Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4794 - Patients With Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus and Anal Dysplasia Utilizing a Markov Model
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Lukus Berber, MD (he/him/his)
Advocate Lutheran General
Des Plaines, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Lukus Berber, MD1, Olivia Foy, MD2, Eli Ehrenpreis, MD, FACG2, Jesus Cantu, MS3
1Advocate Lutheran General, Des Plaines, IL; 2Advocate Lutheran General, Park Ridge, IL; 3Loyola University, Chicago, IL
Introduction: Human papillomavirus (HPV) infection is typically self-limiting, but persistent infection with high-risk HPV subtypes can lead to malignancy. Women with cervical HPV infection are seven times more likely to have concurrent anal HPV infection. Studies in men who have sex with men (MSM) demonstrate that targeted HPV screening can reduce anal cancer incidence. Our model evaluates the potential benefits and cost-effectiveness of screening for anal HPV and dysplasia among women newly diagnosed with cervical cancer.
Methods: We developed a Markov cohort model to simulate disease progression and outcomes over a 20-year period in women newly diagnosed with cervical cancer. Inputs included: initial anal cytology, HPV infection rates, and rates of histological progression and regression (normal to low-grade dysplasia, high-grade dysplasia [HSIL], and anal cancer). Previously published data in MSM populations and cervical cancer survivors were used to input transition rates. The model compared screening, anal HPV testing and treatment of anal HSIL, versus no screening. Costs were derived from 2025 inflation-adjusted rates from the Centers for Medicare & Medicaid Services and published literature. Outcomes included anal cancer incidence, anal cancer mortality, quality-adjusted life years (QALYs), total and incremental costs, and cost per QALY gained.
Results: At 10 years, the screening resulted in 364 cumulative anal cancer cases compared to 620 in the unscreened group. Anal cancer deaths were reduced from 151 to 87 with screening. Total all-cause deaths were 269 with screening vs. 346 without. QALYs gained were higher with screening (89,309 vs. 85,248), and cumulative costs were lower ($454.4M screened vs. $647.9M unscreened). By 20 years, screening prevented 1,227 cases of anal cancer, 279 cancer-related deaths, gained an additional 4,061 discounted QALYs, and saved over $193.6 million.
Discussion: The incidence of anal cancer is rising among white and Hispanic women over the age of 65—a demographic also experiencing increased cervical cancer rates and higher mortality. Our model predicts that implementing anal HPV screening with early treatment of HSIL in women diagnosed with cervical cancer reduces the incidence and mortality of anal cancer. Furthermore, it is cost-effective and supports recent International Anal Neoplasia Society guidance recommending screening in this high-risk population.
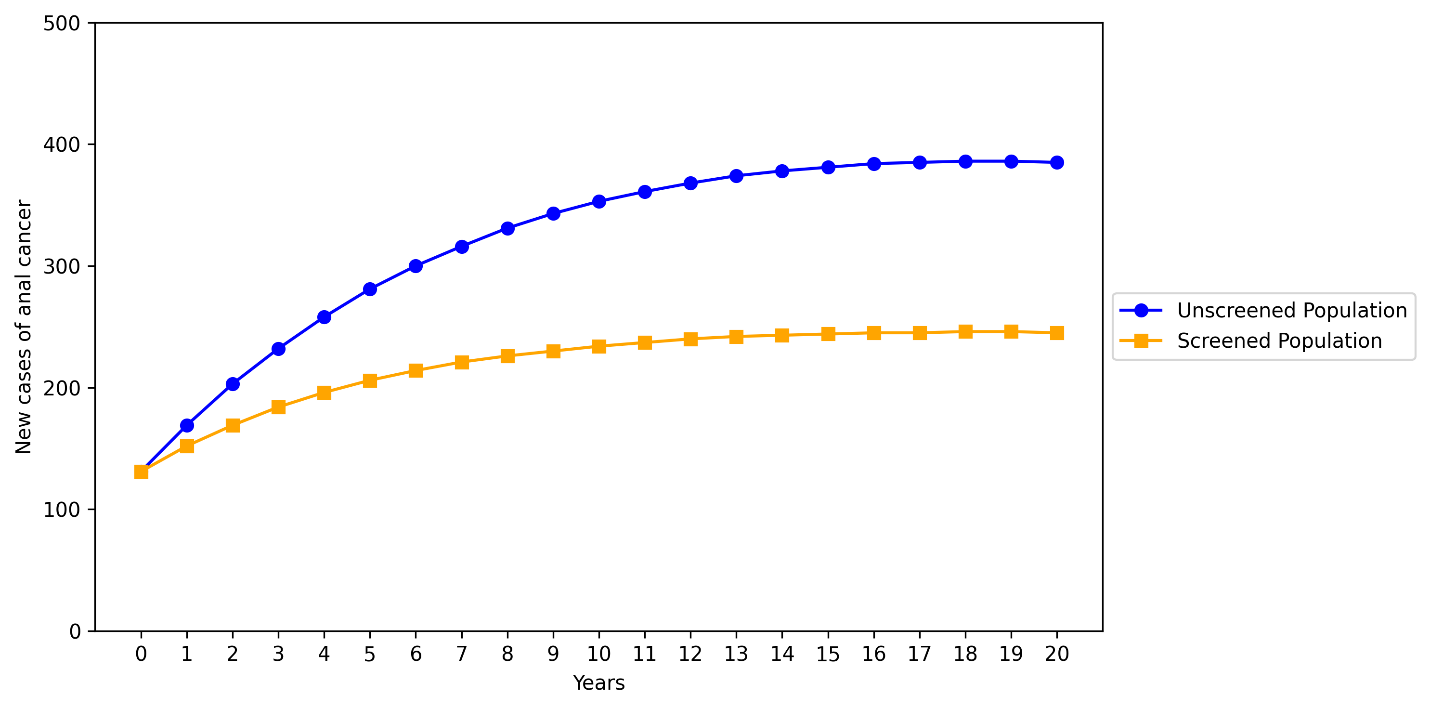
Figure: Predicted number of new anal cancer cases per year over a 20-year period in women with a history of cervical cancer, comparing those undergoing screening for anal dysplasia with those not screened
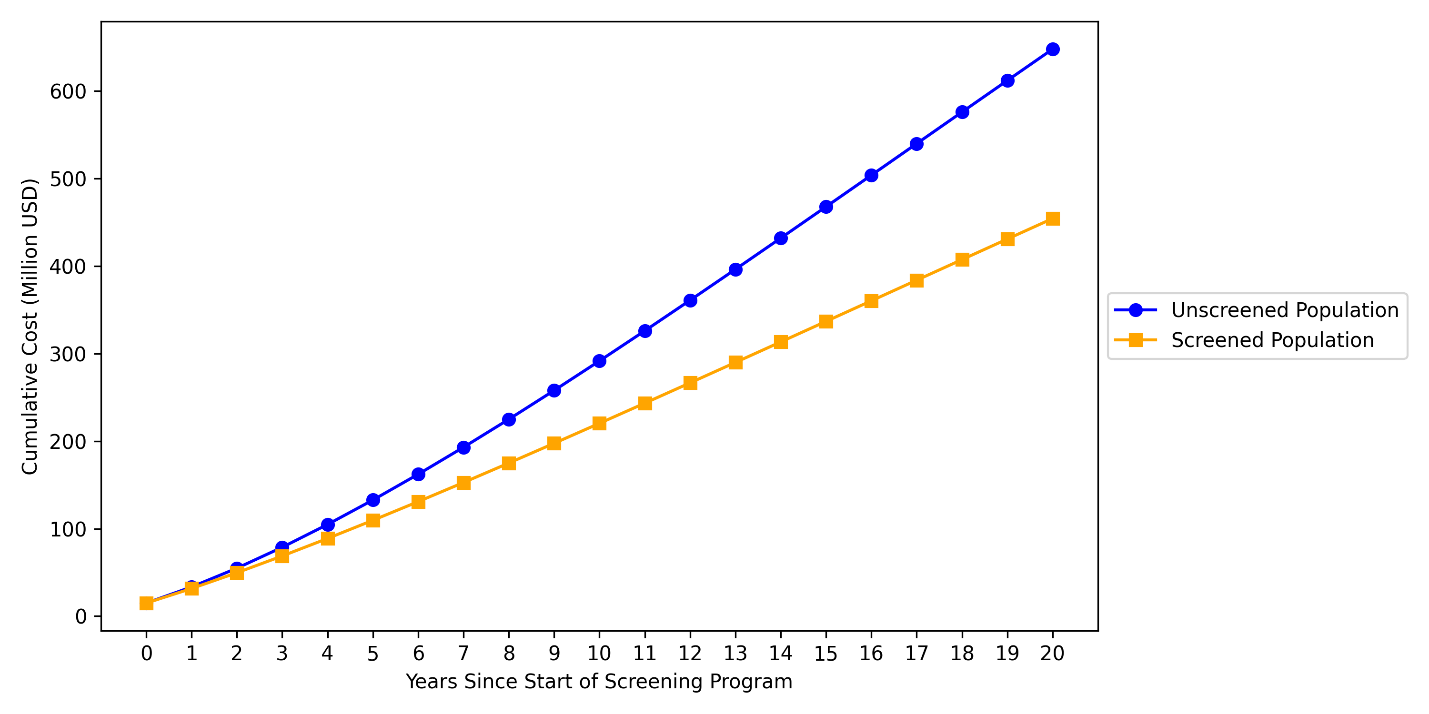
Figure: Predicted cumulative costs of screening and treatment for anal cancer over a 20-year period in patients with cervical cancer, comparing screened and unscreened populations
Disclosures:
Lukus Berber indicated no relevant financial relationships.
Olivia Foy indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Jesus Cantu indicated no relevant financial relationships.
Lukus Berber, MD1, Olivia Foy, MD2, Eli Ehrenpreis, MD, FACG2, Jesus Cantu, MS3. P4794 - Patients With Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus and Anal Dysplasia Utilizing a Markov Model, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lukus Berber, MD1, Olivia Foy, MD2, Eli Ehrenpreis, MD, FACG2, Jesus Cantu, MS3
1Advocate Lutheran General, Des Plaines, IL; 2Advocate Lutheran General, Park Ridge, IL; 3Loyola University, Chicago, IL
Introduction: Human papillomavirus (HPV) infection is typically self-limiting, but persistent infection with high-risk HPV subtypes can lead to malignancy. Women with cervical HPV infection are seven times more likely to have concurrent anal HPV infection. Studies in men who have sex with men (MSM) demonstrate that targeted HPV screening can reduce anal cancer incidence. Our model evaluates the potential benefits and cost-effectiveness of screening for anal HPV and dysplasia among women newly diagnosed with cervical cancer.
Methods: We developed a Markov cohort model to simulate disease progression and outcomes over a 20-year period in women newly diagnosed with cervical cancer. Inputs included: initial anal cytology, HPV infection rates, and rates of histological progression and regression (normal to low-grade dysplasia, high-grade dysplasia [HSIL], and anal cancer). Previously published data in MSM populations and cervical cancer survivors were used to input transition rates. The model compared screening, anal HPV testing and treatment of anal HSIL, versus no screening. Costs were derived from 2025 inflation-adjusted rates from the Centers for Medicare & Medicaid Services and published literature. Outcomes included anal cancer incidence, anal cancer mortality, quality-adjusted life years (QALYs), total and incremental costs, and cost per QALY gained.
Results: At 10 years, the screening resulted in 364 cumulative anal cancer cases compared to 620 in the unscreened group. Anal cancer deaths were reduced from 151 to 87 with screening. Total all-cause deaths were 269 with screening vs. 346 without. QALYs gained were higher with screening (89,309 vs. 85,248), and cumulative costs were lower ($454.4M screened vs. $647.9M unscreened). By 20 years, screening prevented 1,227 cases of anal cancer, 279 cancer-related deaths, gained an additional 4,061 discounted QALYs, and saved over $193.6 million.
Discussion: The incidence of anal cancer is rising among white and Hispanic women over the age of 65—a demographic also experiencing increased cervical cancer rates and higher mortality. Our model predicts that implementing anal HPV screening with early treatment of HSIL in women diagnosed with cervical cancer reduces the incidence and mortality of anal cancer. Furthermore, it is cost-effective and supports recent International Anal Neoplasia Society guidance recommending screening in this high-risk population.
Figure: Predicted number of new anal cancer cases per year over a 20-year period in women with a history of cervical cancer, comparing those undergoing screening for anal dysplasia with those not screened
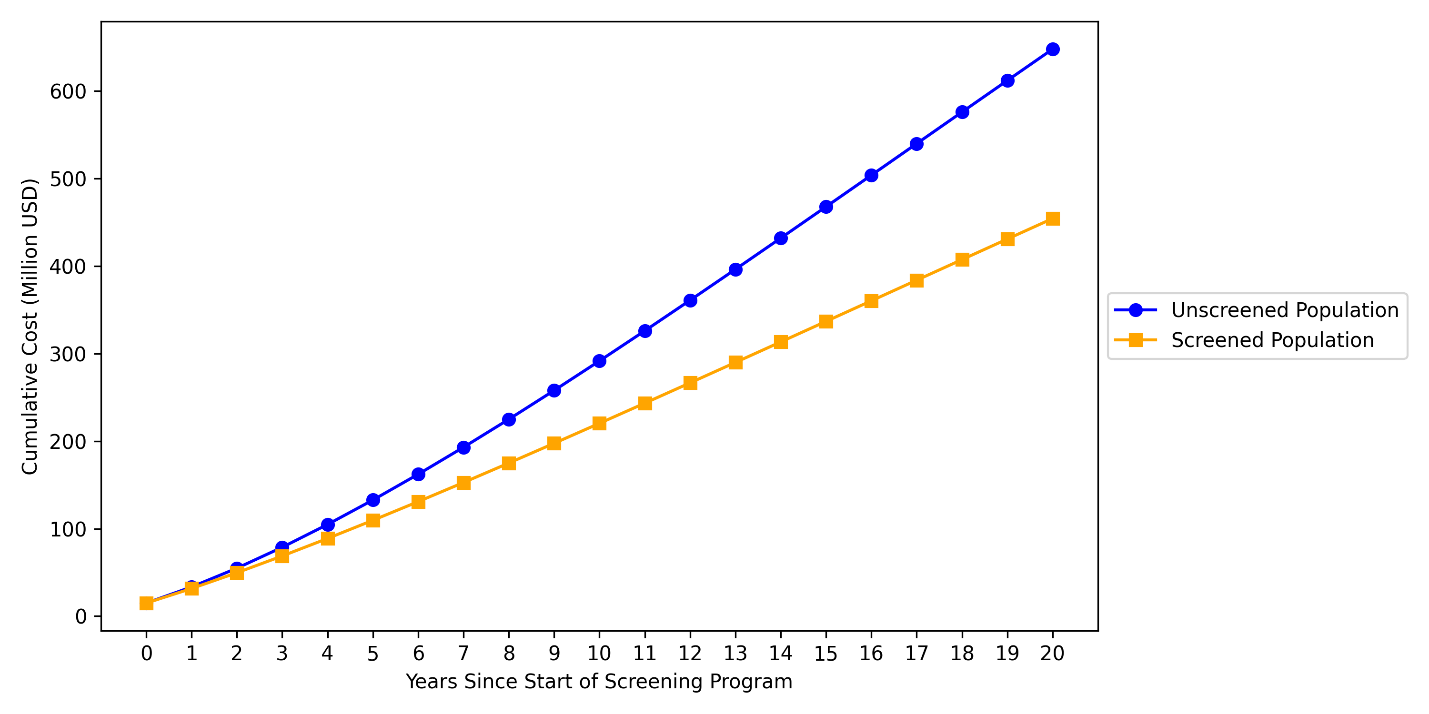
Figure: Predicted cumulative costs of screening and treatment for anal cancer over a 20-year period in patients with cervical cancer, comparing screened and unscreened populations
Disclosures:
Lukus Berber indicated no relevant financial relationships.
Olivia Foy indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Jesus Cantu indicated no relevant financial relationships.
Lukus Berber, MD1, Olivia Foy, MD2, Eli Ehrenpreis, MD, FACG2, Jesus Cantu, MS3. P4794 - Patients With Newly Diagnosed Cervical Cancer Should Be Screened for Anal Human Papillomavirus and Anal Dysplasia Utilizing a Markov Model, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


