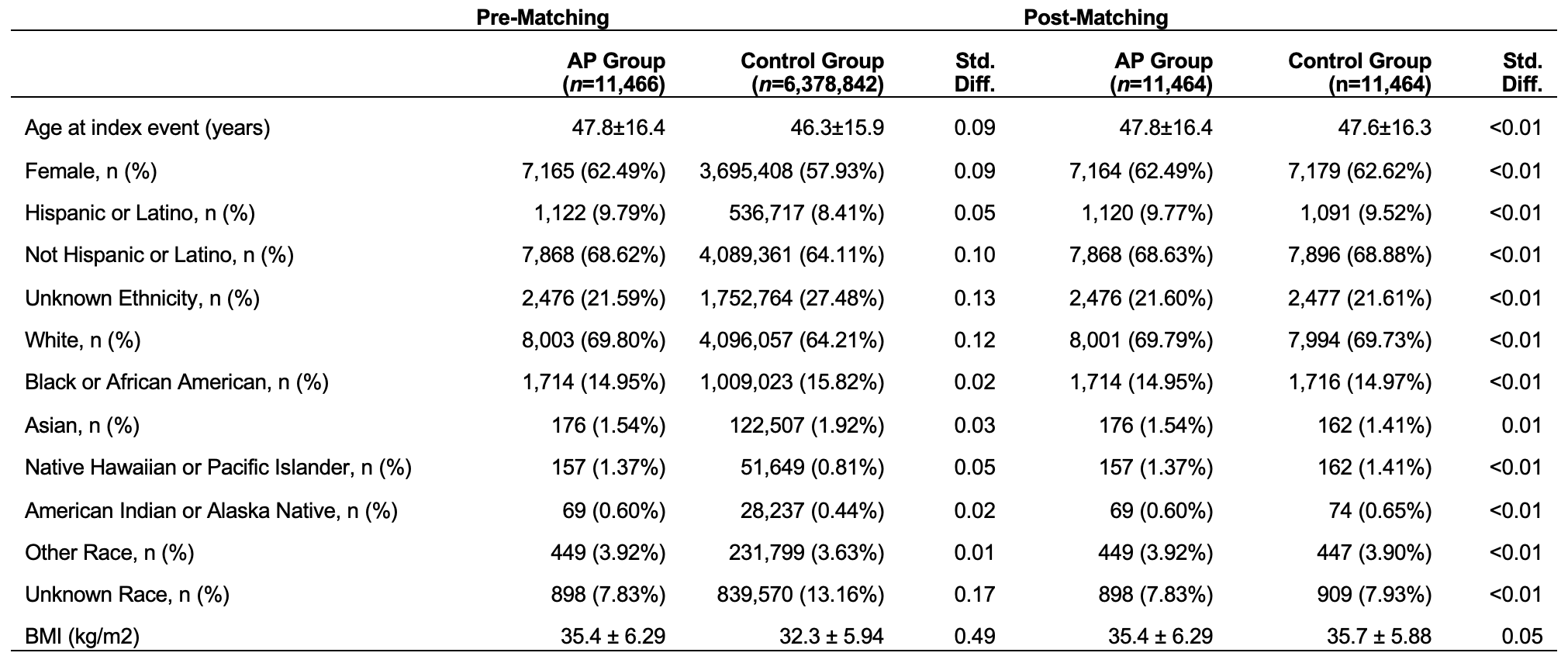
Figure: Table 1:
Patients in the AP group and control group were propensity score matched 1:1 for age at time of index event, gender, ethnicity, race and BMI. Groups were well matched with standard mean difference (std. diff.) less than 0.1.

Figure: Table 2:
Patients in the AP group had significantly higher rate of new diagnosis of DM compared to the control group at each timepoint, with p-values <0.0001. Odds ratios at each time interval also demonstrate higher odds of developing DM in the AP group with greater odds at timepoints closest to the time of index event.
Disclosures:
Gordon Hong indicated no relevant financial relationships.
Abbinaya Elangovan indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Stacey Culp indicated no relevant financial relationships.
Hamza Shah indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Peter Lee indicated no relevant financial relationships.
Somashekar Krishna indicated no relevant financial relationships.
Kathleen Dungan: Eli Lilly and Company – Consultant. Insulet – Grant/Research Support. Oppenheimer – Consultant.
Georgios Papachristou: AbbVie – Grant/Research Support.
Philip Hart indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Gordon Hong, MD1, Abbinaya Elangovan, MD2, Elleson Harper, BS1, Jaime A. Perez, PhD1, Stacey Culp, PhD3, Hamza Shah, DO3, Mitchell L. Ramsey, MD3, Peter Lee, MBBCh3, Somashekar Krishna, MD, MPH3, Kathleen Dungan, MD3, Georgios I. Papachristou, MD, PhD3, Philip A. Hart, MD3, Raj Shah, MD3. P4292 - Increased Odds of Developing Diabetes Following Sentinel Episode of Acute Pancreatitis in Patients With Obesity: A Propensity-Matched Population Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

