Tuesday Poster Session
Category: Biliary/Pancreas
P4484 - Bouveret Syndrome in a Patient Without a History of Biliary Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yen Bryan Fong, MD
HonorHealth
Phoenix, AZ
Presenting Author(s)
Yen Bryan Fong, MD1, Shradha Gupta, MD2, Amar Thosani, MD3, Anuj Vyas, MD3
1HonorHealth, Phoenix, AZ; 2HonorHealth, Chandler, AZ; 3HonorHealth, Scottsdale, AZ
Introduction: Bouveret syndrome is a rare form of gallstone ileus characterized by gastric outlet obstruction caused gallstone migration through a cholecystoduodenal/gastric fistula and becoming impacted in the duodenum or pylorus. Gallstone ileus accounts for 1-4% of mechanical bowel obstructions and only around 10% present as Bouveret syndrome.
Case Description/
Methods: A 77-year-old Caucasian female with a past medical history of hypertension presented with emesis and 2 months of sharp, episodic back pain radiating to the left shoulder. Computed tomography (CT) showed inflammation at the gallbladder fossa with a large 2.8 cm stone eroding into the adjacent duodenum. Due to concerns of a cholecystoduodenal fistula the patient underwent endoscopic retrograde cholangiopancreatography (ERCP). On esophagogastroduodenoscopy (EGD), a large stone and 20 mm fistula from the gallbladder to the second portion of the duodenum were seen. The stone was fragmented and cleared using electrohydraulic lithotripsy (EHL) in two successive procedures. The distal duodenum was observed to be patent and the patient was discharged. Four days later the patient presented again with emesis. CT showed a gallstone in the distal ileum, a high-grade small bowel obstruction, and pneumobilia consistent with gallstone ileus. Exploratory laparotomy was performed and a 3x5 cm stone was found to have spontaneously passed into the rectosigmoid junction. No further interventions were indicated and the patient was discharged in a stable condition.
Discussion: This case highlights the challenge the initial diagnosis of Bouveret syndrome and complications after treatment. Females over 60 years and a history of biliary disease are at highest risk. Symptoms lack specificity and can mimic more common causes of gastric outlet obstruction thus leading to diagnostic and management delays resulting in a high morbidity and mortality rate that is estimated to be 12-30%. Labs are non-specific and CT remains the most reliable diagnostic modality. Bowel obstruction, aberrant gallstone, and pneumobilia seen on radiography (Rigler’s triad) strongly suggests Bouveret Syndrome. Recommended management with minimally invasive techniques via endoscopy has a lower mortality and morbidity rate compared to surgery but a comparatively reduced rate of success. As endoscopic treatment techniques and tools continue to improve, this disparity may be reduced. A high index of clinical suspicion is essential for timely diagnosis and intervention, thereby improving outcomes.
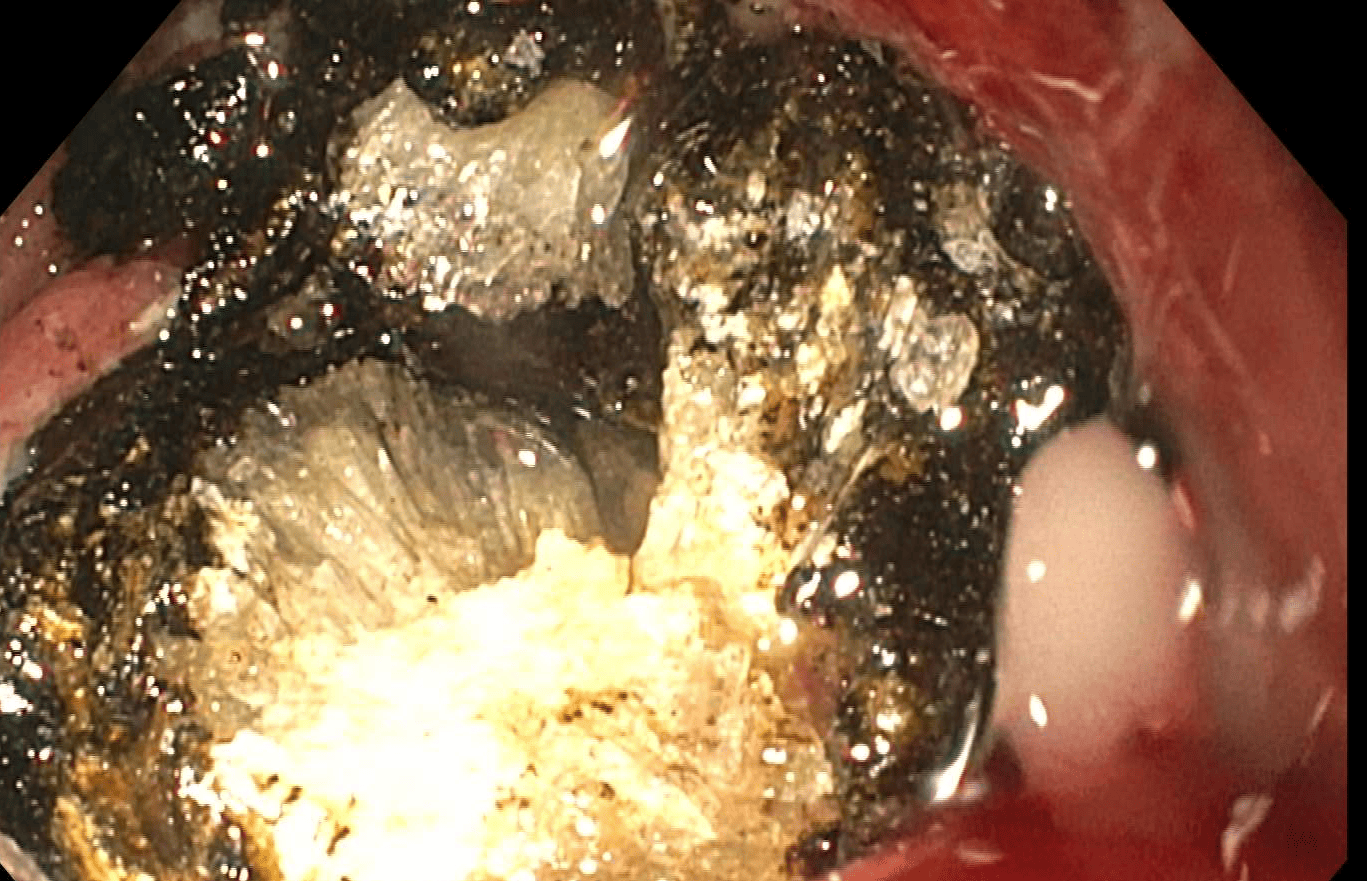
Figure: Gallstone seen in the duodenal bulb on CT abdomen pelvis with contrast.
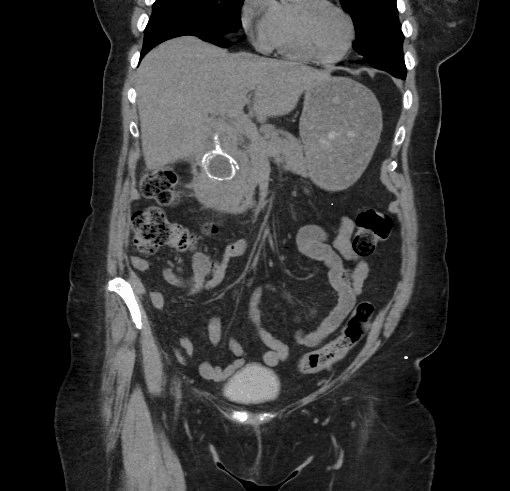
Figure: Endoscopic visualization of gallstone impacting duodenal bulb.
Disclosures:
Yen Bryan Fong indicated no relevant financial relationships.
Shradha Gupta indicated no relevant financial relationships.
Amar Thosani indicated no relevant financial relationships.
Anuj Vyas indicated no relevant financial relationships.
Yen Bryan Fong, MD1, Shradha Gupta, MD2, Amar Thosani, MD3, Anuj Vyas, MD3. P4484 - Bouveret Syndrome in a Patient Without a History of Biliary Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HonorHealth, Phoenix, AZ; 2HonorHealth, Chandler, AZ; 3HonorHealth, Scottsdale, AZ
Introduction: Bouveret syndrome is a rare form of gallstone ileus characterized by gastric outlet obstruction caused gallstone migration through a cholecystoduodenal/gastric fistula and becoming impacted in the duodenum or pylorus. Gallstone ileus accounts for 1-4% of mechanical bowel obstructions and only around 10% present as Bouveret syndrome.
Case Description/
Methods: A 77-year-old Caucasian female with a past medical history of hypertension presented with emesis and 2 months of sharp, episodic back pain radiating to the left shoulder. Computed tomography (CT) showed inflammation at the gallbladder fossa with a large 2.8 cm stone eroding into the adjacent duodenum. Due to concerns of a cholecystoduodenal fistula the patient underwent endoscopic retrograde cholangiopancreatography (ERCP). On esophagogastroduodenoscopy (EGD), a large stone and 20 mm fistula from the gallbladder to the second portion of the duodenum were seen. The stone was fragmented and cleared using electrohydraulic lithotripsy (EHL) in two successive procedures. The distal duodenum was observed to be patent and the patient was discharged. Four days later the patient presented again with emesis. CT showed a gallstone in the distal ileum, a high-grade small bowel obstruction, and pneumobilia consistent with gallstone ileus. Exploratory laparotomy was performed and a 3x5 cm stone was found to have spontaneously passed into the rectosigmoid junction. No further interventions were indicated and the patient was discharged in a stable condition.
Discussion: This case highlights the challenge the initial diagnosis of Bouveret syndrome and complications after treatment. Females over 60 years and a history of biliary disease are at highest risk. Symptoms lack specificity and can mimic more common causes of gastric outlet obstruction thus leading to diagnostic and management delays resulting in a high morbidity and mortality rate that is estimated to be 12-30%. Labs are non-specific and CT remains the most reliable diagnostic modality. Bowel obstruction, aberrant gallstone, and pneumobilia seen on radiography (Rigler’s triad) strongly suggests Bouveret Syndrome. Recommended management with minimally invasive techniques via endoscopy has a lower mortality and morbidity rate compared to surgery but a comparatively reduced rate of success. As endoscopic treatment techniques and tools continue to improve, this disparity may be reduced. A high index of clinical suspicion is essential for timely diagnosis and intervention, thereby improving outcomes.
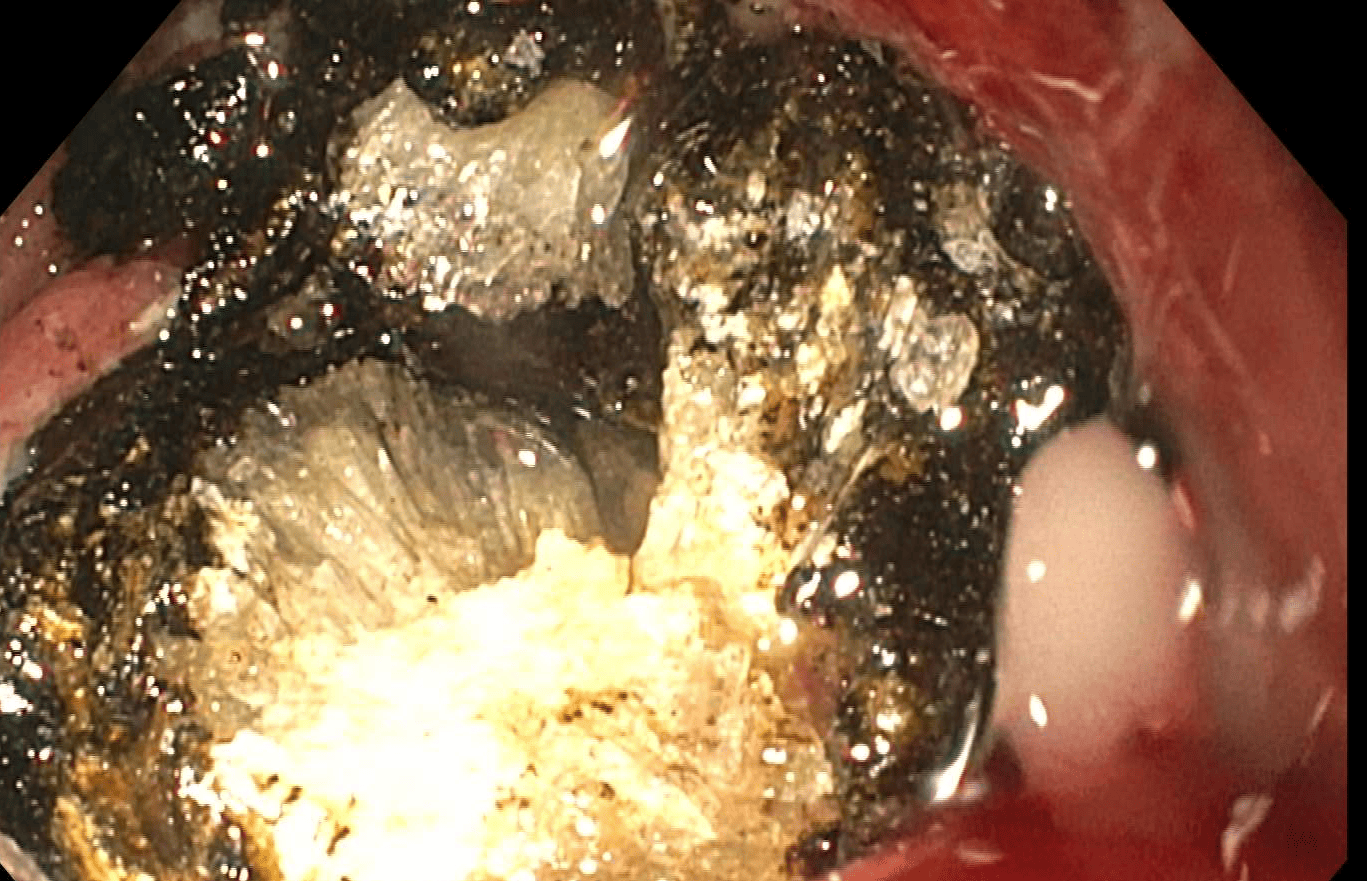
Figure: Gallstone seen in the duodenal bulb on CT abdomen pelvis with contrast.
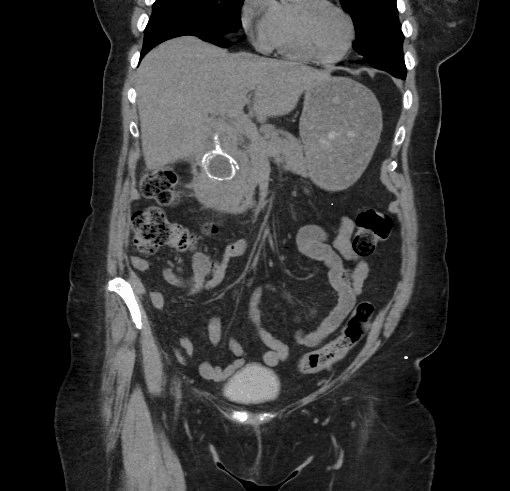
Figure: Endoscopic visualization of gallstone impacting duodenal bulb.
Disclosures:
Yen Bryan Fong indicated no relevant financial relationships.
Shradha Gupta indicated no relevant financial relationships.
Amar Thosani indicated no relevant financial relationships.
Anuj Vyas indicated no relevant financial relationships.
Yen Bryan Fong, MD1, Shradha Gupta, MD2, Amar Thosani, MD3, Anuj Vyas, MD3. P4484 - Bouveret Syndrome in a Patient Without a History of Biliary Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

