Tuesday Poster Session
Category: Biliary/Pancreas
P4496 - A Case of Duodenal Diverticulitis Mimicking a Choledochal Cyst
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bishoy Gad, MD (he/him/his)
Montefiore Medical Center
Bronx, NY
Presenting Author(s)
Bishoy Gad, MD, Nicholas Costable, MD, Sammy Ho, MD, FACG
Montefiore Medical Center, Bronx, NY
Introduction: Duodenal diverticulitis is a rare complication of the common finding of duodenal diverticulosis. Duodenal diverticula are usually asymptomatic and incidentally found; however, approximately 5% of patients will experience clinically relevant symptomatic duodenal diverticulosis. Complications of duodenal diverticulitis include pancreaticobiliary or duodenal obstruction, perforation, or hemorrhage. Periampullary duodenal diverticulosis may lead to biliary stasis within the distal CBD and obstructive biliary pathology, including choledocholithiasis. While CBD stones are the most common reason for mechanical obstruction, obstruction can also arise from adjacent periampullary diverticulitis. Few cases of this have been described, and they are a rare complication of duodenal diverticulitis.
Case Description/
Methods: A 28-year-old male with one day of epigastric pain, fevers, and vomiting. Initial labs revealed WBC 6.3, AST 722, ALT 609, Alk Phos 187, and T Billi 4.2. CTAP revealed wall thickening and enhancement of the common hepatic duct and central intrahepatic biliary tree with a 2 cm fluid-filled mid-CBD cystic structure. MRI/MRCP showed a prominent CBD measuring up to 1 cm and a 2.4 cm cystic structure subjacent to the midsegment of the CBD, suspicious of a type II choledochal cyst, with concern for superinfection. Initial ERCP revealed an intradiverticular major papilla. The cholangiogram demonstrated underfilling of the mid-bile duct but did not show a choledochal cyst. A biliary sphincterotomy was performed, and no stones were found on subsequent balloon sweeps. A subsequent ERCP with cholangioscopy eleven days later confirmed the absence of choledocholithiasis and choledochal cyst.
Discussion: Acute cholangitis is a rare complication of duodenal diverticulitis, commonly related to choledocholithiasis. This case reveals a rare presentation of acute cholangitis without biliary stones, and thus, from periampullary inflammation. MRI suggested a choledochal cyst, which was not found on cholangiogram. The MRI likely detected the intrapapillary diverticulum and was misinterpreted as a choledochal cyst. Cholangioscopy at repeat ERCP confirmed the absence of a choledochal cyst, greatly changing management and preventing unnecessary surgical excision of the cyst, which is the definitive treatment. The use of cholangioscopy is not common practice for confirmation of biliary pathology in interpapillary duodenal diverticulitis. However, in this case, it likely prevented unnecessary surgery for the patient.
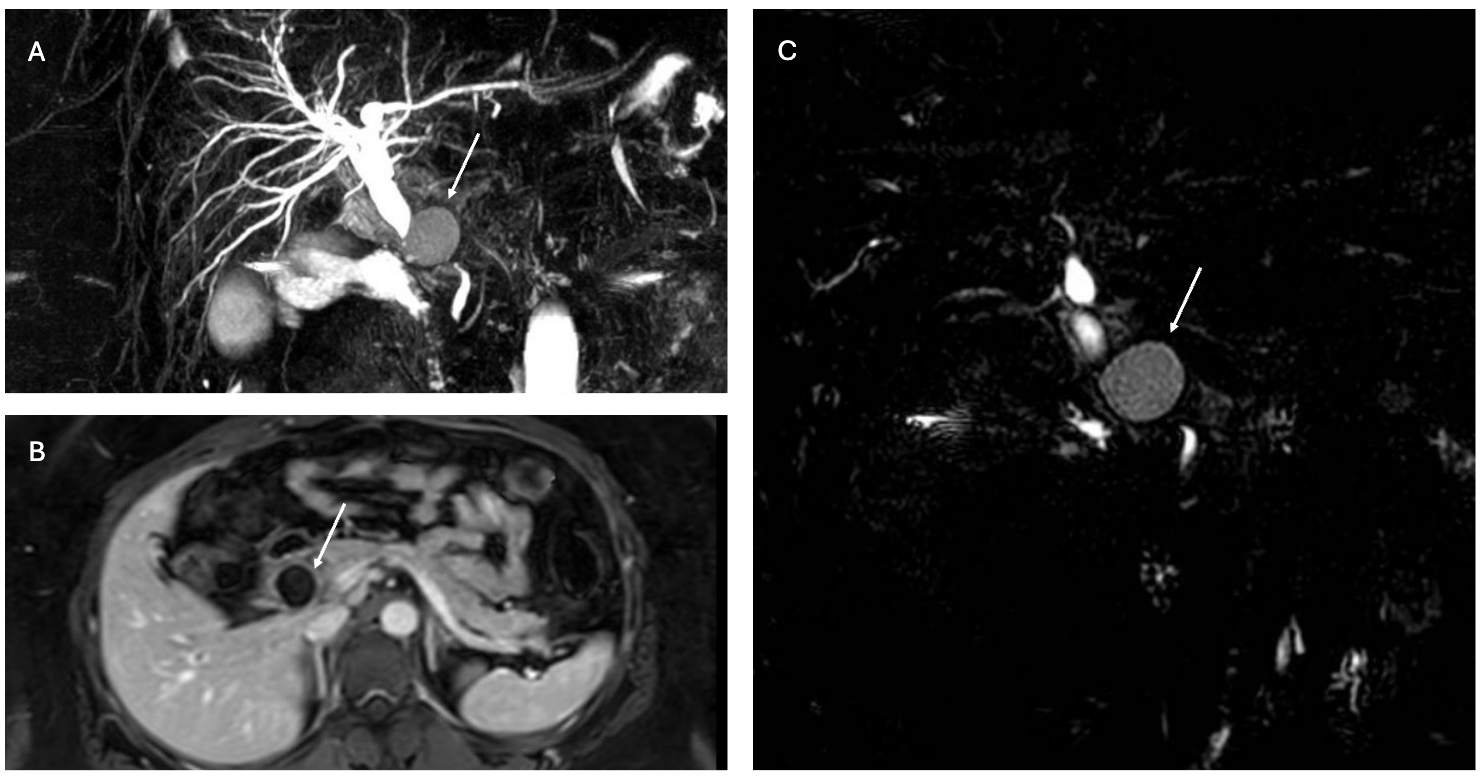
Figure: A-C: MRCP and MRI abdomen Images with outpouching structure foundto be duodenal diverticulum
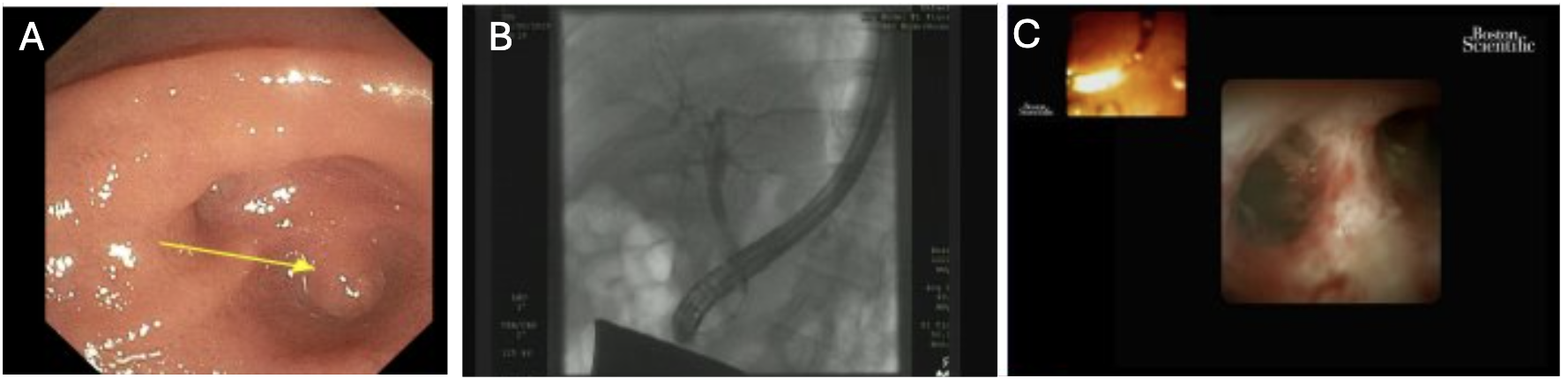
Figure: A- Periampullary diverticulum
B- Original ERCP without choledochal cyst
C- Cholangioscopy (SpyGlass) of CBD without choledochal cyst
Disclosures:
Bishoy Gad indicated no relevant financial relationships.
Nicholas Costable indicated no relevant financial relationships.
Sammy Ho indicated no relevant financial relationships.
Bishoy Gad, MD, Nicholas Costable, MD, Sammy Ho, MD, FACG. P4496 - A Case of Duodenal Diverticulitis Mimicking a Choledochal Cyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Montefiore Medical Center, Bronx, NY
Introduction: Duodenal diverticulitis is a rare complication of the common finding of duodenal diverticulosis. Duodenal diverticula are usually asymptomatic and incidentally found; however, approximately 5% of patients will experience clinically relevant symptomatic duodenal diverticulosis. Complications of duodenal diverticulitis include pancreaticobiliary or duodenal obstruction, perforation, or hemorrhage. Periampullary duodenal diverticulosis may lead to biliary stasis within the distal CBD and obstructive biliary pathology, including choledocholithiasis. While CBD stones are the most common reason for mechanical obstruction, obstruction can also arise from adjacent periampullary diverticulitis. Few cases of this have been described, and they are a rare complication of duodenal diverticulitis.
Case Description/
Methods: A 28-year-old male with one day of epigastric pain, fevers, and vomiting. Initial labs revealed WBC 6.3, AST 722, ALT 609, Alk Phos 187, and T Billi 4.2. CTAP revealed wall thickening and enhancement of the common hepatic duct and central intrahepatic biliary tree with a 2 cm fluid-filled mid-CBD cystic structure. MRI/MRCP showed a prominent CBD measuring up to 1 cm and a 2.4 cm cystic structure subjacent to the midsegment of the CBD, suspicious of a type II choledochal cyst, with concern for superinfection. Initial ERCP revealed an intradiverticular major papilla. The cholangiogram demonstrated underfilling of the mid-bile duct but did not show a choledochal cyst. A biliary sphincterotomy was performed, and no stones were found on subsequent balloon sweeps. A subsequent ERCP with cholangioscopy eleven days later confirmed the absence of choledocholithiasis and choledochal cyst.
Discussion: Acute cholangitis is a rare complication of duodenal diverticulitis, commonly related to choledocholithiasis. This case reveals a rare presentation of acute cholangitis without biliary stones, and thus, from periampullary inflammation. MRI suggested a choledochal cyst, which was not found on cholangiogram. The MRI likely detected the intrapapillary diverticulum and was misinterpreted as a choledochal cyst. Cholangioscopy at repeat ERCP confirmed the absence of a choledochal cyst, greatly changing management and preventing unnecessary surgical excision of the cyst, which is the definitive treatment. The use of cholangioscopy is not common practice for confirmation of biliary pathology in interpapillary duodenal diverticulitis. However, in this case, it likely prevented unnecessary surgery for the patient.
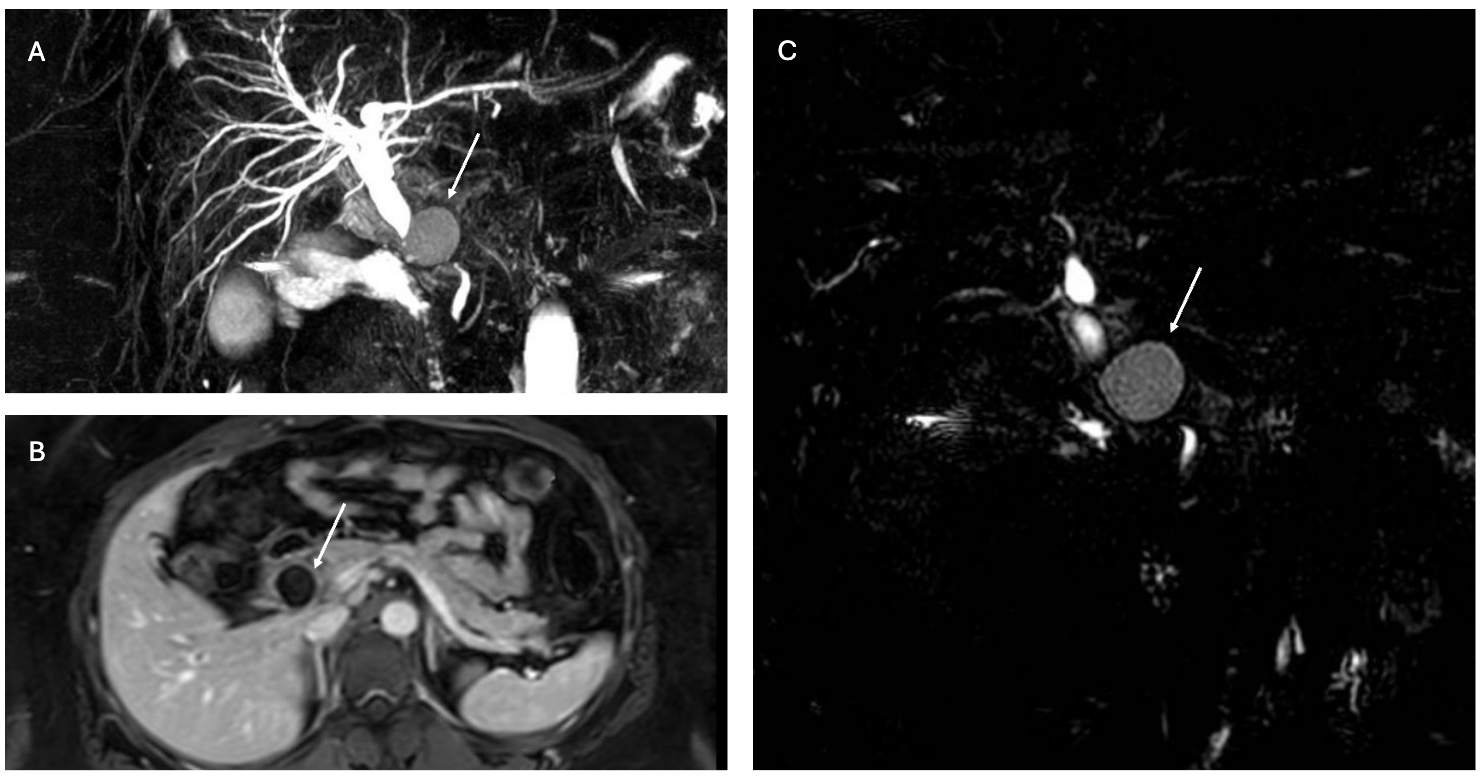
Figure: A-C: MRCP and MRI abdomen Images with outpouching structure foundto be duodenal diverticulum
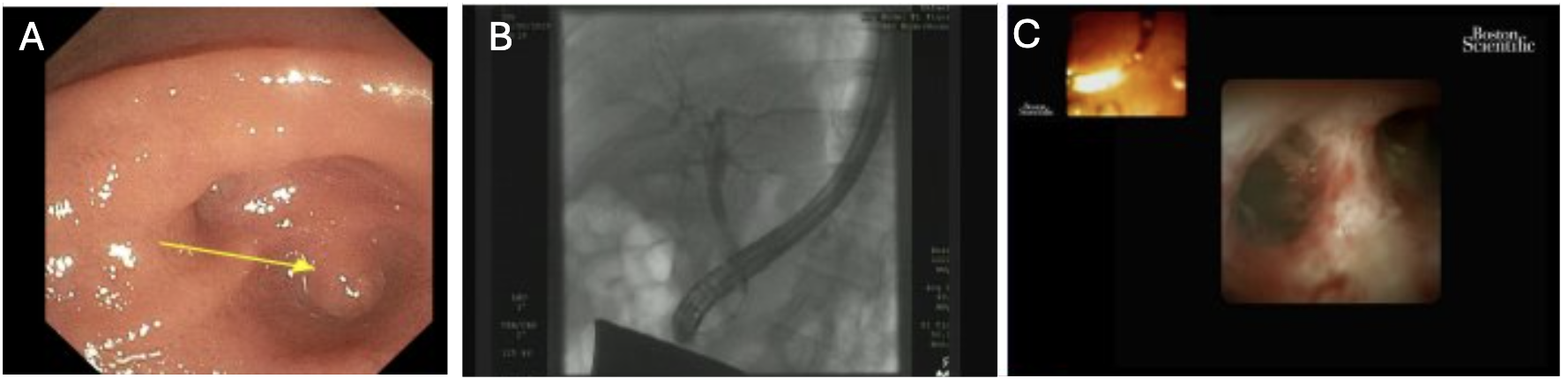
Figure: A- Periampullary diverticulum
B- Original ERCP without choledochal cyst
C- Cholangioscopy (SpyGlass) of CBD without choledochal cyst
Disclosures:
Bishoy Gad indicated no relevant financial relationships.
Nicholas Costable indicated no relevant financial relationships.
Sammy Ho indicated no relevant financial relationships.
Bishoy Gad, MD, Nicholas Costable, MD, Sammy Ho, MD, FACG. P4496 - A Case of Duodenal Diverticulitis Mimicking a Choledochal Cyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
