Tuesday Poster Session
Category: Colon
P4662 - Cholecystocolonic Fistula with Coexisting Diverticulosis and Gallstone Disease: A Diagnostic and Therapeutic Challenge
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panisara Fangsaard, MD
Bassett Medical Center
Cooperstown, NY
Presenting Author(s)
Panisara Fangsaard, MD, Unaib Ahmed Memon, MBBS, Timur Otajonov, MD, Farhan Afridi, MBBS, Nikita Srivalsan, MD, Carmine Catalano, MD
Bassett Medical Center, Cooperstown, NY
Introduction: Cholecystocolonic fistula (CCF) is a rare but significant complication of gallbladder disease. While it typically results from chronic cholecystitis or cholelithiasis, several studies suggest that CCF may arise secondary to colonic diverticulosis. Presentations are often incidental or non-acute, characterized by the classic triad of pneumobilia, diarrhea, and vitamin K malabsorption. Here, we report a case of CCF presenting with acute cholecystitis (AC) sepsis in the setting of diverticulosis.
Case Description/
Methods: A 71-year-old male with a history of hypertension, hyperlipidemia, and type II diabetes presented with epigastric pain for 3 days. Vital signs revealed a temperature of 37.8 °C, heart rate 106 bpm, blood pressure 127/70 mmHg, respiratory rate 16/min, and SpO2 95%. Physical examination showed tenderness on the right upper abdomen without peritoneal signs. Laboratory results were significant for leukocytosis of 16,700 cells/μL, total bilirubin of 2.0 mg/dL, direct bilirubin of 0.5 mg/dL, and alkaline phosphatase of 65 U/L. A computed tomography (CT) scan of the abdomen revealed AC, presence of pneumobilia, and CCF (Figure 1). On hospital day two, the patient developed a myocardial infarction and was deemed a poor surgical candidate. He was managed with piperacillin-tazobactam. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed CCF and noted choledocholithiasis (Figure 2). The stones were removed, and a stent was placed in the common bile duct. A percutaneous cholecystostomy was performed. The patient's symptoms improved, and he was discharged after one week. Outpatient colonoscopy revealed severe pan-diverticulosis and resolution of the fistula. He subsequently underwent elective cholecystectomy.
Discussion: This case highlights several learning points. First, CCF may present atypically, including in acute settings such as AC sepsis, necessitating a high level of diagnostic suspicion. Second, identifying the etiology of CCF in the coexistence of diverticulosis and gallstone disease is challenging but crucial for guiding timely management decisions. In this case, conservative treatment with antibiotics and GB decompression led to fistula resolution, as confirmed by follow-up colonoscopy and CT abdomen. Third, although the pathogenesis of CCF related to diverticulosis is thought to involve diverticulitis, no evidence of diverticulitis was observed in this case. This knowledge gap warrants further investigation.

Figure: Figure 1: CT abdomen showed acute cholecystitis, gas in the gallbladder cystic duct, minimal pneumobilia, and cholecystocolonic fistula
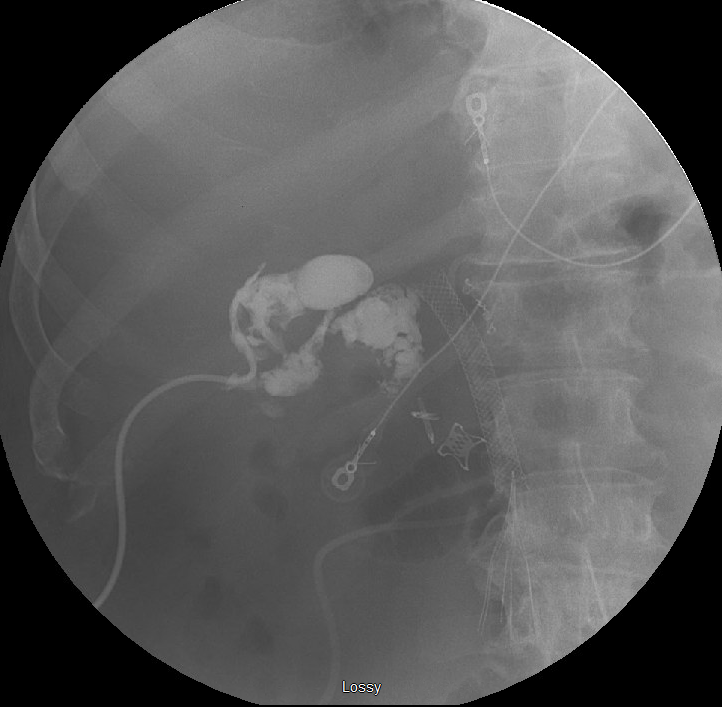
Figure: Figure 2: ERCP revealed the presence of the cholecystocolonic fistula and choledocholithiasis
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Unaib Ahmed Memon indicated no relevant financial relationships.
Timur Otajonov indicated no relevant financial relationships.
Farhan Afridi indicated no relevant financial relationships.
Nikita Srivalsan indicated no relevant financial relationships.
Carmine Catalano indicated no relevant financial relationships.
Panisara Fangsaard, MD, Unaib Ahmed Memon, MBBS, Timur Otajonov, MD, Farhan Afridi, MBBS, Nikita Srivalsan, MD, Carmine Catalano, MD. P4662 - Cholecystocolonic Fistula with Coexisting Diverticulosis and Gallstone Disease: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Bassett Medical Center, Cooperstown, NY
Introduction: Cholecystocolonic fistula (CCF) is a rare but significant complication of gallbladder disease. While it typically results from chronic cholecystitis or cholelithiasis, several studies suggest that CCF may arise secondary to colonic diverticulosis. Presentations are often incidental or non-acute, characterized by the classic triad of pneumobilia, diarrhea, and vitamin K malabsorption. Here, we report a case of CCF presenting with acute cholecystitis (AC) sepsis in the setting of diverticulosis.
Case Description/
Methods: A 71-year-old male with a history of hypertension, hyperlipidemia, and type II diabetes presented with epigastric pain for 3 days. Vital signs revealed a temperature of 37.8 °C, heart rate 106 bpm, blood pressure 127/70 mmHg, respiratory rate 16/min, and SpO2 95%. Physical examination showed tenderness on the right upper abdomen without peritoneal signs. Laboratory results were significant for leukocytosis of 16,700 cells/μL, total bilirubin of 2.0 mg/dL, direct bilirubin of 0.5 mg/dL, and alkaline phosphatase of 65 U/L. A computed tomography (CT) scan of the abdomen revealed AC, presence of pneumobilia, and CCF (Figure 1). On hospital day two, the patient developed a myocardial infarction and was deemed a poor surgical candidate. He was managed with piperacillin-tazobactam. Endoscopic retrograde cholangiopancreatography (ERCP) confirmed CCF and noted choledocholithiasis (Figure 2). The stones were removed, and a stent was placed in the common bile duct. A percutaneous cholecystostomy was performed. The patient's symptoms improved, and he was discharged after one week. Outpatient colonoscopy revealed severe pan-diverticulosis and resolution of the fistula. He subsequently underwent elective cholecystectomy.
Discussion: This case highlights several learning points. First, CCF may present atypically, including in acute settings such as AC sepsis, necessitating a high level of diagnostic suspicion. Second, identifying the etiology of CCF in the coexistence of diverticulosis and gallstone disease is challenging but crucial for guiding timely management decisions. In this case, conservative treatment with antibiotics and GB decompression led to fistula resolution, as confirmed by follow-up colonoscopy and CT abdomen. Third, although the pathogenesis of CCF related to diverticulosis is thought to involve diverticulitis, no evidence of diverticulitis was observed in this case. This knowledge gap warrants further investigation.

Figure: Figure 1: CT abdomen showed acute cholecystitis, gas in the gallbladder cystic duct, minimal pneumobilia, and cholecystocolonic fistula
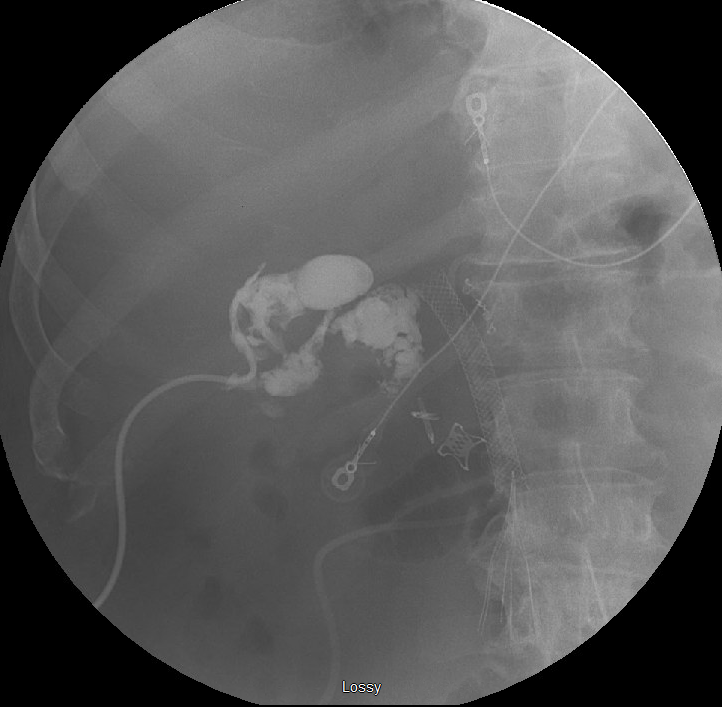
Figure: Figure 2: ERCP revealed the presence of the cholecystocolonic fistula and choledocholithiasis
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Unaib Ahmed Memon indicated no relevant financial relationships.
Timur Otajonov indicated no relevant financial relationships.
Farhan Afridi indicated no relevant financial relationships.
Nikita Srivalsan indicated no relevant financial relationships.
Carmine Catalano indicated no relevant financial relationships.
Panisara Fangsaard, MD, Unaib Ahmed Memon, MBBS, Timur Otajonov, MD, Farhan Afridi, MBBS, Nikita Srivalsan, MD, Carmine Catalano, MD. P4662 - Cholecystocolonic Fistula with Coexisting Diverticulosis and Gallstone Disease: A Diagnostic and Therapeutic Challenge, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

