Tuesday Poster Session
Category: Colon
P4672 - Recurrent Ischemic Colitis Secondary to Orthostatic Hypotension: Recognizing a Hidden Culprit

Mustafa Sadek, MD
NCH Healthcare System
Naples, FL
Presenting Author(s)
NCH Healthcare System, Naples, FL
Introduction: Ischemic colitis is the most common form of intestinal ischemia, typically due to reduced colonic blood flow. It is more often seen in acute illnesses such as shock. While systemic hypotension is a known risk, cases from chronic orthostatic hypotension are rare. We present a case highlighting this underrecognized cause.
Case Description/
Methods:
A 54 year old woman with a history of multiple admissions for ischemic colitis presented with acute onset of severe cramping lower abdominal pain, associated with vomiting, hematochezia, and diarrhea. She was hemodynamically stable on admission. Laboratory findings were notable for leukocytosis (WBC 18.6 ×10⁹/L). A contrast-enhanced CT scan of the abdomen revealed wall thickening of the descending colon with pericolic stranding, consistent with colitis. Sigmoidoscopy demonstrated congested mucosa in the sigmoid and descending colon, with several ulcers (Figure 1). Biopsies confirmed focal active ischemic colitis.
Due to the severity of her symptoms and concern for bowel perforation, colectomy was considered. However, she responded well to aggressive IV fluid resuscitation and improved significantly, ultimately avoiding surgery. Near discharge, a new concern emerged: her systolic blood pressure (SBP) declined, ranging from 90 to 95 mmHg, with a mean arterial pressure (MAP) reaching 67 mmHg.
Ongoing outpatient monitoring revealed persistent hypotension. At her primary care follow-up, her blood pressure was 97/68 mmHg. Six months later, a follow-up colonoscopy showed segmental erythema in the sigmoid and descending colon (Figure 2).
Notably, her blood pressure on the day of the colonoscopy remained low, with SBP ranging from 85 to 98 mmHg and MAP between 68 and 73 mmHg. Given the recurrent ischemic colitis episodes and persistently low blood pressure, her gastroenterologist suspected orthostatic hypotension as a contributing factor.
She was ultimately diagnosed with orthostatic hypotension and started on midodrine, along with lifestyle modifications including increased salt and fluid intake and the use of compression garments.
Discussion:
This case underscores orthostatic hypotension as a rare but important cause of recurrent ischemic colitis. Chronic low flow states may lead to repeated hypoperfusion of vulnerable colonic watershed areas. Recognizing orthostatic hypotension as the primary etiology enabled targeted treatment and may help prevent recurrence. Clinicians should consider it in patients with recurrent ischemic colitis and no clear acute trigger.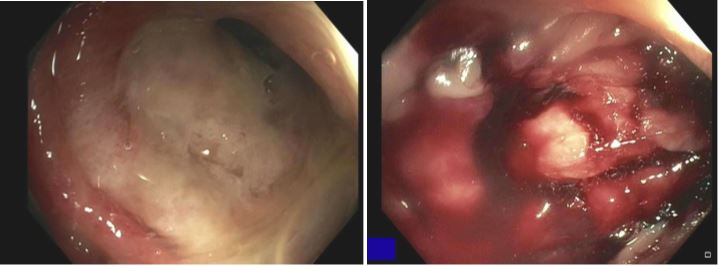
Figure: Figure 1: Endoscopic images showing ischemic colitis in the descending colon (left) and sigmoid colon (right).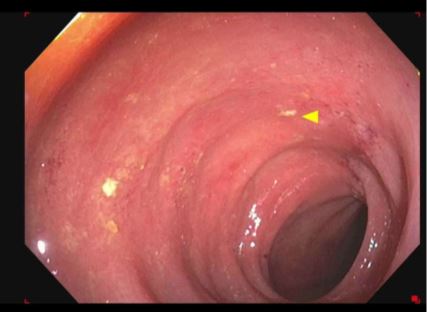
Figure: Figure 2: Endoscopic image showing ischemic colitis in the descending colon six months after discharge, indicated by the yellow arrowhead.
Disclosures:
Mustafa Sadek indicated no relevant financial relationships.
Alaa Almallouhi indicated no relevant financial relationships.
Mustafa Sadek, MD, Alaa Almallouhi, MD. P4672 - Recurrent Ischemic Colitis Secondary to Orthostatic Hypotension: Recognizing a Hidden Culprit, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
