Tuesday Poster Session
Category: Colon
P4720 - Strange Rectal Bedfellow: Isolated Perirectal Squamous Cell Carcinoma of Unknown Origin
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NG
Nathaniel C. Goss, MD (he/him/his)
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Nathaniel C. Goss, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Cancer of unknown primary (CUP) accounts for up to 5% of all invasive cancers. Only 10% of CUP is squamous cell carcinoma (SCC). Cervical lymph nodes are the most common location for this scenario. Pelvic SCC without an anogenital primary lesion is uncommon. We present an unusual case of isolated perirectal SCC diagnosed with endoscopic ultrasound with fine needle biopsy (EUS/FNB).
Case Description/
Methods: A 52 year-old female with history of breast cancer at age 26 in remission since lumpectomy with chemoradiation, multiple cutaneous basal cell carcinomas and melanomas and total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH-BSO) for abnormal uterine bleeding from fibroids at age 42 presented with four months of progressive, severe left lower quadrant pain. CT of the abdomen and pelvis showed a large perirectal mass which was followed by an MRI demonstrating an ill-defined mass within the mid rectum. Initial colonoscopy showed extrinsic compression in this area with normal mucosa. EUS showed a 34 x 30 mm hypoechoic perirectal mass with adjacent malignant appearing lymph nodes. Pathology from FNB showed at least high grade squamous intraepithelial lesion with features suggestive, but not definitive for invasive squamous cell carcinoma. Further anogenital examinations and PET imaging was unrevealing for a primary source. Review of the pathology from her prior TAH-BSO showed only (CIN) grade II with prior HPV testing and all subsequent Pap tests and comprehensive genetic testing being negative. She began chemo-immunotherapy and radiation with curative intent with a satisfactory clinical and radiologic response thus far.
Discussion: A perirectal SCC without an identified anogenital source is rare. This patient had a history of CIN II found incidentally, but all surveillance exams after TAH-BSO were normal. This makes a cervical primary cancer highly unusual, but it remained a more probable explanation than skin or anal primary given normal examinations. For pelvic SCC without a known primary, a decision must be made using all the available evidence to guide treatment. Multi-disciplinary collaboration is required. In this patient’s case, using immunotherapy with chemoradiation protocols found to be effective for locally advanced cervical cancer was chosen. EUS/FNB should be considered for similar cases as it was instrumental in establishing a diagnosis given conflicting CT and MRI findings, obtaining pathologic diagnosis and obviating the need for more invasive means of doing so.
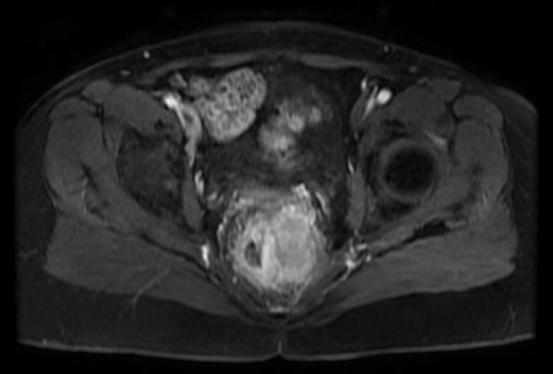
Figure: Magnetic resonance with contrast image demonstrating enhancing multilobulated pelvic mass with mass effect and possible invasion of the left aspect of the rectum.

Figure: Endoscopic ultrasound w/ fine needle biopsy of the perirectal mass
Disclosures:
Nathaniel Goss indicated no relevant financial relationships.
Charleston Powell indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Nathaniel C. Goss, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG. P4720 - Strange Rectal Bedfellow: Isolated Perirectal Squamous Cell Carcinoma of Unknown Origin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Cancer of unknown primary (CUP) accounts for up to 5% of all invasive cancers. Only 10% of CUP is squamous cell carcinoma (SCC). Cervical lymph nodes are the most common location for this scenario. Pelvic SCC without an anogenital primary lesion is uncommon. We present an unusual case of isolated perirectal SCC diagnosed with endoscopic ultrasound with fine needle biopsy (EUS/FNB).
Case Description/
Methods: A 52 year-old female with history of breast cancer at age 26 in remission since lumpectomy with chemoradiation, multiple cutaneous basal cell carcinomas and melanomas and total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH-BSO) for abnormal uterine bleeding from fibroids at age 42 presented with four months of progressive, severe left lower quadrant pain. CT of the abdomen and pelvis showed a large perirectal mass which was followed by an MRI demonstrating an ill-defined mass within the mid rectum. Initial colonoscopy showed extrinsic compression in this area with normal mucosa. EUS showed a 34 x 30 mm hypoechoic perirectal mass with adjacent malignant appearing lymph nodes. Pathology from FNB showed at least high grade squamous intraepithelial lesion with features suggestive, but not definitive for invasive squamous cell carcinoma. Further anogenital examinations and PET imaging was unrevealing for a primary source. Review of the pathology from her prior TAH-BSO showed only (CIN) grade II with prior HPV testing and all subsequent Pap tests and comprehensive genetic testing being negative. She began chemo-immunotherapy and radiation with curative intent with a satisfactory clinical and radiologic response thus far.
Discussion: A perirectal SCC without an identified anogenital source is rare. This patient had a history of CIN II found incidentally, but all surveillance exams after TAH-BSO were normal. This makes a cervical primary cancer highly unusual, but it remained a more probable explanation than skin or anal primary given normal examinations. For pelvic SCC without a known primary, a decision must be made using all the available evidence to guide treatment. Multi-disciplinary collaboration is required. In this patient’s case, using immunotherapy with chemoradiation protocols found to be effective for locally advanced cervical cancer was chosen. EUS/FNB should be considered for similar cases as it was instrumental in establishing a diagnosis given conflicting CT and MRI findings, obtaining pathologic diagnosis and obviating the need for more invasive means of doing so.
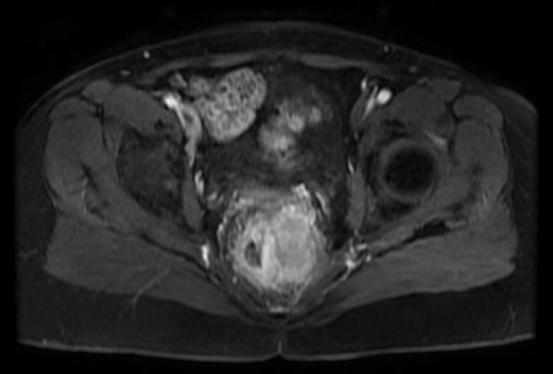
Figure: Magnetic resonance with contrast image demonstrating enhancing multilobulated pelvic mass with mass effect and possible invasion of the left aspect of the rectum.

Figure: Endoscopic ultrasound w/ fine needle biopsy of the perirectal mass
Disclosures:
Nathaniel Goss indicated no relevant financial relationships.
Charleston Powell indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Nathaniel C. Goss, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG. P4720 - Strange Rectal Bedfellow: Isolated Perirectal Squamous Cell Carcinoma of Unknown Origin, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
