Tuesday Poster Session
Category: Biliary/Pancreas
P4479 - From Pancreatic Malignancy to Chronic Pancreatitis: A Rapidly Evolving Case of Colonic Obstruction
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Oleksandr Shumeiko, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Oleksandr Shumeiko, MD1, Sue Dong, MD1, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Sushma Venugopal, MD2, Suresh Nayudu, MD2, Nithan Narendra, MD2
1Brooklyn Hospital Center, Brooklyn, NY; 2SBH Health System, Bronx, NY
Introduction: Pancreatic masses associated with bowel obstruction raise immediate concern for malignancy. However, chronic pancreatitis can occasionally present with similar radiologic and clinical findings.
Case Description/
Methods: A 45-year-old male with a history of hypertension, hyperlipidemia, alcohol-induced hepatitis, and chronic pancreatitis presented with nausea, vomiting, diarrhea, and over 20 pounds of unintentional weight loss. Initial CT imaging revealed a 6 cm mass near the pancreatic tail, inseparable from the splenic flexure, causing large bowel obstruction. The mass appeared to involve the gastric wall and left adrenal gland, raising suspicion for pancreatic adenocarcinoma.
Colonoscopy revealed multiple inflammatory polyps. Biopsies were benign and did not explain the obstructive symptoms. Comparison with a CT from 4 months prior, which showed no mass, highlighted rapid interval development. Subsequent MRI demonstrated low T2 signal intensity in the pancreatic tail and surrounding fibrosis, without pancreatic duct dilation. Imaging raised suspicion for chronic pancreatitis with extensive fibrosis rather than neoplasm. However, due to continued clinical concern and obstructive symptoms, the patient underwent left hemicolectomy and transverse colostomy.
Intraoperatively, the mass was fibrotic and involved the pancreas, stomach, colon, and adrenal gland. Pathology confirmed chronic pancreatitis with fibrosis and no evidence of malignancy. The colonic polyps were inflammatory and non-dysplastic on pathology.
Discussion: This case highlights the diagnostic complexity of differentiating chronic pancreatitis from pancreatic malignancy. The rapid progression and mass effect initially favored a neoplastic process. However, advanced imaging techniques and histopathologic evaluation ultimately confirmed benign inflammatory disease.
The case underscores the limitations of cross-sectional imaging in isolation, particularly in patients with underlying pancreatic disease. MRI and MRCP provided critical clues suggestive of fibrosis rather than malignancy. Surgical exploration and pathology were ultimately required for definitive diagnosis.
In patients with chronic pancreatitis, rapidly evolving pancreatic masses can mimic malignancy both clinically and radiographically. This case reinforces the need for a comprehensive diagnostic approach, including prior imaging comparison, endoscopy, and advanced imaging modalities, to avoid unnecessary surgical interventions and optimize patient outcomes.
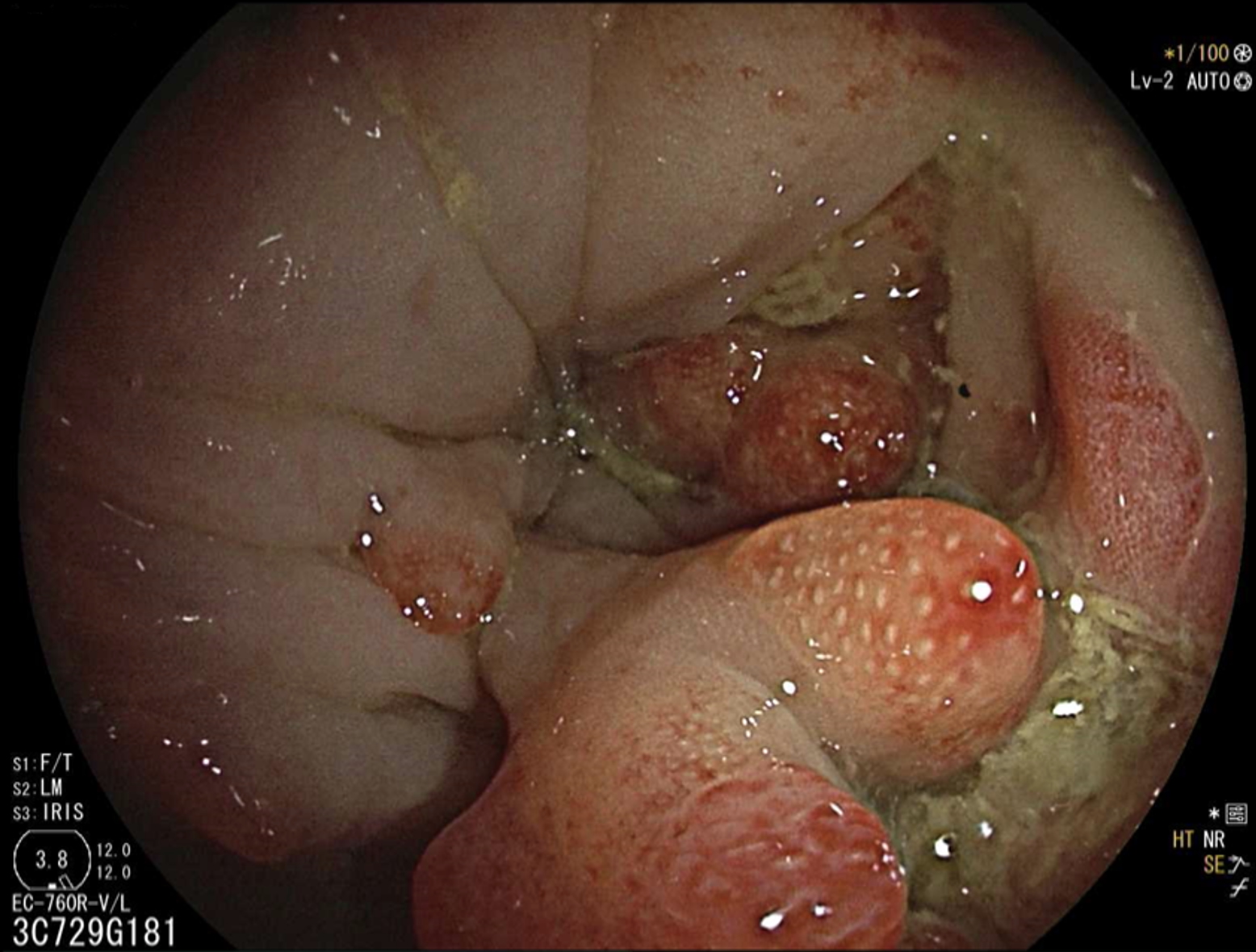
Figure: Figure 1: Polypoid Mass at Splenic Flexure

Figure: Figure 2. MRI with low T2 signal in the pancreatic tail and surrounding fibrosis, suggesting scarring and chronic pancreatitis rather than a neoplastic process
Disclosures:
Oleksandr Shumeiko indicated no relevant financial relationships.
Sue Dong indicated no relevant financial relationships.
Raissa Nana Sede Mbakop Forlemu indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Sushma Venugopal indicated no relevant financial relationships.
Suresh Nayudu indicated no relevant financial relationships.
Nithan Narendra indicated no relevant financial relationships.
Oleksandr Shumeiko, MD1, Sue Dong, MD1, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Sushma Venugopal, MD2, Suresh Nayudu, MD2, Nithan Narendra, MD2. P4479 - From Pancreatic Malignancy to Chronic Pancreatitis: A Rapidly Evolving Case of Colonic Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2SBH Health System, Bronx, NY
Introduction: Pancreatic masses associated with bowel obstruction raise immediate concern for malignancy. However, chronic pancreatitis can occasionally present with similar radiologic and clinical findings.
Case Description/
Methods: A 45-year-old male with a history of hypertension, hyperlipidemia, alcohol-induced hepatitis, and chronic pancreatitis presented with nausea, vomiting, diarrhea, and over 20 pounds of unintentional weight loss. Initial CT imaging revealed a 6 cm mass near the pancreatic tail, inseparable from the splenic flexure, causing large bowel obstruction. The mass appeared to involve the gastric wall and left adrenal gland, raising suspicion for pancreatic adenocarcinoma.
Colonoscopy revealed multiple inflammatory polyps. Biopsies were benign and did not explain the obstructive symptoms. Comparison with a CT from 4 months prior, which showed no mass, highlighted rapid interval development. Subsequent MRI demonstrated low T2 signal intensity in the pancreatic tail and surrounding fibrosis, without pancreatic duct dilation. Imaging raised suspicion for chronic pancreatitis with extensive fibrosis rather than neoplasm. However, due to continued clinical concern and obstructive symptoms, the patient underwent left hemicolectomy and transverse colostomy.
Intraoperatively, the mass was fibrotic and involved the pancreas, stomach, colon, and adrenal gland. Pathology confirmed chronic pancreatitis with fibrosis and no evidence of malignancy. The colonic polyps were inflammatory and non-dysplastic on pathology.
Discussion: This case highlights the diagnostic complexity of differentiating chronic pancreatitis from pancreatic malignancy. The rapid progression and mass effect initially favored a neoplastic process. However, advanced imaging techniques and histopathologic evaluation ultimately confirmed benign inflammatory disease.
The case underscores the limitations of cross-sectional imaging in isolation, particularly in patients with underlying pancreatic disease. MRI and MRCP provided critical clues suggestive of fibrosis rather than malignancy. Surgical exploration and pathology were ultimately required for definitive diagnosis.
In patients with chronic pancreatitis, rapidly evolving pancreatic masses can mimic malignancy both clinically and radiographically. This case reinforces the need for a comprehensive diagnostic approach, including prior imaging comparison, endoscopy, and advanced imaging modalities, to avoid unnecessary surgical interventions and optimize patient outcomes.
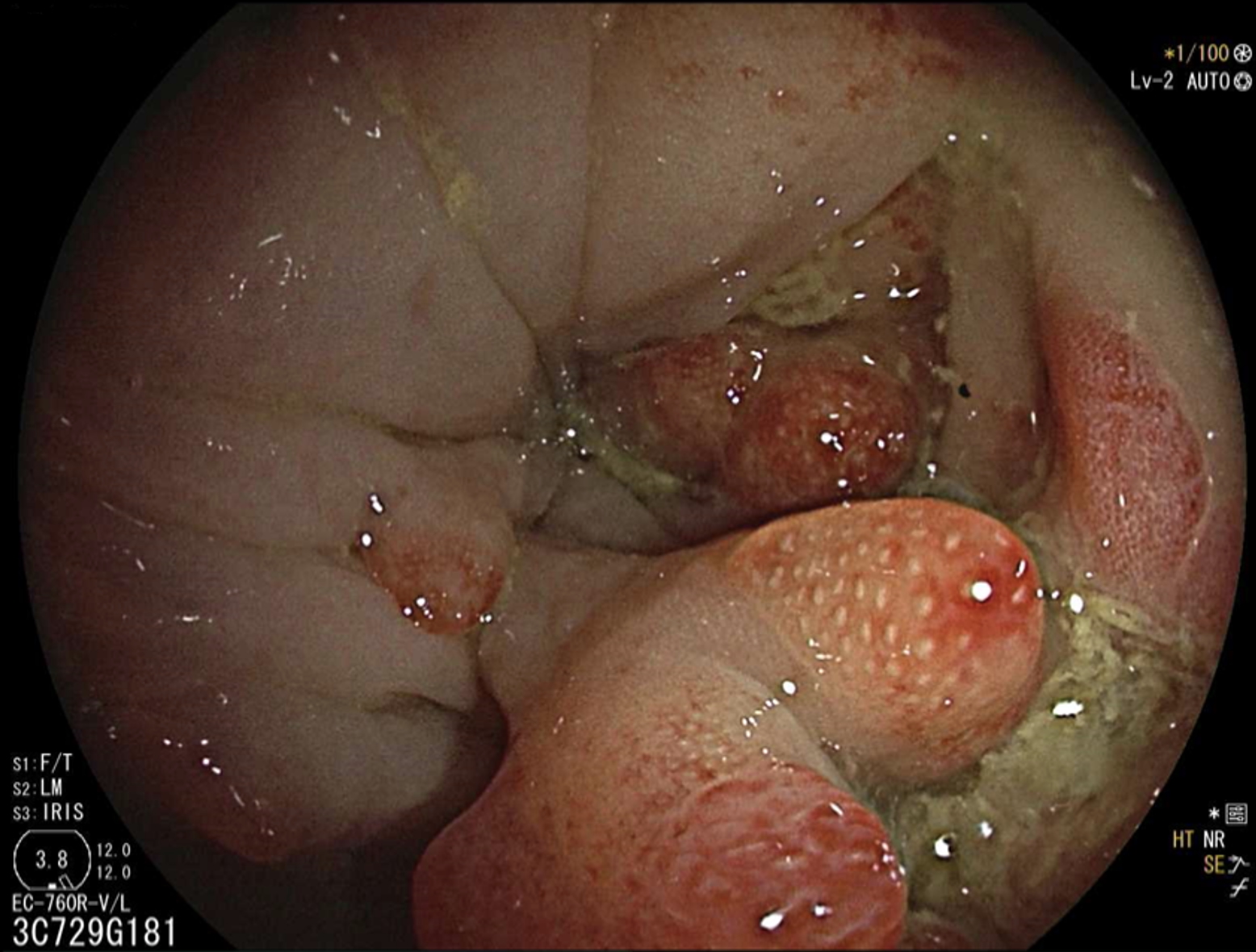
Figure: Figure 1: Polypoid Mass at Splenic Flexure

Figure: Figure 2. MRI with low T2 signal in the pancreatic tail and surrounding fibrosis, suggesting scarring and chronic pancreatitis rather than a neoplastic process
Disclosures:
Oleksandr Shumeiko indicated no relevant financial relationships.
Sue Dong indicated no relevant financial relationships.
Raissa Nana Sede Mbakop Forlemu indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Sushma Venugopal indicated no relevant financial relationships.
Suresh Nayudu indicated no relevant financial relationships.
Nithan Narendra indicated no relevant financial relationships.
Oleksandr Shumeiko, MD1, Sue Dong, MD1, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Sushma Venugopal, MD2, Suresh Nayudu, MD2, Nithan Narendra, MD2. P4479 - From Pancreatic Malignancy to Chronic Pancreatitis: A Rapidly Evolving Case of Colonic Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
