Tuesday Poster Session
Category: Colon
P4675 - Colon Under Pressure: A Case of Colonic Varix
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Monica Arora, DO (she/her/hers)
Mather Hospital, Northwell Health
Port Jefferson, NY
Presenting Author(s)
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Fatimah Spall, DO3, Neva Castro, MD4
1Mather Hospital, Northwell Health, Port Jefferson, NY; 2Northwell Health/Mather Hospital, Port Jefferson, NY; 3Mather Hospital, Zucker School of Medicine at Hofstra University, Port Jefferson, NY; 4Northwell Health, Setauket, NY
Introduction: Ectopic varices, large portosystemic venous collaterals located outside the gastroesophageal region (including colonic, rectal, and gonadal varices), pose a unique challenge. These account for 1–5% of variceal bleeds. Colonic varices can present with lower gastrointestinal bleeding and are identified through endoscopic or imaging investigations. Definitive guidelines are lacking for ectopic varices due to the varied locations and presentations.
Case Description/
Methods: A 59-year-old male with alcohol cirrhosis, grade 1 esophageal varices presented with acute hematochezia and melena. Symptoms included a 40-pound weight loss over 3 years, dry heaving, and vague abdominal pain. Vitals stable. Physical exam notable for tender epigastric region to palpation. Laboratory findings hemoglobin of 6.5, platelets 111, total bilirubin 5.5, direct bilirubin 2.9, AST 71, ALT 23, and alkaline phosphatase 171, INR 1.57, Creatinine 0.68. MELD 21. CTAP showed cirrhosis, portal hypertension, esophageal varices, splenorenal shunt with a venous aneurysm, and additional portal venous collaterals (superior mesenteric vein draining to the gonadal vein) noted in the right side of the abdomen some of which are inseparable from the wall of the ascending colon. Upper endoscopy did not reveal source of bleeding. Colonoscopy revealed bright red blood with clots up to the transverse colon, large, grade 3 colonic varices were identified in the ascending colon (Figure B), Non-bleeding rectal varices and hemorrhoids. Hospital course complicated by hematochezia and anemia, requiring 7 units of packed red blood cells (PRBCs). He was started on an octreotide drip and transferred to a liver transplant center for sclerotherapy and embolization of colonic varices prior to Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement.
Discussion: A review of 169 ectopic variceal bleeding cases revealed ectopic varices in the duodenum (17%), jejunum or ileum (17%), colon (14%), rectum (8%), and peritoneum (9%).
Management of ectopic varices with medications like octreotide remains uncertain. Endoscopy management includes band ligation, endoscopic sclerotherapy, or glue injection. Other alternatives include Balloon-occluded retrograde transvenous obliteration (BRTO) and Percutaneous transhepatic obliteration (PTO). The recommended approach for effective bleeding management involves a combination of TIPS and embolization.
In our patient, the management plan involved sclerotherapy and TIPS with a long-term goal of a liver transplant.
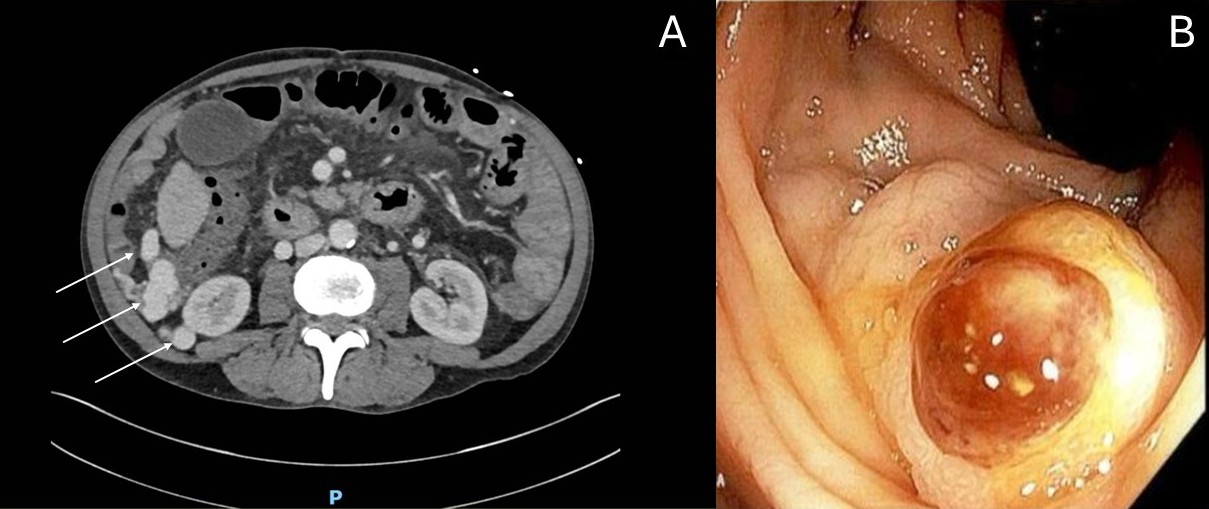
Figure: Figure A: CT Abdomen Pelvis revealed varices involving the ascending colon (white arrows). The vessels are adjacent to the ascending colon. There is no fat plane on imaging, making the varices inseparable from the colon.
Figure B: Large, grade 3 colonic varix identified in the ascending colon.
Disclosures:
Monica Arora indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Fatimah Spall indicated no relevant financial relationships.
Neva Castro indicated no relevant financial relationships.
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Fatimah Spall, DO3, Neva Castro, MD4. P4675 - Colon Under Pressure: A Case of Colonic Varix, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mather Hospital, Northwell Health, Port Jefferson, NY; 2Northwell Health/Mather Hospital, Port Jefferson, NY; 3Mather Hospital, Zucker School of Medicine at Hofstra University, Port Jefferson, NY; 4Northwell Health, Setauket, NY
Introduction: Ectopic varices, large portosystemic venous collaterals located outside the gastroesophageal region (including colonic, rectal, and gonadal varices), pose a unique challenge. These account for 1–5% of variceal bleeds. Colonic varices can present with lower gastrointestinal bleeding and are identified through endoscopic or imaging investigations. Definitive guidelines are lacking for ectopic varices due to the varied locations and presentations.
Case Description/
Methods: A 59-year-old male with alcohol cirrhosis, grade 1 esophageal varices presented with acute hematochezia and melena. Symptoms included a 40-pound weight loss over 3 years, dry heaving, and vague abdominal pain. Vitals stable. Physical exam notable for tender epigastric region to palpation. Laboratory findings hemoglobin of 6.5, platelets 111, total bilirubin 5.5, direct bilirubin 2.9, AST 71, ALT 23, and alkaline phosphatase 171, INR 1.57, Creatinine 0.68. MELD 21. CTAP showed cirrhosis, portal hypertension, esophageal varices, splenorenal shunt with a venous aneurysm, and additional portal venous collaterals (superior mesenteric vein draining to the gonadal vein) noted in the right side of the abdomen some of which are inseparable from the wall of the ascending colon. Upper endoscopy did not reveal source of bleeding. Colonoscopy revealed bright red blood with clots up to the transverse colon, large, grade 3 colonic varices were identified in the ascending colon (Figure B), Non-bleeding rectal varices and hemorrhoids. Hospital course complicated by hematochezia and anemia, requiring 7 units of packed red blood cells (PRBCs). He was started on an octreotide drip and transferred to a liver transplant center for sclerotherapy and embolization of colonic varices prior to Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement.
Discussion: A review of 169 ectopic variceal bleeding cases revealed ectopic varices in the duodenum (17%), jejunum or ileum (17%), colon (14%), rectum (8%), and peritoneum (9%).
Management of ectopic varices with medications like octreotide remains uncertain. Endoscopy management includes band ligation, endoscopic sclerotherapy, or glue injection. Other alternatives include Balloon-occluded retrograde transvenous obliteration (BRTO) and Percutaneous transhepatic obliteration (PTO). The recommended approach for effective bleeding management involves a combination of TIPS and embolization.
In our patient, the management plan involved sclerotherapy and TIPS with a long-term goal of a liver transplant.
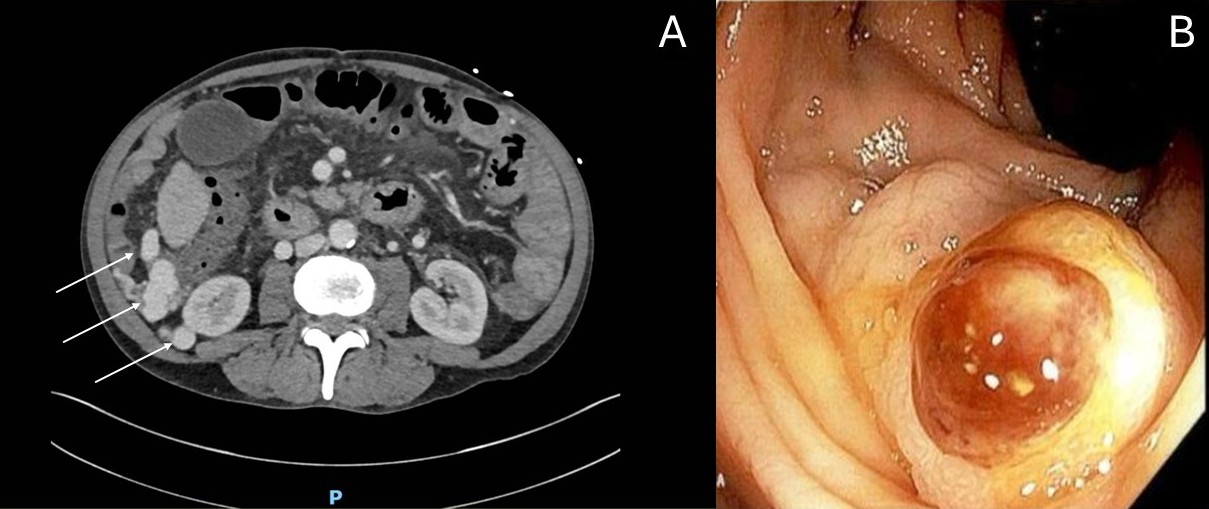
Figure: Figure A: CT Abdomen Pelvis revealed varices involving the ascending colon (white arrows). The vessels are adjacent to the ascending colon. There is no fat plane on imaging, making the varices inseparable from the colon.
Figure B: Large, grade 3 colonic varix identified in the ascending colon.
Disclosures:
Monica Arora indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Fatimah Spall indicated no relevant financial relationships.
Neva Castro indicated no relevant financial relationships.
Monica Arora, DO1, Muhammad Jahanzaib Khan, MD2, Fatimah Spall, DO3, Neva Castro, MD4. P4675 - Colon Under Pressure: A Case of Colonic Varix, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

