Tuesday Poster Session
Category: Biliary/Pancreas
P4346 - Who Really Needs a Drain? Admission Predictors of Successful Conservative Management in Necrotizing Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Petr Vanek, MD, PhD
University of Minnesota, Minneapolis, USA; Palacky University Olomouc, Olomouc, Czech Republic
Minneapolis, MN
Presenting Author(s)
Petr Vanek, MD, PhD1, Gaurav Suryawanshi, MD2, Nauroze Faizi, MD2, Guru Trikudanathan, MD2
1University of Minnesota, Minneapolis, USA; Palacky University Olomouc, Olomouc, Czech Republic, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: Although some patients with necrotizing pancreatitis (NP) are managed with a minimally invasive step-up approach, reliable predictors to identify those who can be managed conservatively remain elusive. We analyzed a prospectively maintained NP database to define baseline predictors of a wholly conservative course.
Methods: Adults admitted with NP between 2009 and 2022 were included. Exclusions were lack of follow-up or death during index admission/within 30 days of discharge. Baseline demographic, clinical, and radiologic variables from contrast-enhanced CT performed ≤ 72 h after admission were evaluated. Conservative management was defined as no percutaneous, endoscopic, or surgical intervention during the entire disease course. Univariable associations were tested with χ² test; multivariable logistic regression was adjusted for demographics, disease severity, and imaging covariates.
Results: Of 512 patients, 155 (30%) completed the entire disease course without intervention and 357 (70%) required drainage at some point. In the multivariable model, sterile necrosis (absence of infection) (adjusted odds ratio [aOR] 8.23, 95% CI 4.37–15.5), collection diameter < 6 cm (aOR 5.67, 95% CI 3.25–9.92), and intact pancreatic duct (absence of disconnection) (aOR 2.51, 95% CI 1.36–4.61) independently predicted success of conservative therapy (all p < 0.005). Among the 357 interventionally managed patients, 273 (77%) underwent a procedure during the index admission; early intervention was again associated with infected necrosis, duct disconnection, and larger collections.
Discussion: Three admission findings—sterile necrosis, smaller collection size (< 6 cm), and an intact pancreatic duct—are independent predictors of successful conservative management in NP. Conversely, the presence of just one adverse feature (infected necrosis, a larger collection, or pancreatic duct disconnection) predicts failure of conservative therapy in the majority of patients; in fact, 8 out of 10 such patients will ultimately require interventional treatment. Incorporating these variables into a clinical decision tool may help defer unnecessary interventions and prioritize monitoring in appropriately selected patients.
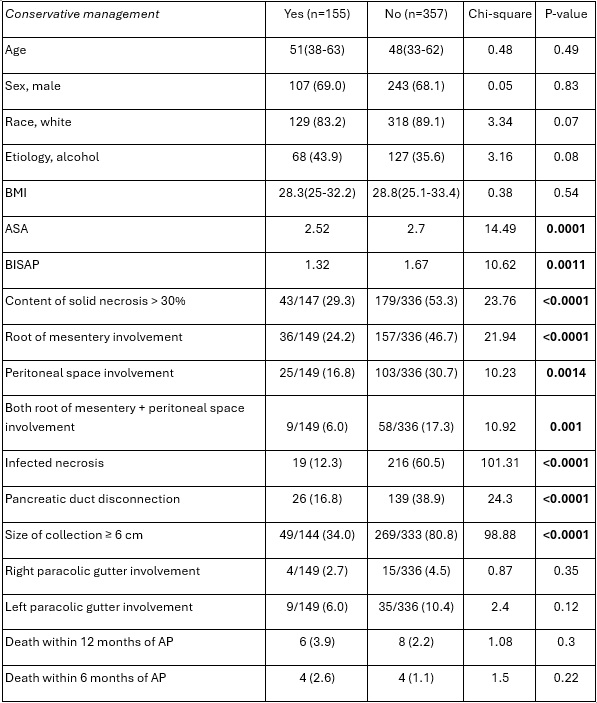
Figure: Table 1. Univariable analysis comparing patients managed conservatively vs. those requiring intervention at any point.
BMI = body mass index; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis, AP = acute pancreatitis.
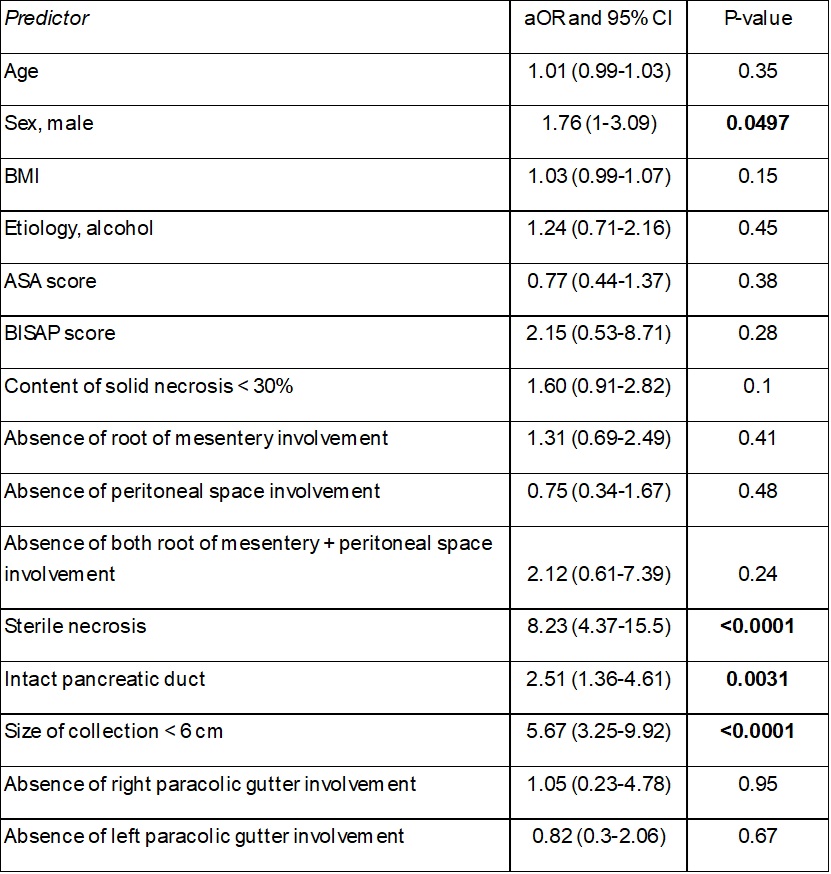
Figure: Table 2. Multivariable analysis of predictors of conservative management during the entire disease course.
aOR = adjusted odds ratio; CI = confidence interval; BMI = body mass index; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis.
Disclosures:
Petr Vanek indicated no relevant financial relationships.
Gaurav Suryawanshi indicated no relevant financial relationships.
Nauroze Faizi indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Petr Vanek, MD, PhD1, Gaurav Suryawanshi, MD2, Nauroze Faizi, MD2, Guru Trikudanathan, MD2. P4346 - Who Really Needs a Drain? Admission Predictors of Successful Conservative Management in Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, USA; Palacky University Olomouc, Olomouc, Czech Republic, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: Although some patients with necrotizing pancreatitis (NP) are managed with a minimally invasive step-up approach, reliable predictors to identify those who can be managed conservatively remain elusive. We analyzed a prospectively maintained NP database to define baseline predictors of a wholly conservative course.
Methods: Adults admitted with NP between 2009 and 2022 were included. Exclusions were lack of follow-up or death during index admission/within 30 days of discharge. Baseline demographic, clinical, and radiologic variables from contrast-enhanced CT performed ≤ 72 h after admission were evaluated. Conservative management was defined as no percutaneous, endoscopic, or surgical intervention during the entire disease course. Univariable associations were tested with χ² test; multivariable logistic regression was adjusted for demographics, disease severity, and imaging covariates.
Results: Of 512 patients, 155 (30%) completed the entire disease course without intervention and 357 (70%) required drainage at some point. In the multivariable model, sterile necrosis (absence of infection) (adjusted odds ratio [aOR] 8.23, 95% CI 4.37–15.5), collection diameter < 6 cm (aOR 5.67, 95% CI 3.25–9.92), and intact pancreatic duct (absence of disconnection) (aOR 2.51, 95% CI 1.36–4.61) independently predicted success of conservative therapy (all p < 0.005). Among the 357 interventionally managed patients, 273 (77%) underwent a procedure during the index admission; early intervention was again associated with infected necrosis, duct disconnection, and larger collections.
Discussion: Three admission findings—sterile necrosis, smaller collection size (< 6 cm), and an intact pancreatic duct—are independent predictors of successful conservative management in NP. Conversely, the presence of just one adverse feature (infected necrosis, a larger collection, or pancreatic duct disconnection) predicts failure of conservative therapy in the majority of patients; in fact, 8 out of 10 such patients will ultimately require interventional treatment. Incorporating these variables into a clinical decision tool may help defer unnecessary interventions and prioritize monitoring in appropriately selected patients.
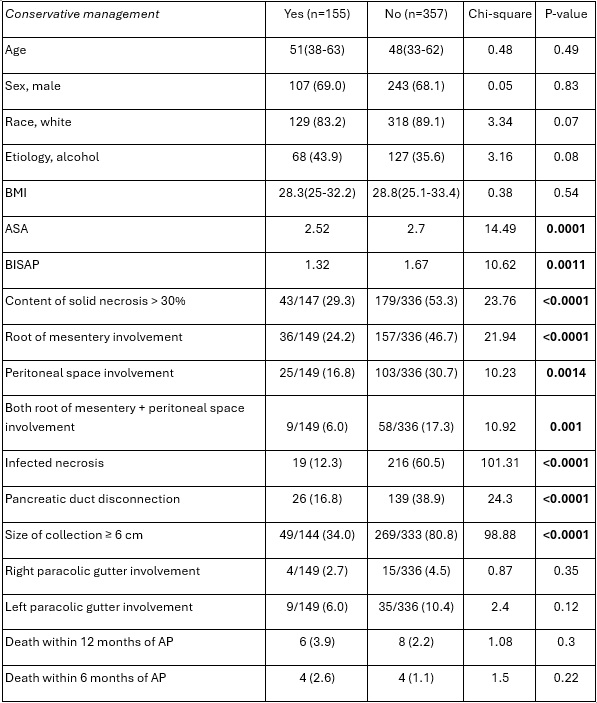
Figure: Table 1. Univariable analysis comparing patients managed conservatively vs. those requiring intervention at any point.
BMI = body mass index; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis, AP = acute pancreatitis.
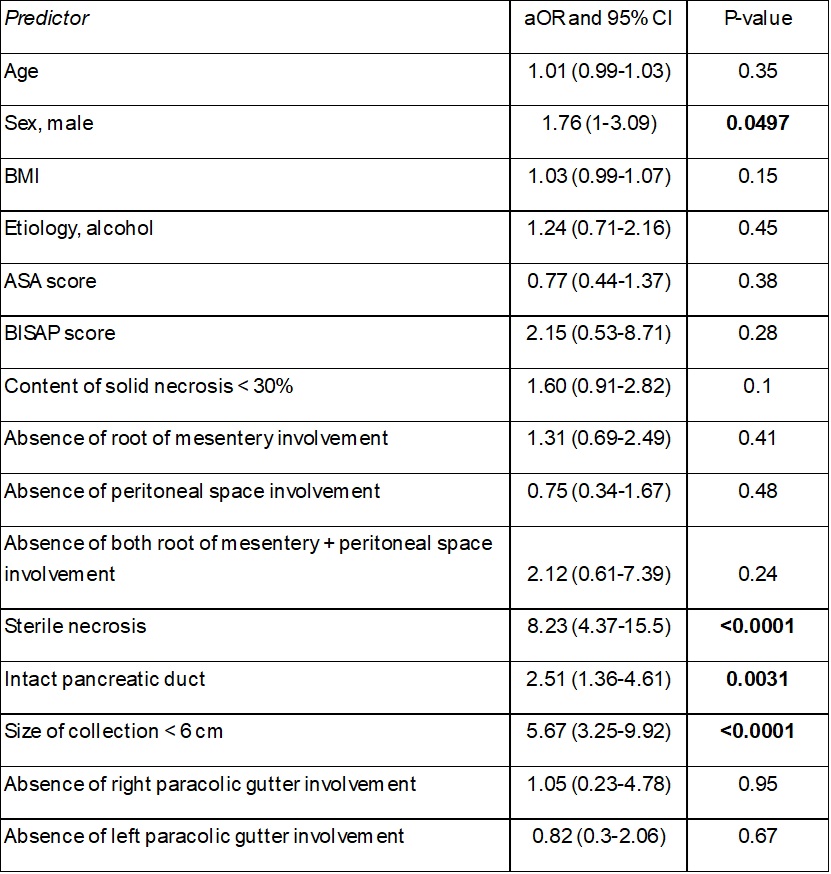
Figure: Table 2. Multivariable analysis of predictors of conservative management during the entire disease course.
aOR = adjusted odds ratio; CI = confidence interval; BMI = body mass index; ASA = American Society of Anesthesiologists physical status classification; BISAP = Bedside Index for Severity in Acute Pancreatitis.
Disclosures:
Petr Vanek indicated no relevant financial relationships.
Gaurav Suryawanshi indicated no relevant financial relationships.
Nauroze Faizi indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Petr Vanek, MD, PhD1, Gaurav Suryawanshi, MD2, Nauroze Faizi, MD2, Guru Trikudanathan, MD2. P4346 - Who Really Needs a Drain? Admission Predictors of Successful Conservative Management in Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
