Tuesday Poster Session
Category: Colon
P4717 - A Rare Endoscopic Presentation of Acute Colonic Pseudo-Obstruction Related to Chronic Anastomotic Dehiscence
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Olivia Becker, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Olivia Becker, MD, Manavi Bhagwat, MD, Andrew Copland, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: Ogilvie’s syndrome, or acute colonic pseudo-obstruction (ACPO), is a common cause of colonic dilation and ischemia among critically ill and post-surgical hospitalized patients, but a mechanical cause of colonic obstruction should also be considered. We present a case where likely ACPO was further complicated by anastomotic dehiscence (AD) in the rectosigmoid junction.
Case Description/
Methods: A 76-year-old woman with a history of end-stage renal disease, rectosigmoid adenocarcinoma (in remission), and prior partial colectomy with end-to-end colo-colonic anastomosis in the sigmoid colon presented 6 days after a kidney transplant surgery with nausea, abdominal pain, and distention. Computed tomography revealed diffuse colonic dilation, heterogeneous appearing cecum, and proximal ascending colon with possible pneumatosis. Colonoscopy was attempted for decompression and revealed a large area of ulceration and contact friability extending 5 cm from the anal verge to the dentate line. The depth of apparent ulceration and resistance to traversing the possible lumen prevented further advancement into the colon [Figure 1]. On further chart review, a solitary rectal ulcer had been visualized and biopsied on colonoscopy 4 years prior but was thought to be ischemic in nature. Colorectal surgery assisted in repeat colonoscopy to traverse the area of stenosis abutting what was suspected to be chronic rectal dehiscence [Figure 2]. After successfully traversing the area of dehiscence, the right colon demonstrated mucosal ulceration related to substantial distension. Colonic decompression was performed. Due to symptom improvement and hemodynamic stability, repair of the dehiscence was initially deferred. Her course was complicated by Bacterioides fragilis bacteremia and rectovaginal fistula, for which she eventually underwent diverting transverse loop colostomy.
Discussion: The diagnosis of ACPO should be considered contextually and mechanical obstruction must be ruled out. In this case, chronic AD likely contributed to the clinical presentation and made subsequent management more challenging. Complications of chronic AD include systemic infection, fistulization, and a presacral sinus. AD is rarely encountered on endoscopic evaluation by gastroenterologists but is often easily recognized by an experienced colorectal surgeon. Good partnerships between gastroenterologists and colorectal surgeons can benefit patient outcomes.
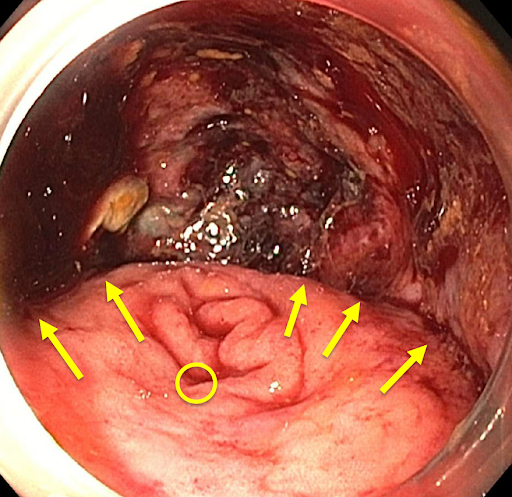
Figure: Rectal anastomosis dehiscence. Area above arrows is the presacral space while the circle highlights the colon lumen.
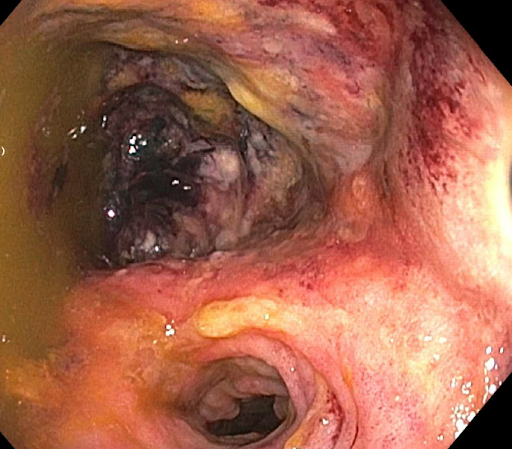
Figure: Eventual traversal of rectal AD with colorectal surgery assistance (lumen in lower half of image, dehiscence in upper half of image).
Disclosures:
Olivia Becker indicated no relevant financial relationships.
Manavi Bhagwat indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Olivia Becker, MD, Manavi Bhagwat, MD, Andrew Copland, MD. P4717 - A Rare Endoscopic Presentation of Acute Colonic Pseudo-Obstruction Related to Chronic Anastomotic Dehiscence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: Ogilvie’s syndrome, or acute colonic pseudo-obstruction (ACPO), is a common cause of colonic dilation and ischemia among critically ill and post-surgical hospitalized patients, but a mechanical cause of colonic obstruction should also be considered. We present a case where likely ACPO was further complicated by anastomotic dehiscence (AD) in the rectosigmoid junction.
Case Description/
Methods: A 76-year-old woman with a history of end-stage renal disease, rectosigmoid adenocarcinoma (in remission), and prior partial colectomy with end-to-end colo-colonic anastomosis in the sigmoid colon presented 6 days after a kidney transplant surgery with nausea, abdominal pain, and distention. Computed tomography revealed diffuse colonic dilation, heterogeneous appearing cecum, and proximal ascending colon with possible pneumatosis. Colonoscopy was attempted for decompression and revealed a large area of ulceration and contact friability extending 5 cm from the anal verge to the dentate line. The depth of apparent ulceration and resistance to traversing the possible lumen prevented further advancement into the colon [Figure 1]. On further chart review, a solitary rectal ulcer had been visualized and biopsied on colonoscopy 4 years prior but was thought to be ischemic in nature. Colorectal surgery assisted in repeat colonoscopy to traverse the area of stenosis abutting what was suspected to be chronic rectal dehiscence [Figure 2]. After successfully traversing the area of dehiscence, the right colon demonstrated mucosal ulceration related to substantial distension. Colonic decompression was performed. Due to symptom improvement and hemodynamic stability, repair of the dehiscence was initially deferred. Her course was complicated by Bacterioides fragilis bacteremia and rectovaginal fistula, for which she eventually underwent diverting transverse loop colostomy.
Discussion: The diagnosis of ACPO should be considered contextually and mechanical obstruction must be ruled out. In this case, chronic AD likely contributed to the clinical presentation and made subsequent management more challenging. Complications of chronic AD include systemic infection, fistulization, and a presacral sinus. AD is rarely encountered on endoscopic evaluation by gastroenterologists but is often easily recognized by an experienced colorectal surgeon. Good partnerships between gastroenterologists and colorectal surgeons can benefit patient outcomes.
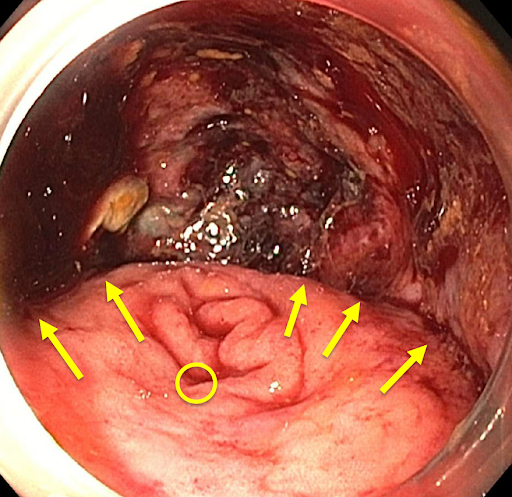
Figure: Rectal anastomosis dehiscence. Area above arrows is the presacral space while the circle highlights the colon lumen.
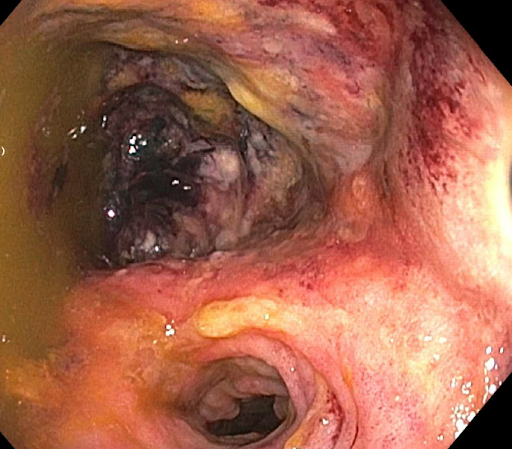
Figure: Eventual traversal of rectal AD with colorectal surgery assistance (lumen in lower half of image, dehiscence in upper half of image).
Disclosures:
Olivia Becker indicated no relevant financial relationships.
Manavi Bhagwat indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Olivia Becker, MD, Manavi Bhagwat, MD, Andrew Copland, MD. P4717 - A Rare Endoscopic Presentation of Acute Colonic Pseudo-Obstruction Related to Chronic Anastomotic Dehiscence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
