Tuesday Poster Session
Category: Esophagus
P4887 - Case-Based Teaching to Improve Resident Knowledge on Screening for Barrett’s Esophagus: A Targeted Curriculum for High-Impact Learning
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Swati Patel, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Swati Patel, MD1, Ines Varela Knorr, MD1, Michael S.. Smith, MD, MBA2, Priya Simoes, MBBS2
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Internal medicine (IM) residents at programs with teaching at multiple sites inherently experience variability in depth and breadth of exposure to subspecialties. The American Board of Internal Medicine (ABIM) Certification Exam first-time pass rate has declined nationally dropping to 87% in 2023. To address these trends, we developed a targeted educational curriculum to unify and reinforce residents’ knowledge of commonly tested gastroenterology (GI) topics.
Methods: A 10‑question needs assessment targeting “High Importance” topics from the ABIM blueprint was completed by 53 PGY‑1 through PGY‑3 residents training across two hospitals and five outpatient clinics. Of these, 41 (77%) reported being unfamiliar or only somewhat familiar with the diagnosis and management of premalignant and malignant GI disorders. Based on these findings, we designed case‑based lectures on Barrett’s esophagus (BE), delivered during half‑day academic sessions split into interns (PGY‑1) and senior residents (PGY‑2/3). Knowledge was measured with pre‑ and post‑session assessments, and retention was evaluated 20 weeks later.
Results: On pre‑assessment, 7 of 19 senior residents (37%) and 12 of 20 interns (60%) correctly answered a ABIM‑style question on BE. Post‑lecture, correct responses rose to 100% (15/15) among seniors and 89% (17/19) among interns. At the 20‑week follow‑up, 8 of 12 residents (67%) answered correctly. Additionally, 79% (26/33) participants reported feeling “comfortable” or “very comfortable” with diagnosing and managing neoplastic esophageal disorders; none reported discomfort.
Discussion: This study addressed trainee knowledge gaps by creating a targeted curriculum based on resident familiarity tailored to "high importance" test topics. These findings demonstrate that a resident‑driven, case‑based GI curriculum significantly improves both short‑ and medium‑term knowledge and confidence. While the voluntary nature of sessions and variable follow‑up rates pose limitations, the study’s strengths lie in individualized learner tracking and targeted content delivery. Case‑based teaching fosters engagement and durable learning through real‑world scenarios. Future interventions will explore the utility of introducing infographics at 10 weeks to further enhance retention and incorporate findings of pending 20-week intern retention data. These findings underscore the value of needs‑based curricular design in addressing subspecialty training gaps.
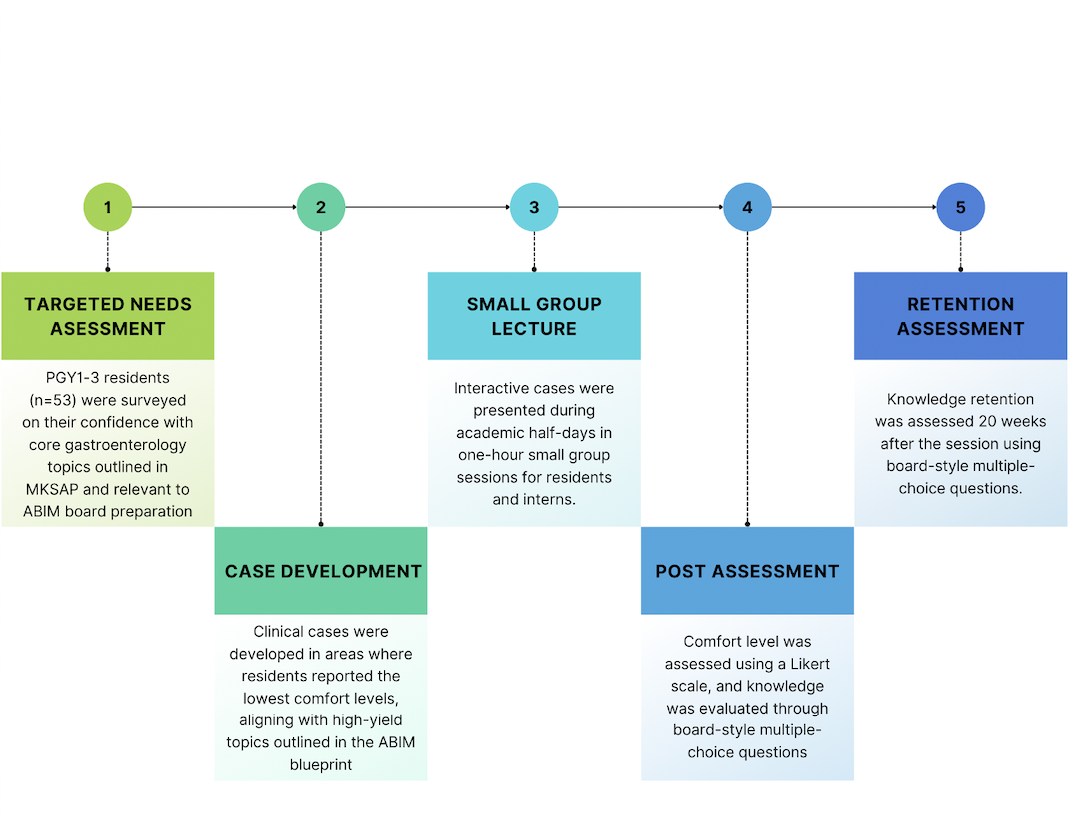
Figure: Figure 1: Curriculum development and evaluation process included: (1) a targeted needs assessment of PGY1–3 residents to identify low-familiarity areas; (2) development of clinical cases aligned with high-yield ABIM blueprint topics; (3) delivery of interactive cases in small-group sessions during academic half-days; (4) post-session assessment of comfort and knowledge using a Likert scale and board-style questions; and (5) knowledge retention evaluation at 20 weeks post-intervention.
Disclosures:
Swati Patel indicated no relevant financial relationships.
Ines Varela Knorr indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Software – Consultant. Sanofi – Consultant. Steris Endoscopy – Consultant.
Priya Simoes indicated no relevant financial relationships.
Swati Patel, MD1, Ines Varela Knorr, MD1, Michael S.. Smith, MD, MBA2, Priya Simoes, MBBS2. P4887 - Case-Based Teaching to Improve Resident Knowledge on Screening for Barrett’s Esophagus: A Targeted Curriculum for High-Impact Learning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Internal medicine (IM) residents at programs with teaching at multiple sites inherently experience variability in depth and breadth of exposure to subspecialties. The American Board of Internal Medicine (ABIM) Certification Exam first-time pass rate has declined nationally dropping to 87% in 2023. To address these trends, we developed a targeted educational curriculum to unify and reinforce residents’ knowledge of commonly tested gastroenterology (GI) topics.
Methods: A 10‑question needs assessment targeting “High Importance” topics from the ABIM blueprint was completed by 53 PGY‑1 through PGY‑3 residents training across two hospitals and five outpatient clinics. Of these, 41 (77%) reported being unfamiliar or only somewhat familiar with the diagnosis and management of premalignant and malignant GI disorders. Based on these findings, we designed case‑based lectures on Barrett’s esophagus (BE), delivered during half‑day academic sessions split into interns (PGY‑1) and senior residents (PGY‑2/3). Knowledge was measured with pre‑ and post‑session assessments, and retention was evaluated 20 weeks later.
Results: On pre‑assessment, 7 of 19 senior residents (37%) and 12 of 20 interns (60%) correctly answered a ABIM‑style question on BE. Post‑lecture, correct responses rose to 100% (15/15) among seniors and 89% (17/19) among interns. At the 20‑week follow‑up, 8 of 12 residents (67%) answered correctly. Additionally, 79% (26/33) participants reported feeling “comfortable” or “very comfortable” with diagnosing and managing neoplastic esophageal disorders; none reported discomfort.
Discussion: This study addressed trainee knowledge gaps by creating a targeted curriculum based on resident familiarity tailored to "high importance" test topics. These findings demonstrate that a resident‑driven, case‑based GI curriculum significantly improves both short‑ and medium‑term knowledge and confidence. While the voluntary nature of sessions and variable follow‑up rates pose limitations, the study’s strengths lie in individualized learner tracking and targeted content delivery. Case‑based teaching fosters engagement and durable learning through real‑world scenarios. Future interventions will explore the utility of introducing infographics at 10 weeks to further enhance retention and incorporate findings of pending 20-week intern retention data. These findings underscore the value of needs‑based curricular design in addressing subspecialty training gaps.
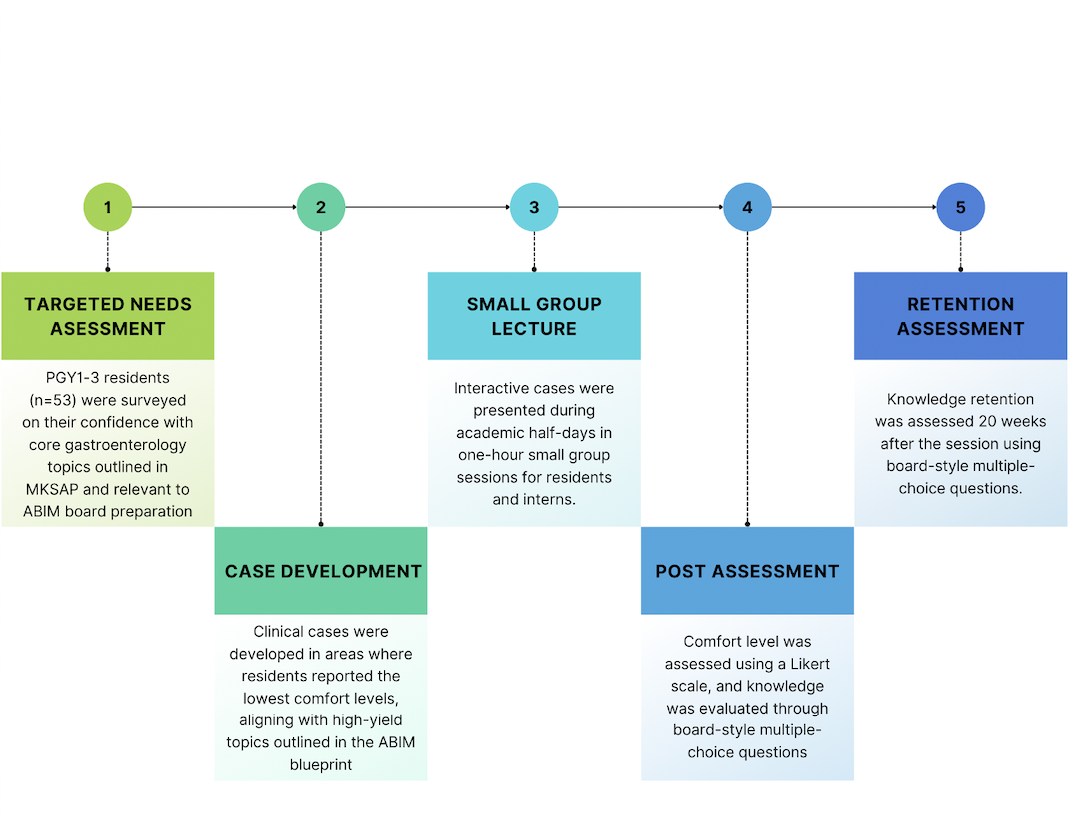
Figure: Figure 1: Curriculum development and evaluation process included: (1) a targeted needs assessment of PGY1–3 residents to identify low-familiarity areas; (2) development of clinical cases aligned with high-yield ABIM blueprint topics; (3) delivery of interactive cases in small-group sessions during academic half-days; (4) post-session assessment of comfort and knowledge using a Likert scale and board-style questions; and (5) knowledge retention evaluation at 20 weeks post-intervention.
Disclosures:
Swati Patel indicated no relevant financial relationships.
Ines Varela Knorr indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Consultant. Provation Software – Consultant. Sanofi – Consultant. Steris Endoscopy – Consultant.
Priya Simoes indicated no relevant financial relationships.
Swati Patel, MD1, Ines Varela Knorr, MD1, Michael S.. Smith, MD, MBA2, Priya Simoes, MBBS2. P4887 - Case-Based Teaching to Improve Resident Knowledge on Screening for Barrett’s Esophagus: A Targeted Curriculum for High-Impact Learning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

