Tuesday Poster Session
Category: Esophagus
P4948 - Radical Racial and Gender-Wise Differences in Esophageal Adenocarcinoma (EAC)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Calvin Ghimire, MD (he/him/his)
Princeton Community Hospital/West Virginia University
Princeton, WV
Presenting Author(s)
Calvin Ghimire, MD1, Pujan Kandel, MD2, Bibek Karki, MD, MPH3, Arvind Kunadi, MD4
1Princeton Community Hospital/West Virginia University, Princeton, WV; 2HCA Florida Citrus Memorial Hospital, Gainesville, FL; 3Hurley Medical Center/Michigan State University, Grand Blanc, MI; 4McLaren Flint Hospital, Flint, MI
Introduction: Esophageal adenocarcinoma (EAC) is the most common form of esophageal cancer in the Western world, with its incidence increasing in recent decades. EAC typically develops from a condition known as Barrett's esophagus, where the normal squamous cells of the esophagus are replaced by abnormal columnar cells due to chronic acid reflux or gastroesophageal reflux disease (GERD). EAC is now the most common type of esophageal cancer in the U.S., surpassing squamous cell carcinoma.
Methods: Using the Surveillance, Epidemiology, and End Results (SEER) 22 registry database, we studied EA trends from 2001-2021 based on incidence and incidence-based mortality (IBM). SEER*Stat 8.4.4 was used to get age-adjusted rates for different years based on gender and race. Joinpoint Regression Program, Version 5.3.0.0. November, 2024 was used to analyze the linear regression model.
Results: Esophageal adenocarcinoma incidence and mortality rates show distinct demographic trends. Incidence rates among males fluctuated, rising 2.29% annually (2001–2008), declining 3.15% (2008–2011), then increasing 0.48% (2011–2021). Females experienced a steady 0.7% annual rise throughout. Racial disparities persisted, with white populations having the highest rates, though American Indian/Alaska Natives saw the sharpest recent increase (1.6% annually vs. 1% in whites and 1.3% in Asian/Pacific Islanders).
Incidence Based mortality rates were consistently higher in males, rising 2% annually (2015–2021) compared to 1.3% in females. White populations had the highest mortality, but Black populations faced a 10.4% annual increase (2018–2021), while American Indian/Alaska Natives experienced a sustained 2.8% annual rise (2001–2021). All trends were statistically significant (P< 0.05).
Discussion: In conclusion, the incidence and incidence-based mortality (IBM) rates for esophageal adenocarcinoma exhibit significant variations across gender, race, and time periods. Males, particularly within the white population, experienced higher incidence rates, with recent increases observed in American Indian/Alaska Native populations. While the IBM is notably higher in males, there has been a concerning rise in mortality rates among both males and females, especially among the black and American Indian/Alaska Native populations. These trends underscore the urgent need for targeted prevention, early detection, and intervention strategies, particularly for high-risk groups, to mitigate the growing burden of esophageal adenocarcinoma.

Figure: Incidence rates of esophageal adenocarcinoma
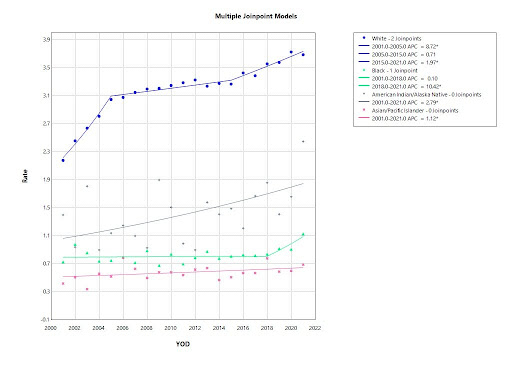
Figure: Incidence rates of esophageal adenocarcinoma
Disclosures:
Calvin Ghimire indicated no relevant financial relationships.
Pujan Kandel indicated no relevant financial relationships.
Bibek Karki indicated no relevant financial relationships.
Arvind Kunadi indicated no relevant financial relationships.
Calvin Ghimire, MD1, Pujan Kandel, MD2, Bibek Karki, MD, MPH3, Arvind Kunadi, MD4. P4948 - Radical Racial and Gender-Wise Differences in Esophageal Adenocarcinoma (EAC), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Princeton Community Hospital/West Virginia University, Princeton, WV; 2HCA Florida Citrus Memorial Hospital, Gainesville, FL; 3Hurley Medical Center/Michigan State University, Grand Blanc, MI; 4McLaren Flint Hospital, Flint, MI
Introduction: Esophageal adenocarcinoma (EAC) is the most common form of esophageal cancer in the Western world, with its incidence increasing in recent decades. EAC typically develops from a condition known as Barrett's esophagus, where the normal squamous cells of the esophagus are replaced by abnormal columnar cells due to chronic acid reflux or gastroesophageal reflux disease (GERD). EAC is now the most common type of esophageal cancer in the U.S., surpassing squamous cell carcinoma.
Methods: Using the Surveillance, Epidemiology, and End Results (SEER) 22 registry database, we studied EA trends from 2001-2021 based on incidence and incidence-based mortality (IBM). SEER*Stat 8.4.4 was used to get age-adjusted rates for different years based on gender and race. Joinpoint Regression Program, Version 5.3.0.0. November, 2024 was used to analyze the linear regression model.
Results: Esophageal adenocarcinoma incidence and mortality rates show distinct demographic trends. Incidence rates among males fluctuated, rising 2.29% annually (2001–2008), declining 3.15% (2008–2011), then increasing 0.48% (2011–2021). Females experienced a steady 0.7% annual rise throughout. Racial disparities persisted, with white populations having the highest rates, though American Indian/Alaska Natives saw the sharpest recent increase (1.6% annually vs. 1% in whites and 1.3% in Asian/Pacific Islanders).
Incidence Based mortality rates were consistently higher in males, rising 2% annually (2015–2021) compared to 1.3% in females. White populations had the highest mortality, but Black populations faced a 10.4% annual increase (2018–2021), while American Indian/Alaska Natives experienced a sustained 2.8% annual rise (2001–2021). All trends were statistically significant (P< 0.05).
Discussion: In conclusion, the incidence and incidence-based mortality (IBM) rates for esophageal adenocarcinoma exhibit significant variations across gender, race, and time periods. Males, particularly within the white population, experienced higher incidence rates, with recent increases observed in American Indian/Alaska Native populations. While the IBM is notably higher in males, there has been a concerning rise in mortality rates among both males and females, especially among the black and American Indian/Alaska Native populations. These trends underscore the urgent need for targeted prevention, early detection, and intervention strategies, particularly for high-risk groups, to mitigate the growing burden of esophageal adenocarcinoma.

Figure: Incidence rates of esophageal adenocarcinoma
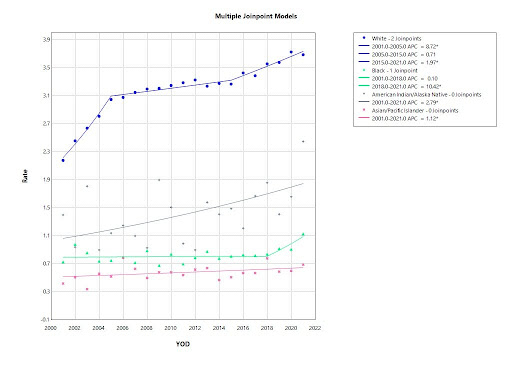
Figure: Incidence rates of esophageal adenocarcinoma
Disclosures:
Calvin Ghimire indicated no relevant financial relationships.
Pujan Kandel indicated no relevant financial relationships.
Bibek Karki indicated no relevant financial relationships.
Arvind Kunadi indicated no relevant financial relationships.
Calvin Ghimire, MD1, Pujan Kandel, MD2, Bibek Karki, MD, MPH3, Arvind Kunadi, MD4. P4948 - Radical Racial and Gender-Wise Differences in Esophageal Adenocarcinoma (EAC), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
