Tuesday Poster Session
Category: Colon
P4602 - Intestinal Spirochetosis in an Immunocompetent Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Serena Brosten, MD (she/her/hers)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Serena Brosten, MD1, Rahul Karna, MD2, Ahmad Malli, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Hennepin Healthcare, Minneapolis, MN
Introduction: Intestinal spirochetosis is a rare and poorly understood infection in which non-treponemal spirochetes attach to the surface epithelium of the colonic mucosa. Its prevalence ranges from 1.1 to 5% in developed countries. When symptomatic, intestinal spirochetosis can cause chronic watery diarrhea and generalized abdominal pain in immunocompromised patients. Here, we report an unusual case of symptomatic intestinal spirochetosis found during screening colonoscopy in an immunocompetent patient.
Case Description/
Methods: A 40-year-old healthy male with a history of six months of waxing and waning diarrhea presented for endoscopic evaluation. Review of systems was negative for weight loss, appetite changes, or blood per rectum. Physical exam and laboratory evaluation were unremarkable. Esophagogastroduodenoscopy and colonoscopy were performed with grossly normal findings and random colon biopsies were taken. Histopathology of the colonic mucosa showed a blue fringe on the surface of the epithelium on H&E staining (Fig. A and B). This finding has been termed a “false brush border” and is pathognomonic for intestinal spirochetosis. The immunohistochemical stain for Treponema pallidum identifies other intestinal spirochetes through cross-reactivity. With this stain, the microorganisms are highlighted at the apical surface of the epithelium of the colon (Fig. C and D). Due to the discovery of intestinal spirochetosis, HIV testing was performed which was negative. Of note, this patient was not immunosuppressed. Due to his ongoing symptoms, it was decided to treat the organism with metronidazole 500mg QID for 10 days. At his one-month follow-up, he reported an improvement in his diarrhea. The sexual orientation of this patient was homosexual.
Discussion: We report a patient with symptomatic intestinal spirochetosis found on random colon biopsy and treated successfully with antibiotics. Our case reinforces the need for random colon biopsies in apparently normal looking colonic mucosa in symptomatic patients.
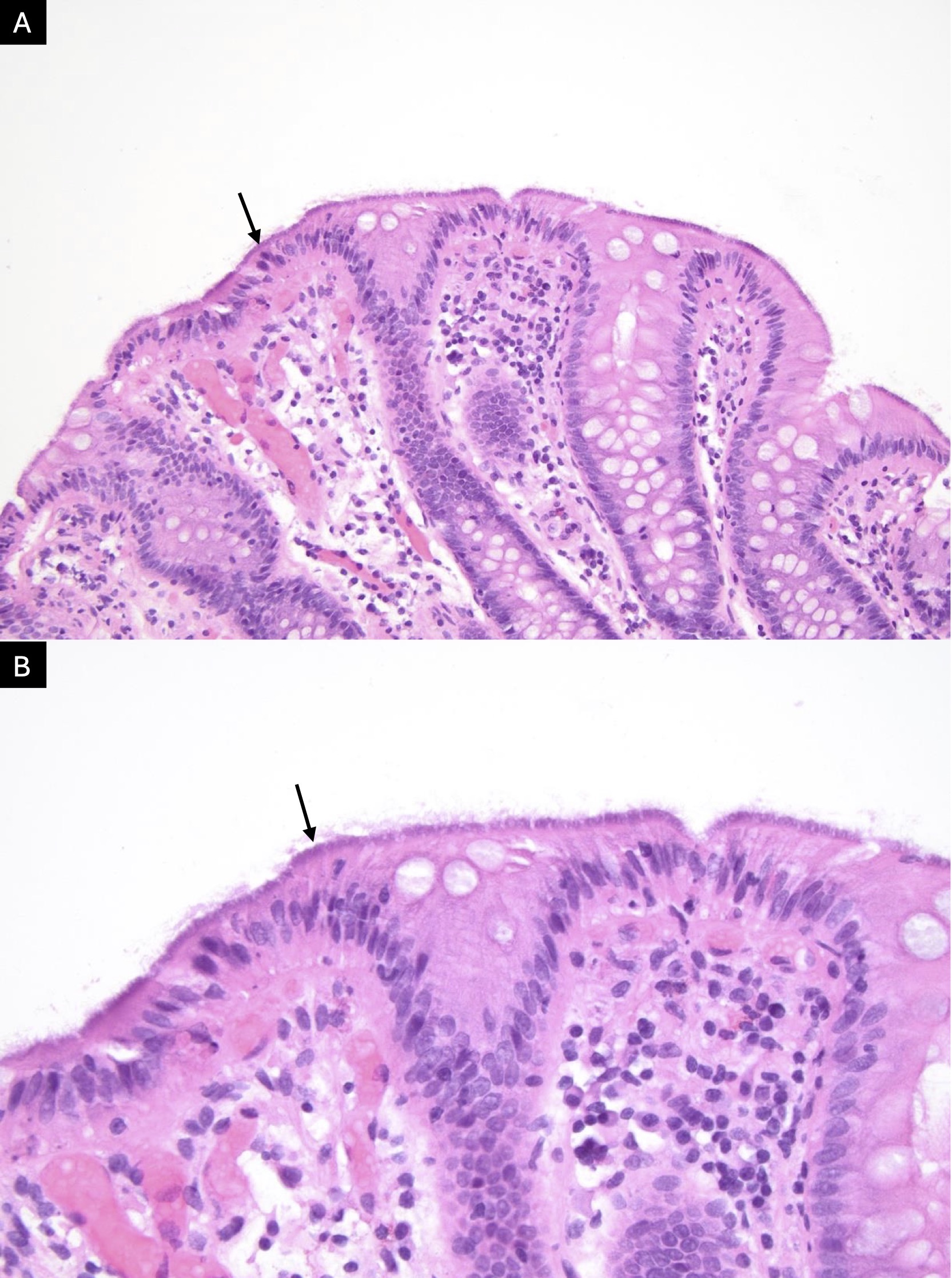
Figure: H&E staining at 20x and 40x magnification of colonic mucosa shows the characteristic blue fringe seen in intestinal spirochetosis
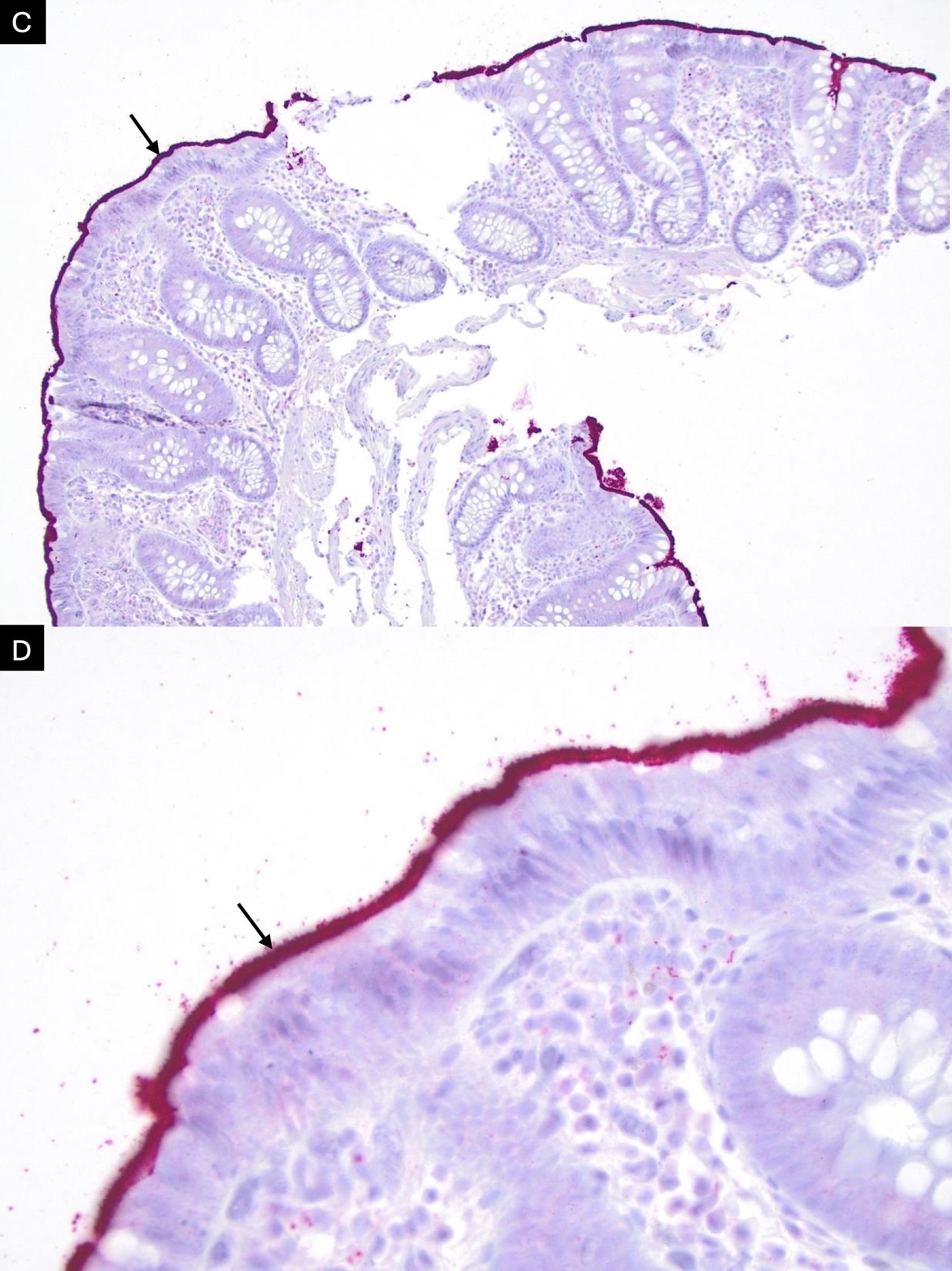
Figure: The Treponema pallidum stain highlights the microorganisms at the apical surface of the colonic mucosa at 10x and 40x magnification
Disclosures:
Serena Brosten indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Ahmad Malli indicated no relevant financial relationships.
Serena Brosten, MD1, Rahul Karna, MD2, Ahmad Malli, MD3. P4602 - Intestinal Spirochetosis in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3Hennepin Healthcare, Minneapolis, MN
Introduction: Intestinal spirochetosis is a rare and poorly understood infection in which non-treponemal spirochetes attach to the surface epithelium of the colonic mucosa. Its prevalence ranges from 1.1 to 5% in developed countries. When symptomatic, intestinal spirochetosis can cause chronic watery diarrhea and generalized abdominal pain in immunocompromised patients. Here, we report an unusual case of symptomatic intestinal spirochetosis found during screening colonoscopy in an immunocompetent patient.
Case Description/
Methods: A 40-year-old healthy male with a history of six months of waxing and waning diarrhea presented for endoscopic evaluation. Review of systems was negative for weight loss, appetite changes, or blood per rectum. Physical exam and laboratory evaluation were unremarkable. Esophagogastroduodenoscopy and colonoscopy were performed with grossly normal findings and random colon biopsies were taken. Histopathology of the colonic mucosa showed a blue fringe on the surface of the epithelium on H&E staining (Fig. A and B). This finding has been termed a “false brush border” and is pathognomonic for intestinal spirochetosis. The immunohistochemical stain for Treponema pallidum identifies other intestinal spirochetes through cross-reactivity. With this stain, the microorganisms are highlighted at the apical surface of the epithelium of the colon (Fig. C and D). Due to the discovery of intestinal spirochetosis, HIV testing was performed which was negative. Of note, this patient was not immunosuppressed. Due to his ongoing symptoms, it was decided to treat the organism with metronidazole 500mg QID for 10 days. At his one-month follow-up, he reported an improvement in his diarrhea. The sexual orientation of this patient was homosexual.
Discussion: We report a patient with symptomatic intestinal spirochetosis found on random colon biopsy and treated successfully with antibiotics. Our case reinforces the need for random colon biopsies in apparently normal looking colonic mucosa in symptomatic patients.
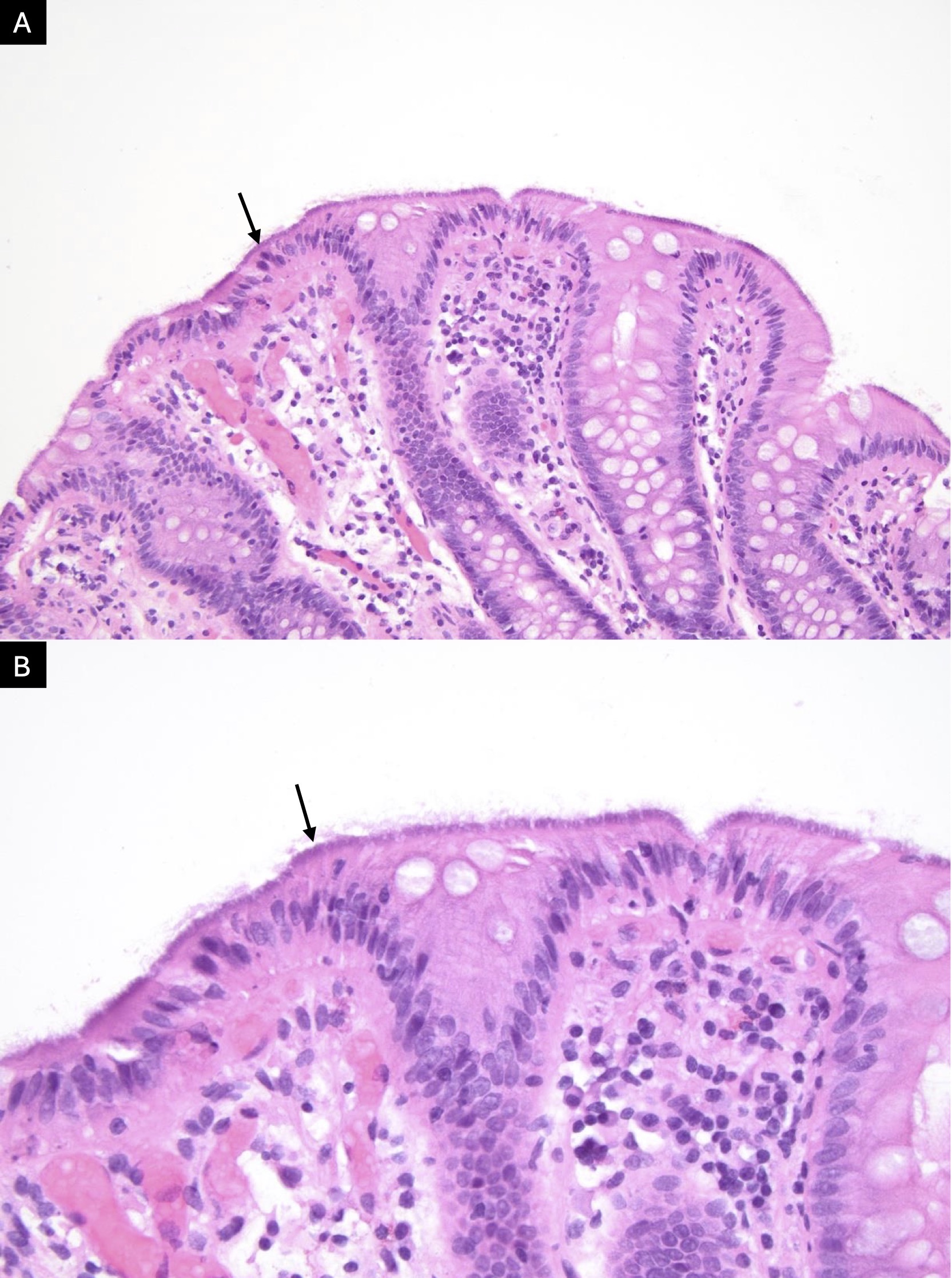
Figure: H&E staining at 20x and 40x magnification of colonic mucosa shows the characteristic blue fringe seen in intestinal spirochetosis
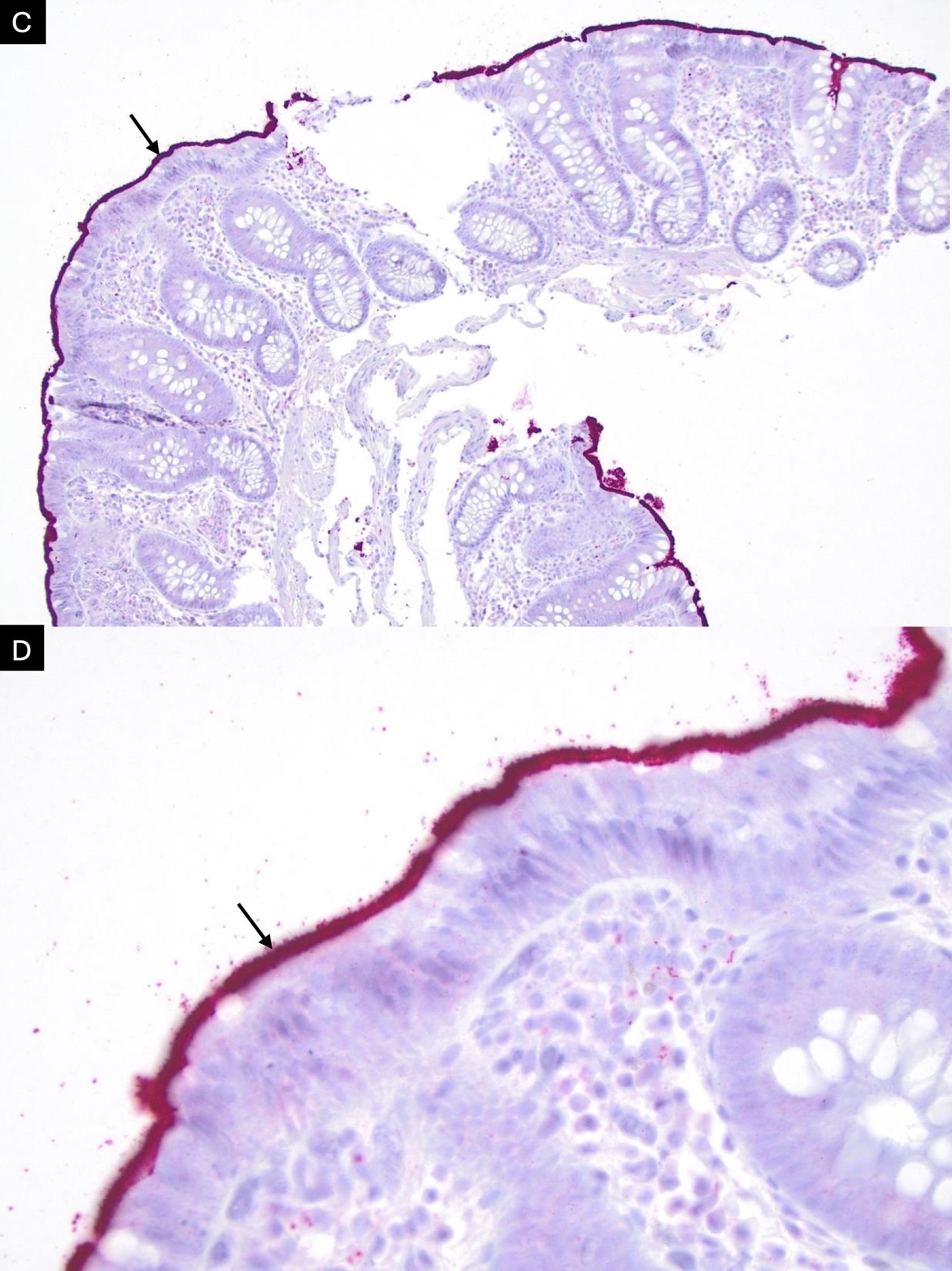
Figure: The Treponema pallidum stain highlights the microorganisms at the apical surface of the colonic mucosa at 10x and 40x magnification
Disclosures:
Serena Brosten indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Ahmad Malli indicated no relevant financial relationships.
Serena Brosten, MD1, Rahul Karna, MD2, Ahmad Malli, MD3. P4602 - Intestinal Spirochetosis in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

