Tuesday Poster Session
Category: Biliary/Pancreas
P4283 - General Anesthesia versus Monitored Anesthesia Care During Endoscopic Retrograde Cholangiopancreatography: A Propensity-Matched Analysis of Postprocedural Pancreatitis and Safety Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad AbuAssi, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Mohammad Abuassi, MD1, Saqr Alsakarneh, MD, MS2, Tony Brar, MD3, Yaseen Perbtani, DO1, Mahmoud Y. Madi, MD4, Bashar Qumseya, MD, MPH5
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Kansas City, MO; 3University of Central Florida, Gainesville, FL; 4University of Texas at Austin Dell Medical School, Austin, TX; 5University of Florida College of Medicine, Gainesville, FL
Introduction: Post-ERCP pancreatitis (PEP) is the most frequent and potentially serious complication following endoscopic retrograde cholangiopancreatography (ERCP). Although monitored anesthesia care (MAC) is commonly recommended for sedation, these guidelines are primarily based on expert consensus. This study presents the nationwide analysis comparing general anesthesia (GA) and MAC during ERCP, evaluating both the risk of PEP and overall procedural safety, while adjusting for a broad range of clinical variables, including prophylactic indomethacin use.
Methods: We conducted a retrospective cohort study using the TriNetX Network, a platform that aggregates de-identified electronic health record data from healthcare organizations across the United States. Adults undergoing ERCP between 2005 and 2025 were stratified by anesthesia modality: GA, defined by same-day administration of neuromuscular blocking agents, or MAC. Propensity score matching (1:1) was performed based on demographics and clinical comorbidities. The primary outcome was PEP within 7 days, defined by ICD-10 code K85 or lipase ≥480 U/L. Secondary outcomes included ICU admission, emergency intubation, respiratory failure, and all-cause mortality. Subgroup analyses adjusted for the use of indomethacin. Relative risks (RR), 95% confidence intervals (CI), and number needed to treat (NNT) were calculated.
Results: In total, 187,632 patients (93,816 per group; mean age 66 years, 54% female) were analyzed. GA significantly reduced the incidence of PEP compared to MAC (9.45% vs 11.34%; RR: 0.834, CI: 0.812–0.856; p< 0.001), translating to an NNT of 53. This protective effect persisted among subgroups undergoing sphincterotomy (RR: 0.816, CI: 0.794–0.839) and stenting (RR: 0.849, CI: 0.817–0.882). GA also maintained its protective effect after adjusting for indomethacin use (9.05% vs 10.45%; RR: 0.866, CI: 0.843–0.889; p< 0.001; NNT=59). However, GA was associated with increased ICU admissions (RR: 1.353, CI: 1.280–1.429), emergency intubation (RR: 1.438, CI: 1.217–1.699), and respiratory failure (RR: 1.121, CI: 1.037–1.212). Mortality was comparable (RR 0.93, 95% CI 0.84–1.02).
Discussion: Our study shows that GA significantly reduces PEP independently of indomethacin use, with a clinically relevant NNT of approximately 53. This benefit must be weighed against its higher rates of respiratory complications, especially in high-risk patients. Prospective randomized studies are needed to confirm these findings and guide clinical practice.
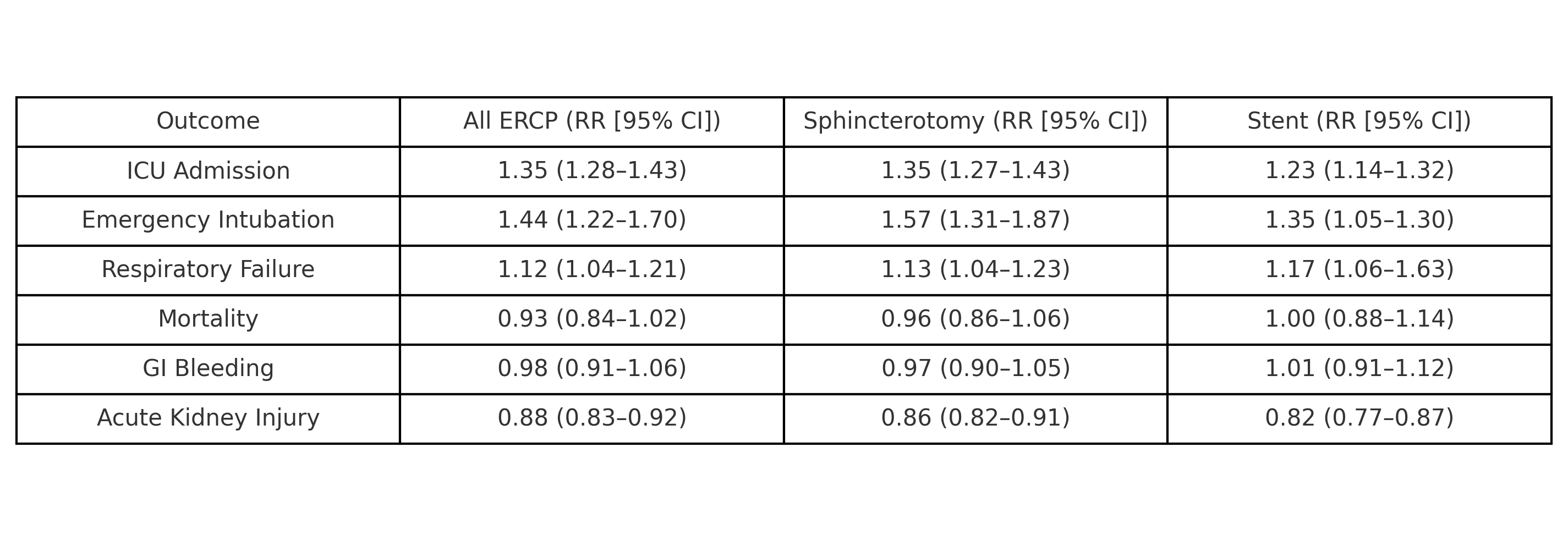
Figure: Relative risk of post-ERCP pancreatitis comparing general anesthesia (GA) to monitored anesthesia care (MAC), overall and in subgroups with and without indomethacin. GA was consistently associated with lower PEP risk across all comparisons.
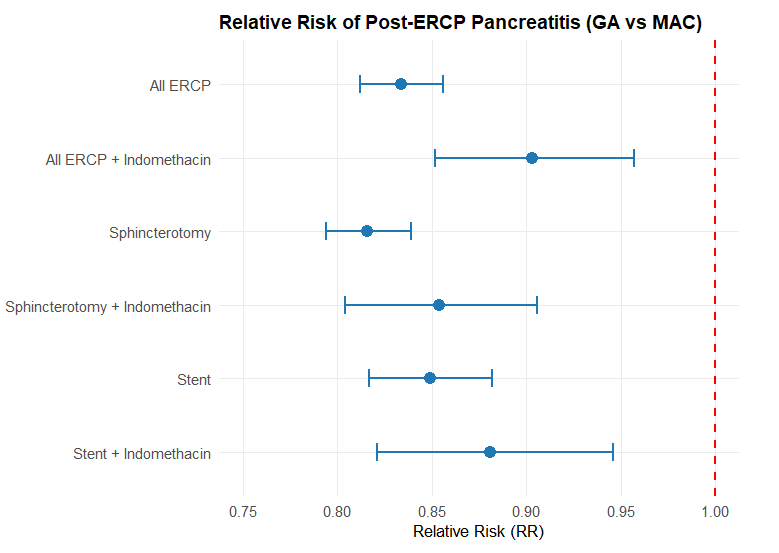
Figure: Relative Risk of Secondary Outcomes Following ERCP Under General Anesthesia (GA) Versus Monitored Anesthesia Care (MAC) Across Three Subgroups: All ERCP, Sphincterotomy, and Stent Placement.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Mohammad Abuassi, MD1, Saqr Alsakarneh, MD, MS2, Tony Brar, MD3, Yaseen Perbtani, DO1, Mahmoud Y. Madi, MD4, Bashar Qumseya, MD, MPH5. P4283 - General Anesthesia versus Monitored Anesthesia Care During Endoscopic Retrograde Cholangiopancreatography: A Propensity-Matched Analysis of Postprocedural Pancreatitis and Safety Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Kansas City, MO; 3University of Central Florida, Gainesville, FL; 4University of Texas at Austin Dell Medical School, Austin, TX; 5University of Florida College of Medicine, Gainesville, FL
Introduction: Post-ERCP pancreatitis (PEP) is the most frequent and potentially serious complication following endoscopic retrograde cholangiopancreatography (ERCP). Although monitored anesthesia care (MAC) is commonly recommended for sedation, these guidelines are primarily based on expert consensus. This study presents the nationwide analysis comparing general anesthesia (GA) and MAC during ERCP, evaluating both the risk of PEP and overall procedural safety, while adjusting for a broad range of clinical variables, including prophylactic indomethacin use.
Methods: We conducted a retrospective cohort study using the TriNetX Network, a platform that aggregates de-identified electronic health record data from healthcare organizations across the United States. Adults undergoing ERCP between 2005 and 2025 were stratified by anesthesia modality: GA, defined by same-day administration of neuromuscular blocking agents, or MAC. Propensity score matching (1:1) was performed based on demographics and clinical comorbidities. The primary outcome was PEP within 7 days, defined by ICD-10 code K85 or lipase ≥480 U/L. Secondary outcomes included ICU admission, emergency intubation, respiratory failure, and all-cause mortality. Subgroup analyses adjusted for the use of indomethacin. Relative risks (RR), 95% confidence intervals (CI), and number needed to treat (NNT) were calculated.
Results: In total, 187,632 patients (93,816 per group; mean age 66 years, 54% female) were analyzed. GA significantly reduced the incidence of PEP compared to MAC (9.45% vs 11.34%; RR: 0.834, CI: 0.812–0.856; p< 0.001), translating to an NNT of 53. This protective effect persisted among subgroups undergoing sphincterotomy (RR: 0.816, CI: 0.794–0.839) and stenting (RR: 0.849, CI: 0.817–0.882). GA also maintained its protective effect after adjusting for indomethacin use (9.05% vs 10.45%; RR: 0.866, CI: 0.843–0.889; p< 0.001; NNT=59). However, GA was associated with increased ICU admissions (RR: 1.353, CI: 1.280–1.429), emergency intubation (RR: 1.438, CI: 1.217–1.699), and respiratory failure (RR: 1.121, CI: 1.037–1.212). Mortality was comparable (RR 0.93, 95% CI 0.84–1.02).
Discussion: Our study shows that GA significantly reduces PEP independently of indomethacin use, with a clinically relevant NNT of approximately 53. This benefit must be weighed against its higher rates of respiratory complications, especially in high-risk patients. Prospective randomized studies are needed to confirm these findings and guide clinical practice.
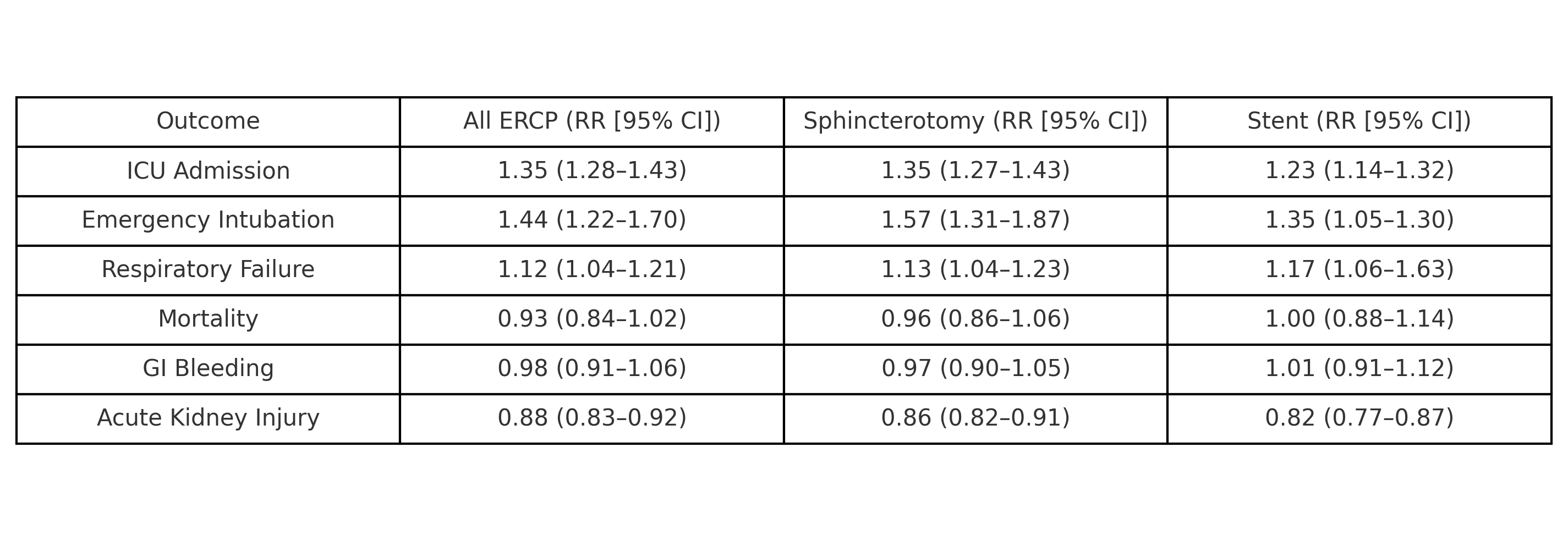
Figure: Relative risk of post-ERCP pancreatitis comparing general anesthesia (GA) to monitored anesthesia care (MAC), overall and in subgroups with and without indomethacin. GA was consistently associated with lower PEP risk across all comparisons.
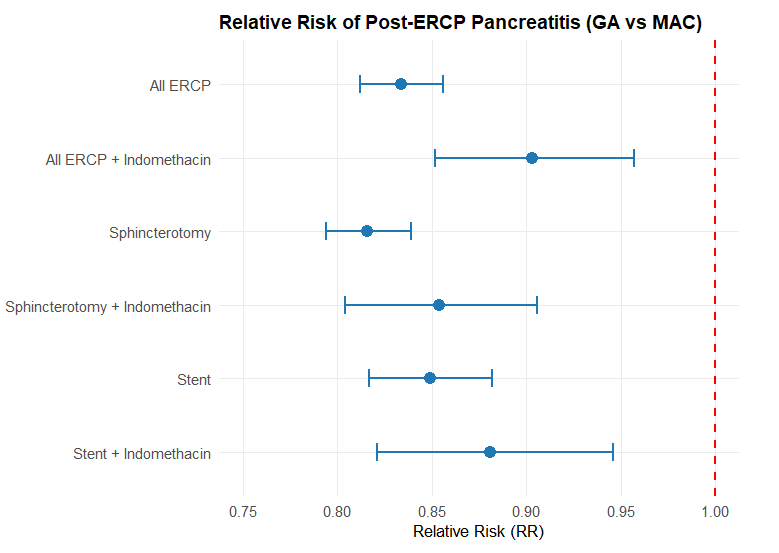
Figure: Relative Risk of Secondary Outcomes Following ERCP Under General Anesthesia (GA) Versus Monitored Anesthesia Care (MAC) Across Three Subgroups: All ERCP, Sphincterotomy, and Stent Placement.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Mohammad Abuassi, MD1, Saqr Alsakarneh, MD, MS2, Tony Brar, MD3, Yaseen Perbtani, DO1, Mahmoud Y. Madi, MD4, Bashar Qumseya, MD, MPH5. P4283 - General Anesthesia versus Monitored Anesthesia Care During Endoscopic Retrograde Cholangiopancreatography: A Propensity-Matched Analysis of Postprocedural Pancreatitis and Safety Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
