Tuesday Poster Session
Category: Esophagus
P4884 - Risk Factors and Predictors for Esophageal Cancer Among Patients With Achalasia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Julton Tomanguillo Chumbe, MD
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Julton Tomanguillo, MD1, Harleen Chela, MD1, Jennifer Collins, PhD1, Nisar Amin, MD1, Rena Yadlapati, MD2, Ebubekir Daglilar, MD1
1Charleston Area Medical Center, Charleston, WV; 2University of California San Diego, San Diego, CA
Introduction: Despite the correlation between achalasia and an increased risk of esophageal cancer, standardized guidelines for routine endoscopic surveillance are lacking. This study aims to identify risk factors in achalasia patients that may predispose them to developing esophageal cancer, potentially leading to targeted endoscopic surveillance.
Methods: This retrospective cohort study utilized the TriNetX Analytics Platform to analyze achalasia patients aged ≥18 years between 2000 and 2024. Patients with ICD-10 codes for achalasia (K22.0) and esophageal cancer (C15.0) were used to identify the study cohort. Odds ratios were calculated with standard methods, while Cox proportional hazards models estimated hazard ratios and 95% CIs, adjusting for potential confounders. Time to event was measured from achalasia diagnosis to esophageal cancer diagnosis or last follow-up. Backward stepwise selection optimized the model. Patients without EC required ≥1 yr of follow-up. HR and OR results were then compared.
Results: Out of 62,609 patients with achalasia, 1,133 (1.81%) were diagnosed with EC, compared to a 0.072% prevalence in the non-achalasia population. Of the achalasia patients with EC, 506 had an achalasia diagnosis that preceded their EC diagnosis and were included in the final analysis (Table 1). Excluding 130 EC cases diagnosed within one month of achalasia, the median time to EC diagnosis was 296 days. Logistic regression showed strong associations with male sex (OR 2.5, 95% CI 2.1–3.0), white race (OR 1.5, 95% CI 1.2–1.8), GERD (OR 2.5, 95% CI 2.1–3.0), BE (OR 8.0, 95% CI 6.2–10), , esophageal ulcer (OR 9.5, 95% CI 7.2–13), smoking (OR 3.2, 95% CI 2.7–3.9), and alcohol use (OR 3.6, 95% CI 2.6–4.9) (all p < 0.0001). In the CPH model, older age (HR = 1.02, 95% CI: 1.01–1.03), , and elevated creatinine (HR = 1.3, 95% CI: 1.1–1.6) were associated with an increased risk of EC. Interestingly, white race showed higher odds of EC (OR 1.5), but reduced hazard over time (HR 0.57, p < 0.0001). Obstruction also showed high odds (OR 5.6) but lower time-based risk (HR 1.3).
Discussion: Male sex, white race, and history of GERD, Barrett's esophagus, esophageal obstruction or ulcer, smoking, and alcohol use are associated with increased EC risk. Given a median EC diagnosis time of 296 days, annual screening EGD appears reasonable.
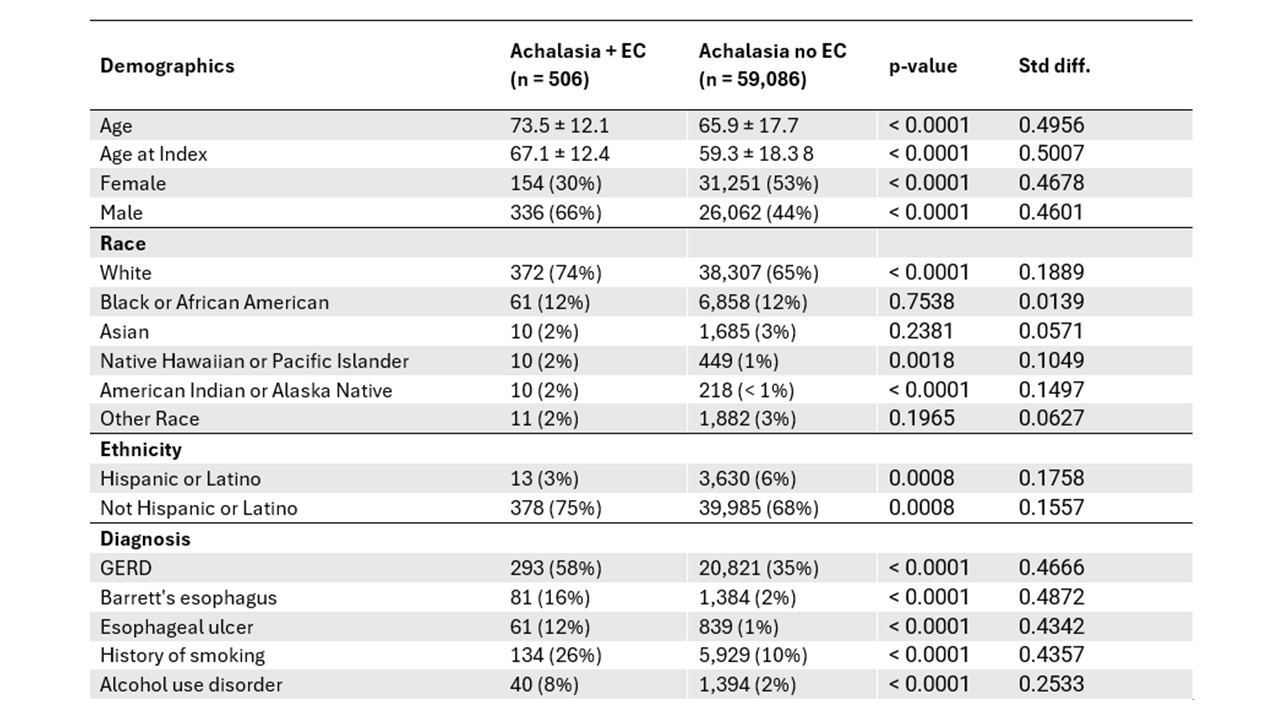
Figure: Table 1: Demographic and Clinical Characteristics
Disclosures:
Julton Tomanguillo indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Jennifer Collins indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Rena Yadlapati: Braintree – Consultant. Medtronic – Consultant. Phathom Pharmaceuticals – Consultant. Reckitt Benckiser – Consultant. RJSMediagnostix – Advisory Committee/Board Member.
Ebubekir Daglilar indicated no relevant financial relationships.
Julton Tomanguillo, MD1, Harleen Chela, MD1, Jennifer Collins, PhD1, Nisar Amin, MD1, Rena Yadlapati, MD2, Ebubekir Daglilar, MD1. P4884 - Risk Factors and Predictors for Esophageal Cancer Among Patients With Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Charleston Area Medical Center, Charleston, WV; 2University of California San Diego, San Diego, CA
Introduction: Despite the correlation between achalasia and an increased risk of esophageal cancer, standardized guidelines for routine endoscopic surveillance are lacking. This study aims to identify risk factors in achalasia patients that may predispose them to developing esophageal cancer, potentially leading to targeted endoscopic surveillance.
Methods: This retrospective cohort study utilized the TriNetX Analytics Platform to analyze achalasia patients aged ≥18 years between 2000 and 2024. Patients with ICD-10 codes for achalasia (K22.0) and esophageal cancer (C15.0) were used to identify the study cohort. Odds ratios were calculated with standard methods, while Cox proportional hazards models estimated hazard ratios and 95% CIs, adjusting for potential confounders. Time to event was measured from achalasia diagnosis to esophageal cancer diagnosis or last follow-up. Backward stepwise selection optimized the model. Patients without EC required ≥1 yr of follow-up. HR and OR results were then compared.
Results: Out of 62,609 patients with achalasia, 1,133 (1.81%) were diagnosed with EC, compared to a 0.072% prevalence in the non-achalasia population. Of the achalasia patients with EC, 506 had an achalasia diagnosis that preceded their EC diagnosis and were included in the final analysis (Table 1). Excluding 130 EC cases diagnosed within one month of achalasia, the median time to EC diagnosis was 296 days. Logistic regression showed strong associations with male sex (OR 2.5, 95% CI 2.1–3.0), white race (OR 1.5, 95% CI 1.2–1.8), GERD (OR 2.5, 95% CI 2.1–3.0), BE (OR 8.0, 95% CI 6.2–10), , esophageal ulcer (OR 9.5, 95% CI 7.2–13), smoking (OR 3.2, 95% CI 2.7–3.9), and alcohol use (OR 3.6, 95% CI 2.6–4.9) (all p < 0.0001). In the CPH model, older age (HR = 1.02, 95% CI: 1.01–1.03), , and elevated creatinine (HR = 1.3, 95% CI: 1.1–1.6) were associated with an increased risk of EC. Interestingly, white race showed higher odds of EC (OR 1.5), but reduced hazard over time (HR 0.57, p < 0.0001). Obstruction also showed high odds (OR 5.6) but lower time-based risk (HR 1.3).
Discussion: Male sex, white race, and history of GERD, Barrett's esophagus, esophageal obstruction or ulcer, smoking, and alcohol use are associated with increased EC risk. Given a median EC diagnosis time of 296 days, annual screening EGD appears reasonable.
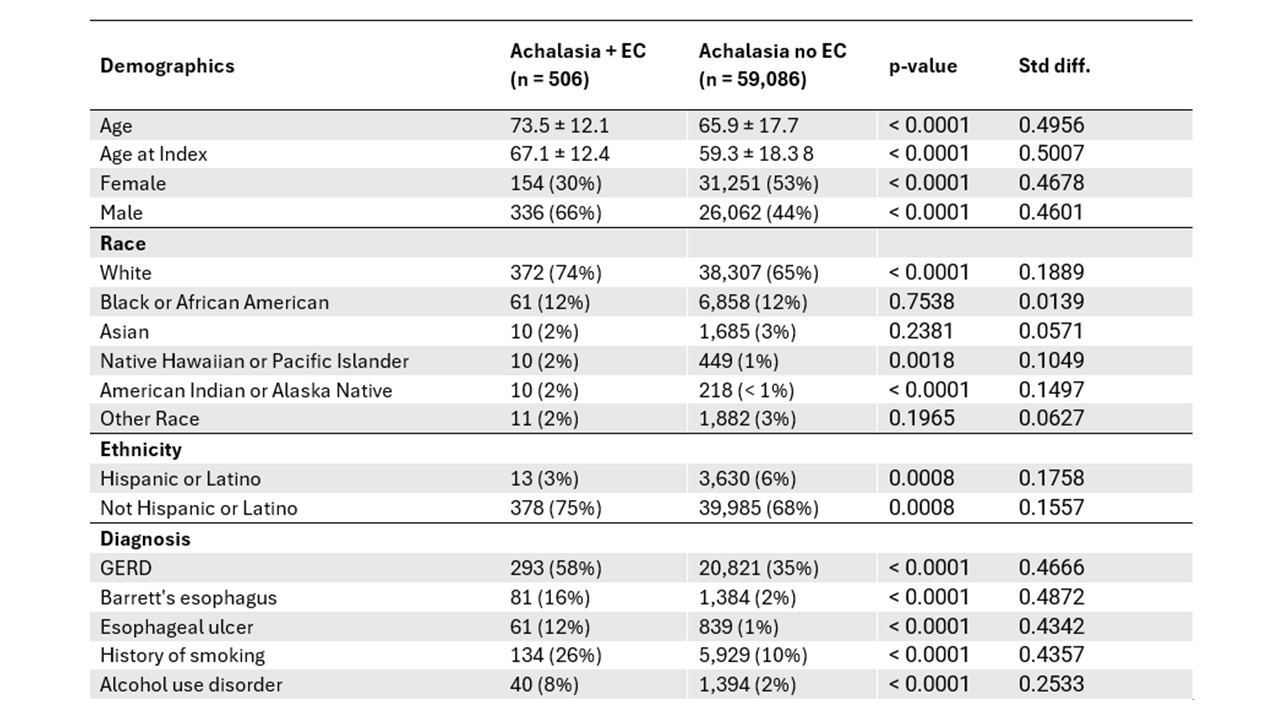
Figure: Table 1: Demographic and Clinical Characteristics
Disclosures:
Julton Tomanguillo indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Jennifer Collins indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Rena Yadlapati: Braintree – Consultant. Medtronic – Consultant. Phathom Pharmaceuticals – Consultant. Reckitt Benckiser – Consultant. RJSMediagnostix – Advisory Committee/Board Member.
Ebubekir Daglilar indicated no relevant financial relationships.
Julton Tomanguillo, MD1, Harleen Chela, MD1, Jennifer Collins, PhD1, Nisar Amin, MD1, Rena Yadlapati, MD2, Ebubekir Daglilar, MD1. P4884 - Risk Factors and Predictors for Esophageal Cancer Among Patients With Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
