Tuesday Poster Session
Category: Biliary/Pancreas
P4340 - Safety and Efficacy of Topical Hemostatic Agents (Powder/Gel) in the Management of Post-Sphincterotomy Bleeding: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PP
Parth Patel, MD
Ascension Saint Joseph Hospital
Chicago, IL
Presenting Author(s)
Parth Patel, MD1, Yordanos Tafesse, MD1, Mohamed A. Ebrahim, MD1, Manav Patel, MD2, Abdelnasir Mohamed, MD1, Ker Patel, MBBS3, Mythili Menon Pathiyil, MD4
1Ascension Saint Joseph Hospital, Chicago, IL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3Government Medical College and Hospital, Chicago, IL; 4Saint Vincent Hospital, Worcester, MA
Introduction: Endoscopic sphincterotomy (EST) and papillectomy are associated with post-procedural bleeding, with rates up to 45.3%. Achieving hemostasis using conventional management (CM) such as epinephrine injection, thermal coagulation, and hemoclips is often challenging due to limited access and maneuverability with the side-viewing duodenoscope. Recently, novel topical agents like PuraStat, a self-assembling peptide-based gel, and hemostatic powders are easier to apply and have emerged as promising alternatives. We conducted a meta-analysis to assess the efficacy and safety of these agents in managing post-sphincterotomy bleeding (PSB).
Methods: A comprehensive search of PubMed, Scopus, Embase, Medline, and Web of Science was conducted through April 2025. Studies reporting safety and efficacy of topical hemostatic agents (gel/powder) for PSB were included. Outcomes analyzed were successful primary hemostasis, delayed bleeding, total procedure time, and adverse event (AE) rates. A random-effects model was used for pooled estimates, and heterogeneity was assessed using I² statistics.
Results: 6 studies were included. 183 patients received either hemostatic gel/powder and 142 patients received CM for PSB. Indications for ERCP included CBD stone, malignant biliary obstruction, biliary drainage, ampullary mass, cholangioscopy and forceps biopsy. Mean PLT count, mean INR value and number of patients receiving anticoagulants / antiplatelet therapy were comparable between the groups. Overall rates of successful primary hemostasis and AE were 98 % and 9% respectively among the patients who received hemostatic powder/gel. Rate of successful primary homeostasis was significantly different between the groups favoring hemostatic powder/gel (OR: 0.22[0.07-0.69]; p=0.01, I2=0%). There was no significant difference in delayed bleeding rates (OR: 02.13[0.74-6.13]; p=0.16, I2=0%), total procedure time (MD: -0.31[-4.44-3.82]; p=0.88, I2=46%) and AE rates (OR: 0.68[0.23-2.06]; p=0.50, I2=0%) between the groups.
Discussion: Topical hemostatic agents are effective and safe alternatives to CM for PSB, offering higher rates of primary hemostasis without increasing delayed bleeding or AE risk. These agents may be a useful alternative to CM in terms of convenience and efficacy. Larger-scale RCTs are needed to better understand the efficacy of these agents—both in comparison to one another and for managing PSB in patients with surgically altered or challenging anatomy.
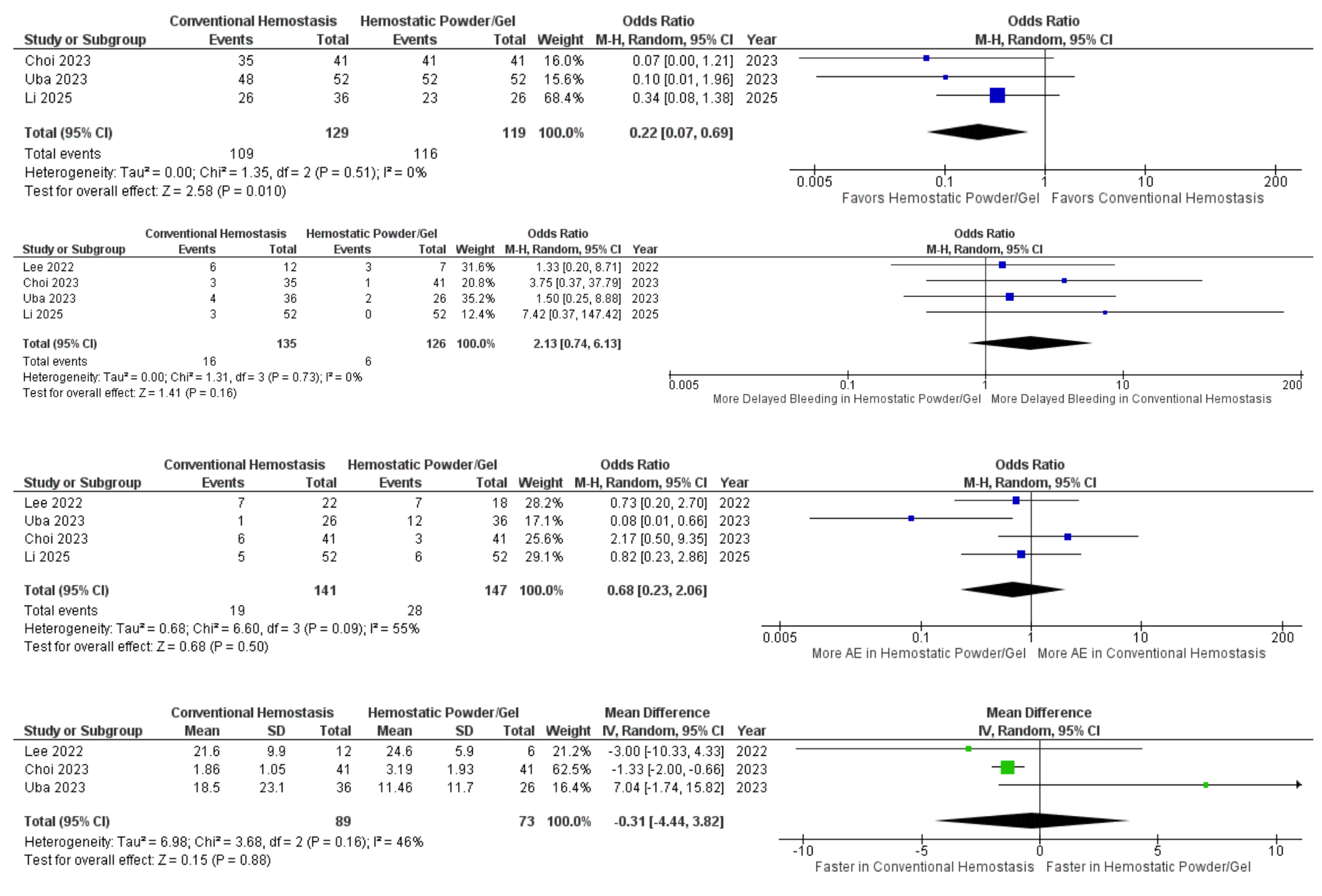
Figure: Forest plots: Comparison of Primary hemostasis, delayed bleeding rate, adverse event rate and total procedure time between two groups
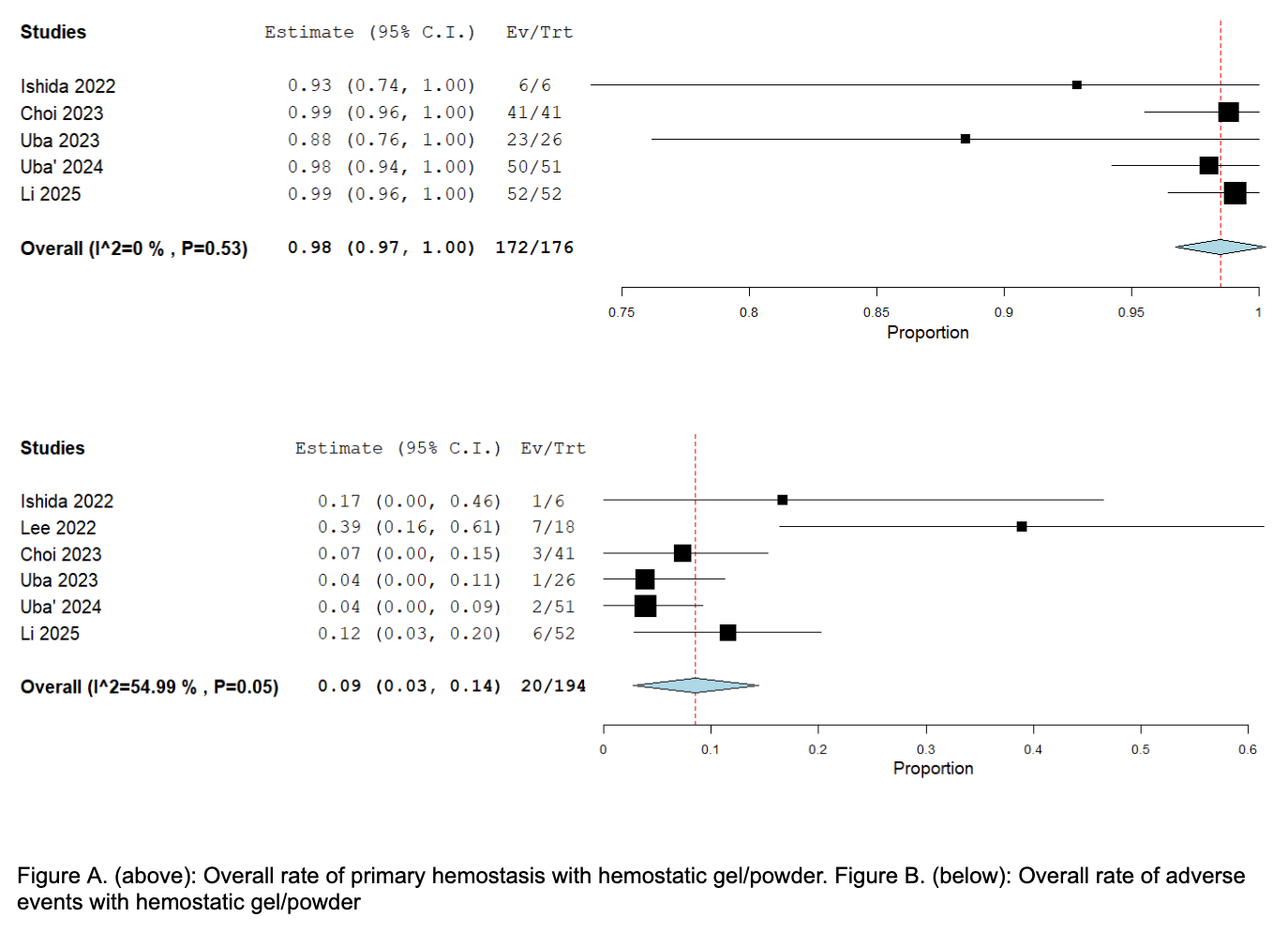
Figure: Figure A. (above): Overall rate of primary hemostasis with hemostatic gel/powder. Figure B. (below): Overall rate of adverse events with hemostatic gel/powder
Disclosures:
Parth Patel indicated no relevant financial relationships.
Yordanos Tafesse indicated no relevant financial relationships.
Mohamed Ebrahim indicated no relevant financial relationships.
Manav Patel indicated no relevant financial relationships.
Abdelnasir Mohamed indicated no relevant financial relationships.
Ker Patel indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Parth Patel, MD1, Yordanos Tafesse, MD1, Mohamed A. Ebrahim, MD1, Manav Patel, MD2, Abdelnasir Mohamed, MD1, Ker Patel, MBBS3, Mythili Menon Pathiyil, MD4. P4340 - Safety and Efficacy of Topical Hemostatic Agents (Powder/Gel) in the Management of Post-Sphincterotomy Bleeding: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ascension Saint Joseph Hospital, Chicago, IL; 2Broward Health Medical Center, Fort Lauderdale, FL; 3Government Medical College and Hospital, Chicago, IL; 4Saint Vincent Hospital, Worcester, MA
Introduction: Endoscopic sphincterotomy (EST) and papillectomy are associated with post-procedural bleeding, with rates up to 45.3%. Achieving hemostasis using conventional management (CM) such as epinephrine injection, thermal coagulation, and hemoclips is often challenging due to limited access and maneuverability with the side-viewing duodenoscope. Recently, novel topical agents like PuraStat, a self-assembling peptide-based gel, and hemostatic powders are easier to apply and have emerged as promising alternatives. We conducted a meta-analysis to assess the efficacy and safety of these agents in managing post-sphincterotomy bleeding (PSB).
Methods: A comprehensive search of PubMed, Scopus, Embase, Medline, and Web of Science was conducted through April 2025. Studies reporting safety and efficacy of topical hemostatic agents (gel/powder) for PSB were included. Outcomes analyzed were successful primary hemostasis, delayed bleeding, total procedure time, and adverse event (AE) rates. A random-effects model was used for pooled estimates, and heterogeneity was assessed using I² statistics.
Results: 6 studies were included. 183 patients received either hemostatic gel/powder and 142 patients received CM for PSB. Indications for ERCP included CBD stone, malignant biliary obstruction, biliary drainage, ampullary mass, cholangioscopy and forceps biopsy. Mean PLT count, mean INR value and number of patients receiving anticoagulants / antiplatelet therapy were comparable between the groups. Overall rates of successful primary hemostasis and AE were 98 % and 9% respectively among the patients who received hemostatic powder/gel. Rate of successful primary homeostasis was significantly different between the groups favoring hemostatic powder/gel (OR: 0.22[0.07-0.69]; p=0.01, I2=0%). There was no significant difference in delayed bleeding rates (OR: 02.13[0.74-6.13]; p=0.16, I2=0%), total procedure time (MD: -0.31[-4.44-3.82]; p=0.88, I2=46%) and AE rates (OR: 0.68[0.23-2.06]; p=0.50, I2=0%) between the groups.
Discussion: Topical hemostatic agents are effective and safe alternatives to CM for PSB, offering higher rates of primary hemostasis without increasing delayed bleeding or AE risk. These agents may be a useful alternative to CM in terms of convenience and efficacy. Larger-scale RCTs are needed to better understand the efficacy of these agents—both in comparison to one another and for managing PSB in patients with surgically altered or challenging anatomy.
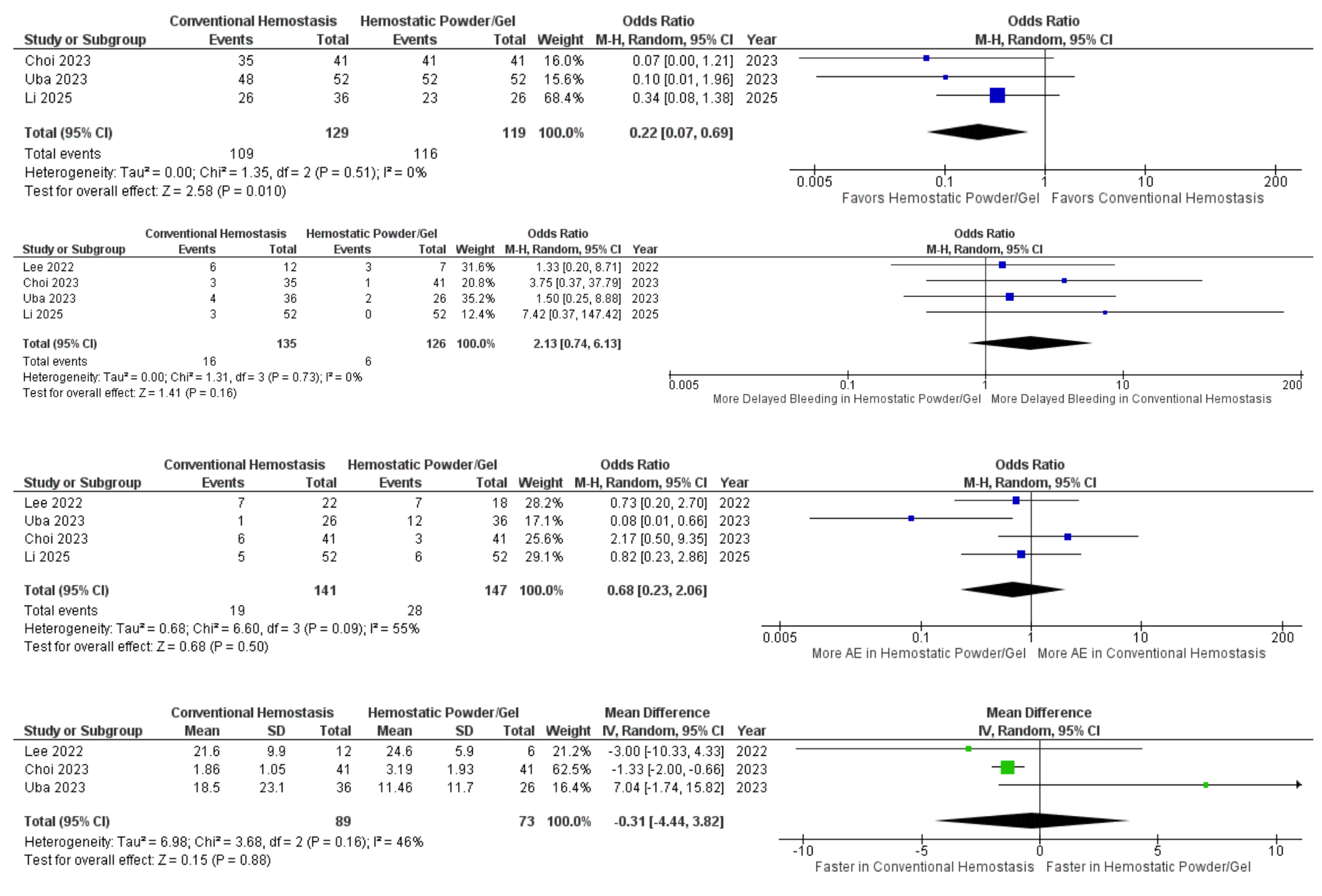
Figure: Forest plots: Comparison of Primary hemostasis, delayed bleeding rate, adverse event rate and total procedure time between two groups
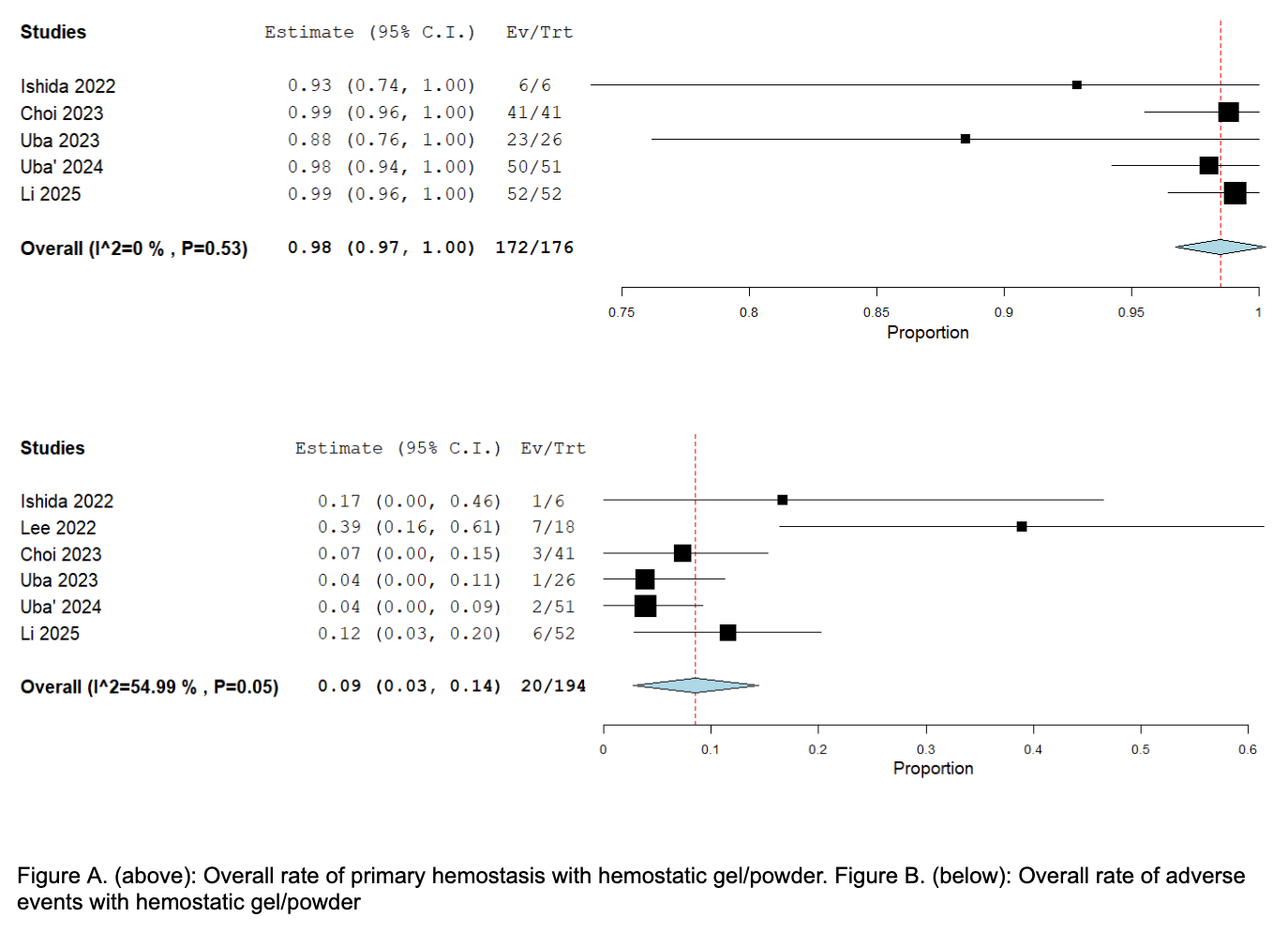
Figure: Figure A. (above): Overall rate of primary hemostasis with hemostatic gel/powder. Figure B. (below): Overall rate of adverse events with hemostatic gel/powder
Disclosures:
Parth Patel indicated no relevant financial relationships.
Yordanos Tafesse indicated no relevant financial relationships.
Mohamed Ebrahim indicated no relevant financial relationships.
Manav Patel indicated no relevant financial relationships.
Abdelnasir Mohamed indicated no relevant financial relationships.
Ker Patel indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Parth Patel, MD1, Yordanos Tafesse, MD1, Mohamed A. Ebrahim, MD1, Manav Patel, MD2, Abdelnasir Mohamed, MD1, Ker Patel, MBBS3, Mythili Menon Pathiyil, MD4. P4340 - Safety and Efficacy of Topical Hemostatic Agents (Powder/Gel) in the Management of Post-Sphincterotomy Bleeding: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
