Tuesday Poster Session
Category: Biliary/Pancreas
P4342 - Potential Impact of Malnutrition on Patients Hospitalized With Pancreatic Pseudocysts: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Adham Obeidat, MD (he/him/his)
presbyterian Hospital
Albuquerque, NM
Presenting Author(s)
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Hareesh K. Gundlapalli, MD2, Jawairia Memon, MD3, Christopher Chang, MD, PhD4
1presbyterian Hospital, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM; 4University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Pancreatic pseudocysts are a common complication of both acute and chronic pancreatitis and are often linked to a complicated clinical course. Despite its high prevalence in this population, malnutrition remains frequently underrecognized. This study aims to assess the association between malnutrition and in-hospital outcomes in patients diagnosed with pancreatic pseudocysts in the context of pancreatitis.
Methods: A retrospective analysis of adult patients hospitalized with the diagnosis of acute and chronic pancreatitis between 2019 and 2021 was conducted using the United States Nationwide Inpatient Sample (NIS) database. Using ICD codes, we identified patients with pancreatic pseudocysts and stratified them based on the presence or absence of malnutrition. We compared demographics and clinical characteristics, as well as in-hospital mortality and other secondary outcomes such as sepsis, respiratory failure (RF), acute kidney injury (AKI), portal venous thrombosis (PVT), hemoperitoneum, abdominal compartment syndrome and length of stay (LOS). Multivariate logistic regression was used to adjust for relevant variables.
Results: A total of 74,756 patients with pancreatitis were identified, of whom 7147 had a concurrent diagnosis of pancreatic pseudocyst. Patients with pancreatic pseudocyst had a longer mean LOS (7.17 vs. 4.99 days) and a higher mean total hospital charges ($76,801.59 vs. $52,192.17). Malnutrition was more prevalent among patients with pancreatic pseudocyst (15.68% vs 7.37%). Additionally, in patients with pancreatic pseudocyst, malnutrition was independently associated with a higher chance of in-hospital mortality (OR 5.23, p< 0.001). It was also associated with increased odds of developing sepsis (OR 2.90, p< 0.001), AKI (OR 2.12, p< 0.001), RF (OR 3.29, p< 0.001), PVT (OR 2.03, p< 0.001), hemoperitoneum (OR 2.42, p=0.004), and abdominal compartment syndrome (OR 3.62, p=0.006). See Table 1.
Discussion: Malnutrition is a prevalent diagnosis in patients with acute and chronic pancreatitis including those with a concurrent diagnosis of pancreatic pseudocyst. Our study showed that malnutrition is a strong and independent predictor of mortality and major in-hospital complications in patients hospitalized with the diagnosis of pancreatic pseudocyst. These findings highlight the importance of early nutritional assessment and timely intervention to reduce complications, lower healthcare utilization, and improve survival in this vulnerable patient population.
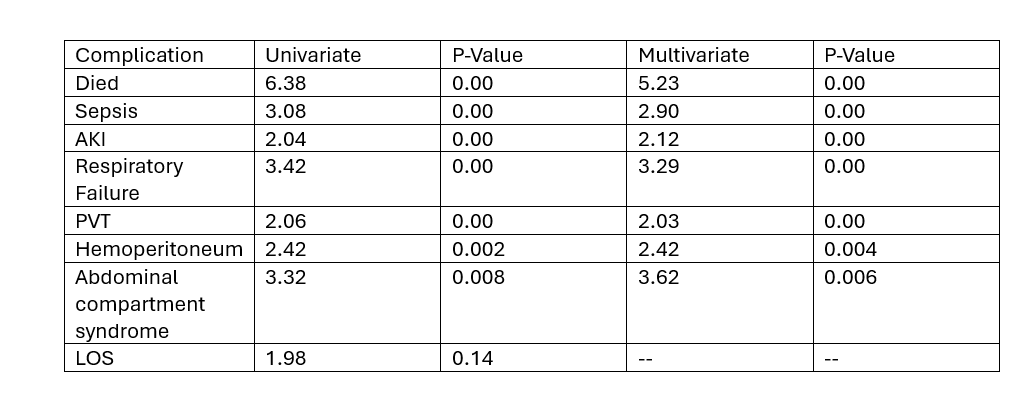
Figure: Table 1. Univariate and Multivariate analysis of malnutrition as a potential predictor of in-hospital complications in patients admitted with pancreatic pseudocyst.
Disclosures:
Adham Obeidat indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Ahmad Abou Yassine indicated no relevant financial relationships.
Hareesh Gundlapalli indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Hareesh K. Gundlapalli, MD2, Jawairia Memon, MD3, Christopher Chang, MD, PhD4. P4342 - Potential Impact of Malnutrition on Patients Hospitalized With Pancreatic Pseudocysts: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1presbyterian Hospital, Albuquerque, NM; 2University of New Mexico, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM; 4University of New Mexico School of Medicine, Albuquerque, NM
Introduction: Pancreatic pseudocysts are a common complication of both acute and chronic pancreatitis and are often linked to a complicated clinical course. Despite its high prevalence in this population, malnutrition remains frequently underrecognized. This study aims to assess the association between malnutrition and in-hospital outcomes in patients diagnosed with pancreatic pseudocysts in the context of pancreatitis.
Methods: A retrospective analysis of adult patients hospitalized with the diagnosis of acute and chronic pancreatitis between 2019 and 2021 was conducted using the United States Nationwide Inpatient Sample (NIS) database. Using ICD codes, we identified patients with pancreatic pseudocysts and stratified them based on the presence or absence of malnutrition. We compared demographics and clinical characteristics, as well as in-hospital mortality and other secondary outcomes such as sepsis, respiratory failure (RF), acute kidney injury (AKI), portal venous thrombosis (PVT), hemoperitoneum, abdominal compartment syndrome and length of stay (LOS). Multivariate logistic regression was used to adjust for relevant variables.
Results: A total of 74,756 patients with pancreatitis were identified, of whom 7147 had a concurrent diagnosis of pancreatic pseudocyst. Patients with pancreatic pseudocyst had a longer mean LOS (7.17 vs. 4.99 days) and a higher mean total hospital charges ($76,801.59 vs. $52,192.17). Malnutrition was more prevalent among patients with pancreatic pseudocyst (15.68% vs 7.37%). Additionally, in patients with pancreatic pseudocyst, malnutrition was independently associated with a higher chance of in-hospital mortality (OR 5.23, p< 0.001). It was also associated with increased odds of developing sepsis (OR 2.90, p< 0.001), AKI (OR 2.12, p< 0.001), RF (OR 3.29, p< 0.001), PVT (OR 2.03, p< 0.001), hemoperitoneum (OR 2.42, p=0.004), and abdominal compartment syndrome (OR 3.62, p=0.006). See Table 1.
Discussion: Malnutrition is a prevalent diagnosis in patients with acute and chronic pancreatitis including those with a concurrent diagnosis of pancreatic pseudocyst. Our study showed that malnutrition is a strong and independent predictor of mortality and major in-hospital complications in patients hospitalized with the diagnosis of pancreatic pseudocyst. These findings highlight the importance of early nutritional assessment and timely intervention to reduce complications, lower healthcare utilization, and improve survival in this vulnerable patient population.
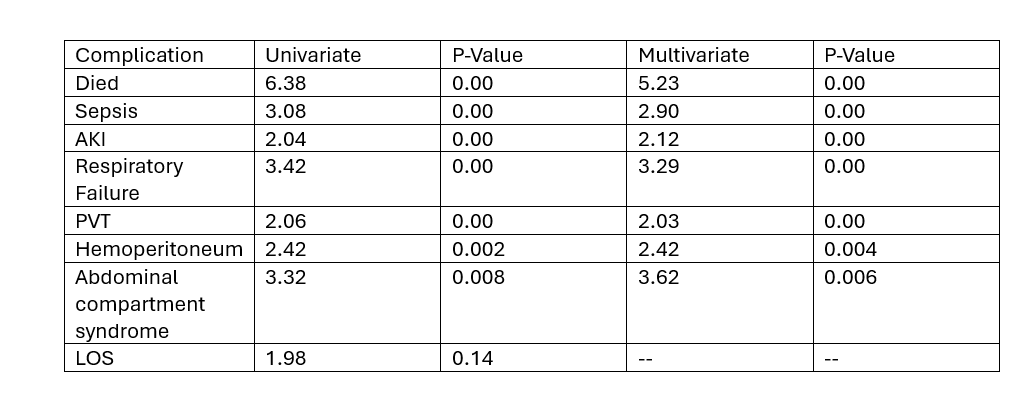
Figure: Table 1. Univariate and Multivariate analysis of malnutrition as a potential predictor of in-hospital complications in patients admitted with pancreatic pseudocyst.
Disclosures:
Adham Obeidat indicated no relevant financial relationships.
Gicel Aguilar indicated no relevant financial relationships.
Ahmad Abou Yassine indicated no relevant financial relationships.
Hareesh Gundlapalli indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
Christopher Chang: Mirum Pharmaceuticals – Advisory Committee/Board Member. Nestle Health – Speakers Bureau. Salix Pharmaceuticals – Advisory Committee/Board Member.
Adham Obeidat, MD1, Gicel J. Aguilar, BS, DO2, Ahmad Abou Yassine, MD2, Hareesh K. Gundlapalli, MD2, Jawairia Memon, MD3, Christopher Chang, MD, PhD4. P4342 - Potential Impact of Malnutrition on Patients Hospitalized With Pancreatic Pseudocysts: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
