Tuesday Poster Session
Category: Biliary/Pancreas
P4412 - Pancreatic Masquerade: Recurrent Colon Adenocarcinoma Presenting as a Pancreatic Head Mass With Obstructive Jaundice
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rasheed Musa, MBBS (he/him/his)
East Tennessee State University
Birmingham, AL
Presenting Author(s)
Rasheed Musa, MBBS, Parth Goenka, , Hamza Altal, MD, Patrick Costello, MD, Puneet Goenka, MD
East Tennessee State University, Johnson City, TN
Introduction: Recurrent colorectal adenocarcinoma presenting as a pancreatic head mass with obstructive jaundice is a rare and diagnostically challenging scenario. This case highlights the intricacies of diagnosis, the role of advanced imaging and endoscopy, and the importance of multidisciplinary management in such atypical presentations.
Case Description/
Methods: A 48-year-old female with a history of colon adenocarcinoma (status post-right hemicolectomy and chemotherapy, in remission since 2022) and type 2 diabetes mellitus presented with obstructive jaundice. Initial magnetic resonance imaging (MRI) revealed a pancreatic head mass with a double duct sign. Endoscopic retrograde cholangiopancreatography (ERCP) with biliary stent placement and brushing for cytology, as well as endoscopic ultrasound-guided fine-needle biopsy (EUS-FNB) of the pancreatic head and periportal lymph nodes, yielded negative results for malignancy.
A previously performed surveillance positron emission tomography (PET) for her history of colon cancer demonstrated increased metabolic activity in the pancreatic head without definitive evidence of colorectal cancer recurrence. Serum carcinoembryonic antigen (CEA) was elevated to 23 ng/mL, and carbohydrate antigen 19-9 (CA 19-9) was 532 U/mL. Repeat EUS with FNB on identified poorly differentiated adenocarcinoma with signet ring morphology, consistent with metastatic colonic adenocarcinoma. Repeat CEA was 149 ng/mL, and CA 19-9 exceeded 60,000 U/mL.
The patient was referred to oncology but subsequently re-presented with worsening jaundice and elevated liver enzymes. Imaging demonstrated progressive biliary obstruction. ERCP was unsuccessful due to duodenal luminal narrowing from tumor invasion. EUS-guided hepaticogastrostomy and gastrojejunostomy were successfully performed for biliary decompression and relief of gastric outlet obstruction, respectively. She is now undergoing chemotherapy under oncology care.
Discussion: Despite initial negative diagnostic findings, repeat EUS with FNB confirmed the metastatic nature of the disease. The elevated tumor markers (CEA and CA 19-9) were pivotal in prompting further investigation.
EUS-guided interventions provided effective palliative relief, underscoring their critical role in managing advanced gastrointestinal malignancies with obstructive complications. Early recognition of atypical metastatic patterns and a multidisciplinary approach are essential for optimizing outcomes in similar cases.
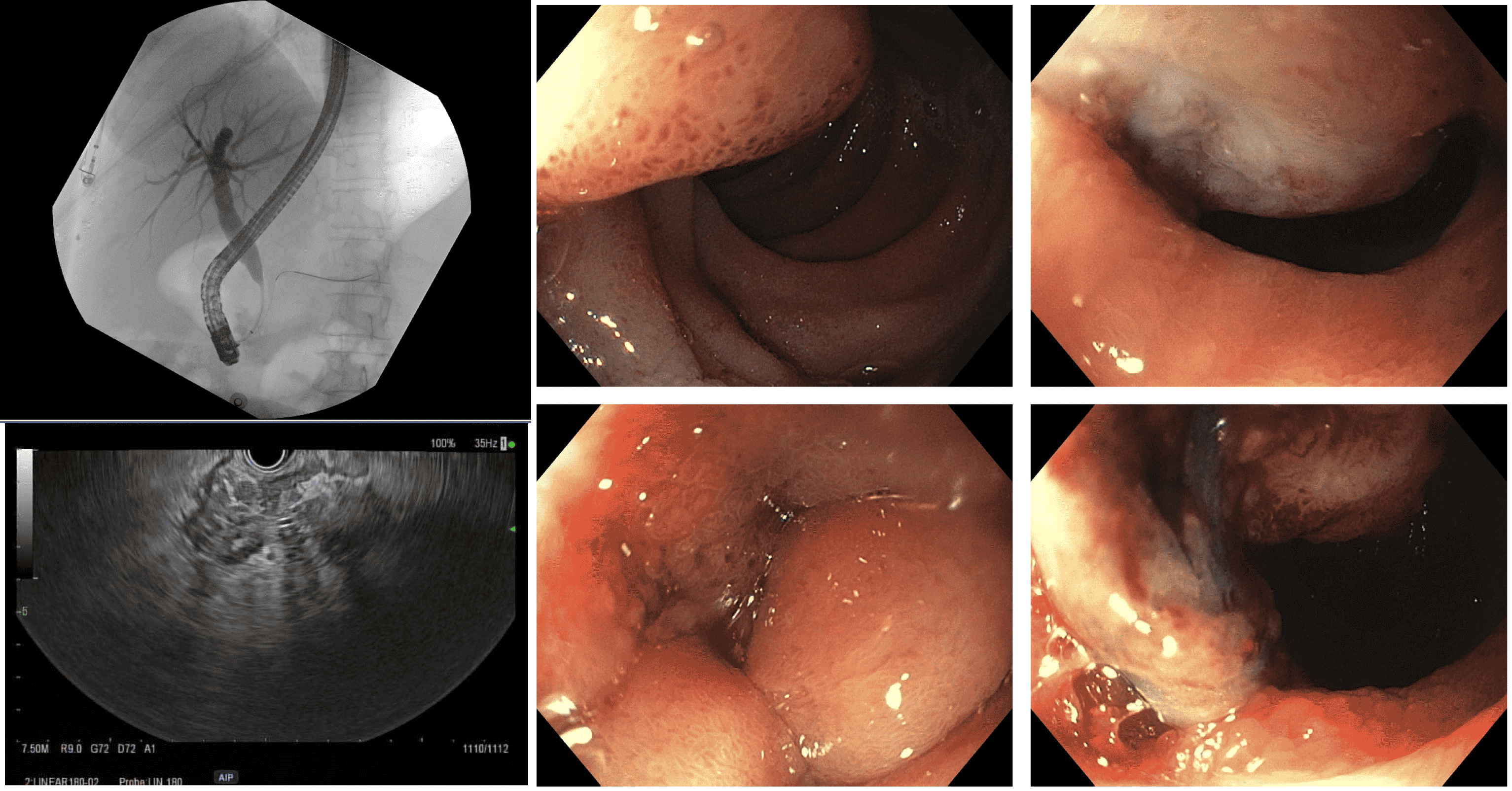
Figure: Endoscopy and fluoroscopy images
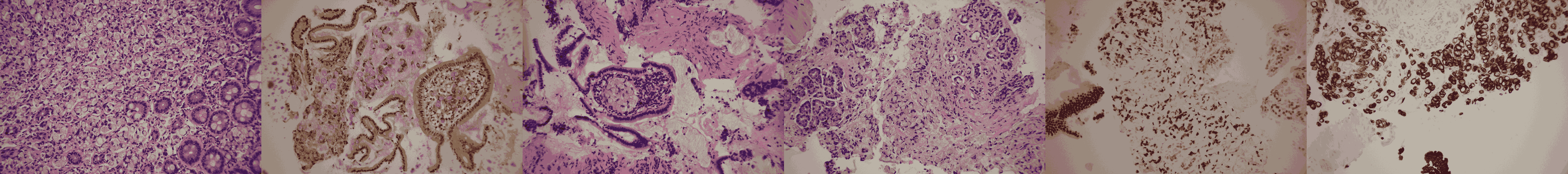
Figure: Pathology slides. respectively:
- Pancreactic FNB showing colon adenocarcinoma with signet ring
- Mucin in signet ring cells
- Intravascular involvement in a duodenal villus (H&E, 200x)
- Signet ring adenocarcinoma infiltrates pancreatic tissue (H&E, 200x)
- Strong CDX2 expression in tumor cells and duodenal epithelium (IHC, 200x)
- Strong CK 20 expression in tumor cells and duodenal epithelium (IHC, 200x)
Disclosures:
Rasheed Musa indicated no relevant financial relationships.
Parth Goenka indicated no relevant financial relationships.
Hamza Altal indicated no relevant financial relationships.
Patrick Costello indicated no relevant financial relationships.
Puneet Goenka indicated no relevant financial relationships.
Rasheed Musa, MBBS, Parth Goenka, , Hamza Altal, MD, Patrick Costello, MD, Puneet Goenka, MD. P4412 - Pancreatic Masquerade: Recurrent Colon Adenocarcinoma Presenting as a Pancreatic Head Mass With Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
East Tennessee State University, Johnson City, TN
Introduction: Recurrent colorectal adenocarcinoma presenting as a pancreatic head mass with obstructive jaundice is a rare and diagnostically challenging scenario. This case highlights the intricacies of diagnosis, the role of advanced imaging and endoscopy, and the importance of multidisciplinary management in such atypical presentations.
Case Description/
Methods: A 48-year-old female with a history of colon adenocarcinoma (status post-right hemicolectomy and chemotherapy, in remission since 2022) and type 2 diabetes mellitus presented with obstructive jaundice. Initial magnetic resonance imaging (MRI) revealed a pancreatic head mass with a double duct sign. Endoscopic retrograde cholangiopancreatography (ERCP) with biliary stent placement and brushing for cytology, as well as endoscopic ultrasound-guided fine-needle biopsy (EUS-FNB) of the pancreatic head and periportal lymph nodes, yielded negative results for malignancy.
A previously performed surveillance positron emission tomography (PET) for her history of colon cancer demonstrated increased metabolic activity in the pancreatic head without definitive evidence of colorectal cancer recurrence. Serum carcinoembryonic antigen (CEA) was elevated to 23 ng/mL, and carbohydrate antigen 19-9 (CA 19-9) was 532 U/mL. Repeat EUS with FNB on identified poorly differentiated adenocarcinoma with signet ring morphology, consistent with metastatic colonic adenocarcinoma. Repeat CEA was 149 ng/mL, and CA 19-9 exceeded 60,000 U/mL.
The patient was referred to oncology but subsequently re-presented with worsening jaundice and elevated liver enzymes. Imaging demonstrated progressive biliary obstruction. ERCP was unsuccessful due to duodenal luminal narrowing from tumor invasion. EUS-guided hepaticogastrostomy and gastrojejunostomy were successfully performed for biliary decompression and relief of gastric outlet obstruction, respectively. She is now undergoing chemotherapy under oncology care.
Discussion: Despite initial negative diagnostic findings, repeat EUS with FNB confirmed the metastatic nature of the disease. The elevated tumor markers (CEA and CA 19-9) were pivotal in prompting further investigation.
EUS-guided interventions provided effective palliative relief, underscoring their critical role in managing advanced gastrointestinal malignancies with obstructive complications. Early recognition of atypical metastatic patterns and a multidisciplinary approach are essential for optimizing outcomes in similar cases.
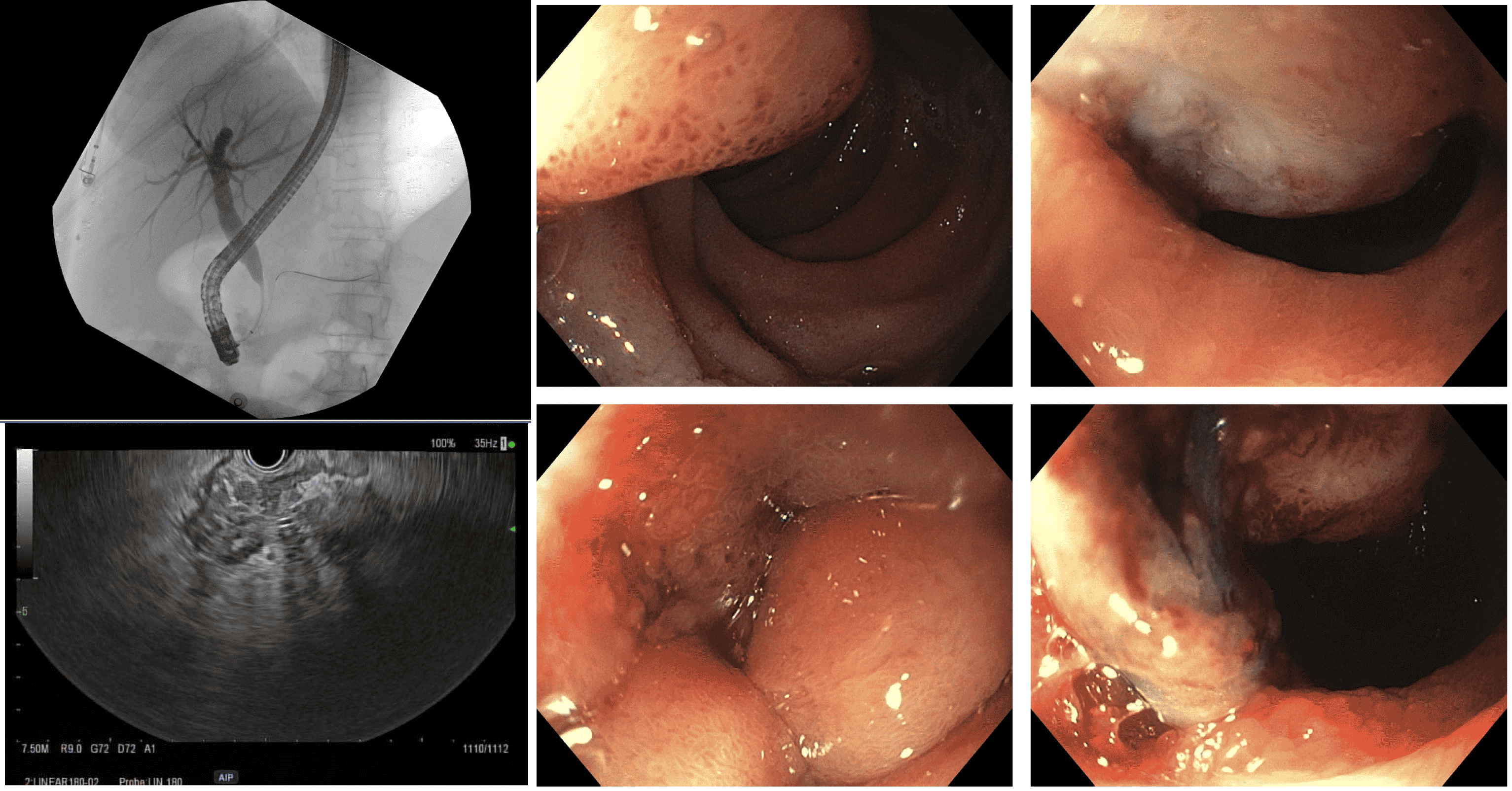
Figure: Endoscopy and fluoroscopy images
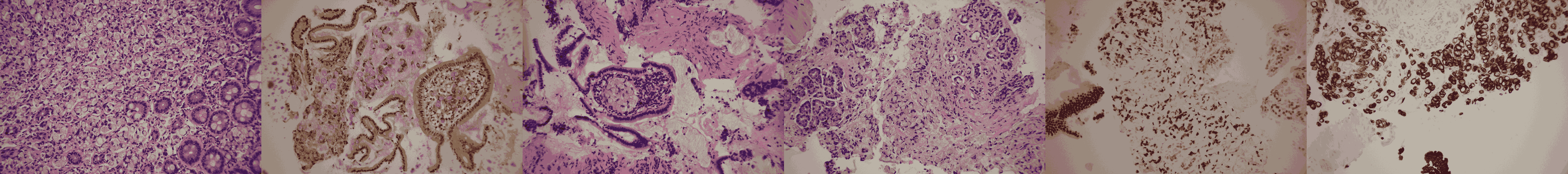
Figure: Pathology slides. respectively:
- Pancreactic FNB showing colon adenocarcinoma with signet ring
- Mucin in signet ring cells
- Intravascular involvement in a duodenal villus (H&E, 200x)
- Signet ring adenocarcinoma infiltrates pancreatic tissue (H&E, 200x)
- Strong CDX2 expression in tumor cells and duodenal epithelium (IHC, 200x)
- Strong CK 20 expression in tumor cells and duodenal epithelium (IHC, 200x)
Disclosures:
Rasheed Musa indicated no relevant financial relationships.
Parth Goenka indicated no relevant financial relationships.
Hamza Altal indicated no relevant financial relationships.
Patrick Costello indicated no relevant financial relationships.
Puneet Goenka indicated no relevant financial relationships.
Rasheed Musa, MBBS, Parth Goenka, , Hamza Altal, MD, Patrick Costello, MD, Puneet Goenka, MD. P4412 - Pancreatic Masquerade: Recurrent Colon Adenocarcinoma Presenting as a Pancreatic Head Mass With Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
