Tuesday Poster Session
Category: Esophagus
P5048 - Hemophilia Masquerading as Cancer: Extraluminal Esophageal Hematoma in a Young Male
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Imroz Apon, MD (he/him/his)
United Health Services, Wilson Medical Center
Vestal, NY
Presenting Author(s)
Imroz Apon, MD1, Khandokar A. Talib, MD1, Ahmed Shehadah, MD2, Gowthami Ramar, MD1, Hammad Qadri, DO1, Rahat Elahi, 3, Amanke Oranu, MD2, Toseef Javaid, MD4
1United Health Services, Wilson Medical Center, Vestal, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3SUNY Downstate Health Sciences University, East Elmhurst, NY; 4United Health Services, Wilson Medical Center, Johnson City, NY
Introduction: Acute Onset Dysphagia raises concerns of esophageal obstruction due to malignancy, strictures, or external compression. We presented a unique case of sudden onset dysphagia due to extraluminal compression of the esophagus, presumed to be caused by a spontaneous mediastinal hematoma in a patient with hemophilia B.
Case Description/
Methods: A 34-year-old male with a history of hemophilia on recombinant factor IX presented with complaints of acute dysphagia to both solids and liquids. The patient had a preceding 3-day history of respiratory illness with a productive cough and low-grade fever. Initial imaging was significant for right basilar opacity and was managed with antibiotics. During hospitalization, CT imaging was significant for a posterior mediastinal mass causing esophageal compression (Figure 2) and hepatic lesions. Upper Endoscopy did not show any intraluminal mass in the esophagus, and an external compression with mucosal discoloration was noted in the mid-distal esophagus (Figure 1). Endoscopic Ultrasound revealed multiple large hypoechoic posterior mediastinal lesions with necrosis. Fine Needle Aspiration biopsy showed hypercellular specimen with fibrosis/sclerosis and few atypical cells but no malignancy. Tumor markers (Alpha-Fetoprotein, beta-human chorionic gonadotropin) were normal. MRI reaffirmed the presence of a posterior mediastinal mass. Following discharge, the patient had spontaneous resolution of symptoms with radiological reduction in mass size on serial imaging. A thoracoscopic biopsy was planned but was deferred due to possible further contained mediastinal hematoma development. Spontaneous regression of mediastinal mass and absence of B symptoms suggested that the compression was likely due to hematoma, possibly triggered by vigorous cough-related vascular injury in the setting of hemophilia B rather than malignancy. The patient was managed and improved with supportive care and factor IX replacement.
Discussion: This case highlights the importance of considering spontaneous mediastinal hematoma as a rare but significant cause of dysphagia, particularly in patients with underlying coagulopathies. Recognizing nonmalignant causes of extraluminal esophageal compression is crucial to prevent unnecessary invasive interventions, and ensure timely, etiology-specific management. Early identification through appropriate imaging and clinical correlation can facilitate conservative treatment and improve outcomes in this uncommon but clinically relevant scenario.
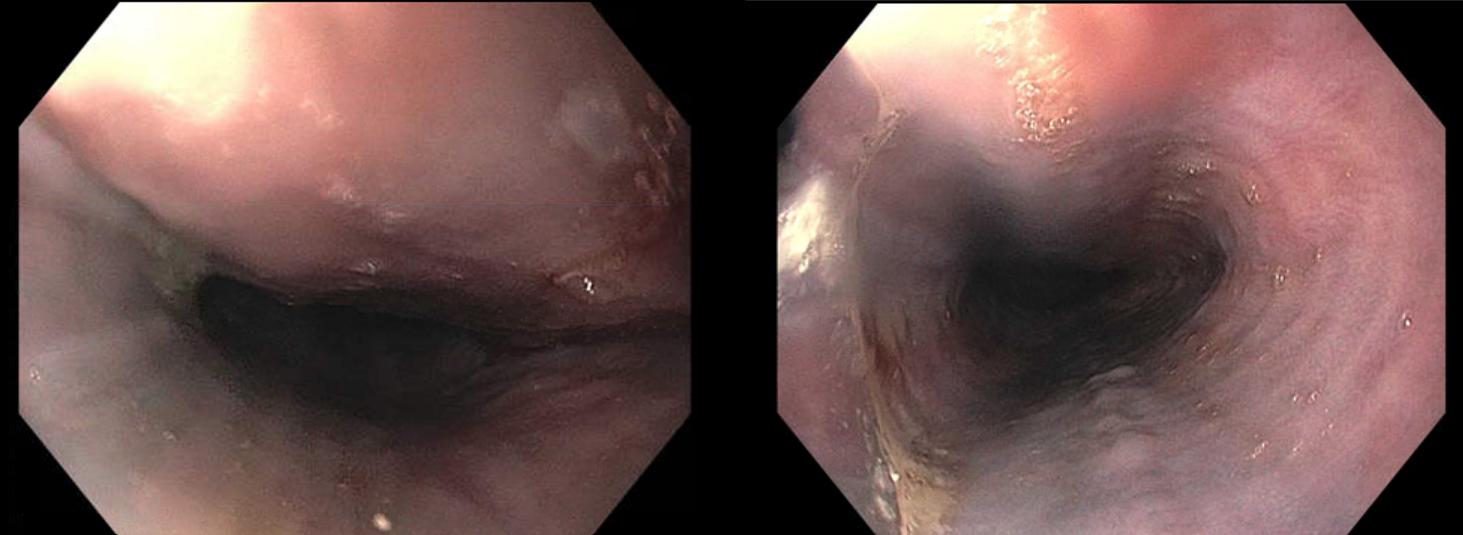
Figure: Figure 1: An external compression with mucosal discoloration in the mid-distal esophagus. No intraluminal mass in the esophagus.
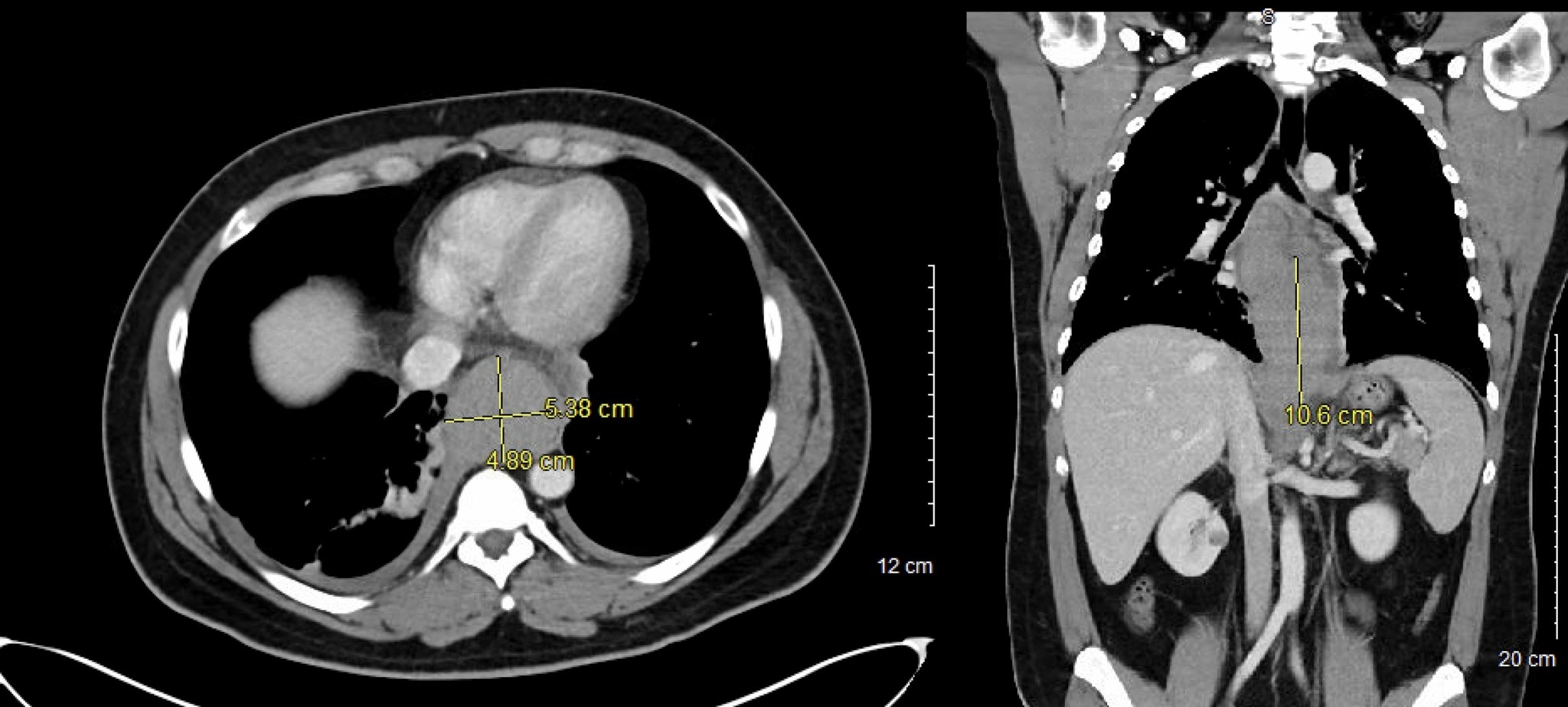
Figure: Figure 2: Posterior mediastinal in the Subcarinal region extending into the Gastroesophageal junction and upper part of the lower abdomen measuring 4.9 x 5.4 x 10.6 cm.
Disclosures:
Imroz Apon indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Rahat Elahi indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Imroz Apon, MD1, Khandokar A. Talib, MD1, Ahmed Shehadah, MD2, Gowthami Ramar, MD1, Hammad Qadri, DO1, Rahat Elahi, 3, Amanke Oranu, MD2, Toseef Javaid, MD4. P5048 - Hemophilia Masquerading as Cancer: Extraluminal Esophageal Hematoma in a Young Male, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Vestal, NY; 2United Health Services, Wilson Medical Center, Binghamton, NY; 3SUNY Downstate Health Sciences University, East Elmhurst, NY; 4United Health Services, Wilson Medical Center, Johnson City, NY
Introduction: Acute Onset Dysphagia raises concerns of esophageal obstruction due to malignancy, strictures, or external compression. We presented a unique case of sudden onset dysphagia due to extraluminal compression of the esophagus, presumed to be caused by a spontaneous mediastinal hematoma in a patient with hemophilia B.
Case Description/
Methods: A 34-year-old male with a history of hemophilia on recombinant factor IX presented with complaints of acute dysphagia to both solids and liquids. The patient had a preceding 3-day history of respiratory illness with a productive cough and low-grade fever. Initial imaging was significant for right basilar opacity and was managed with antibiotics. During hospitalization, CT imaging was significant for a posterior mediastinal mass causing esophageal compression (Figure 2) and hepatic lesions. Upper Endoscopy did not show any intraluminal mass in the esophagus, and an external compression with mucosal discoloration was noted in the mid-distal esophagus (Figure 1). Endoscopic Ultrasound revealed multiple large hypoechoic posterior mediastinal lesions with necrosis. Fine Needle Aspiration biopsy showed hypercellular specimen with fibrosis/sclerosis and few atypical cells but no malignancy. Tumor markers (Alpha-Fetoprotein, beta-human chorionic gonadotropin) were normal. MRI reaffirmed the presence of a posterior mediastinal mass. Following discharge, the patient had spontaneous resolution of symptoms with radiological reduction in mass size on serial imaging. A thoracoscopic biopsy was planned but was deferred due to possible further contained mediastinal hematoma development. Spontaneous regression of mediastinal mass and absence of B symptoms suggested that the compression was likely due to hematoma, possibly triggered by vigorous cough-related vascular injury in the setting of hemophilia B rather than malignancy. The patient was managed and improved with supportive care and factor IX replacement.
Discussion: This case highlights the importance of considering spontaneous mediastinal hematoma as a rare but significant cause of dysphagia, particularly in patients with underlying coagulopathies. Recognizing nonmalignant causes of extraluminal esophageal compression is crucial to prevent unnecessary invasive interventions, and ensure timely, etiology-specific management. Early identification through appropriate imaging and clinical correlation can facilitate conservative treatment and improve outcomes in this uncommon but clinically relevant scenario.
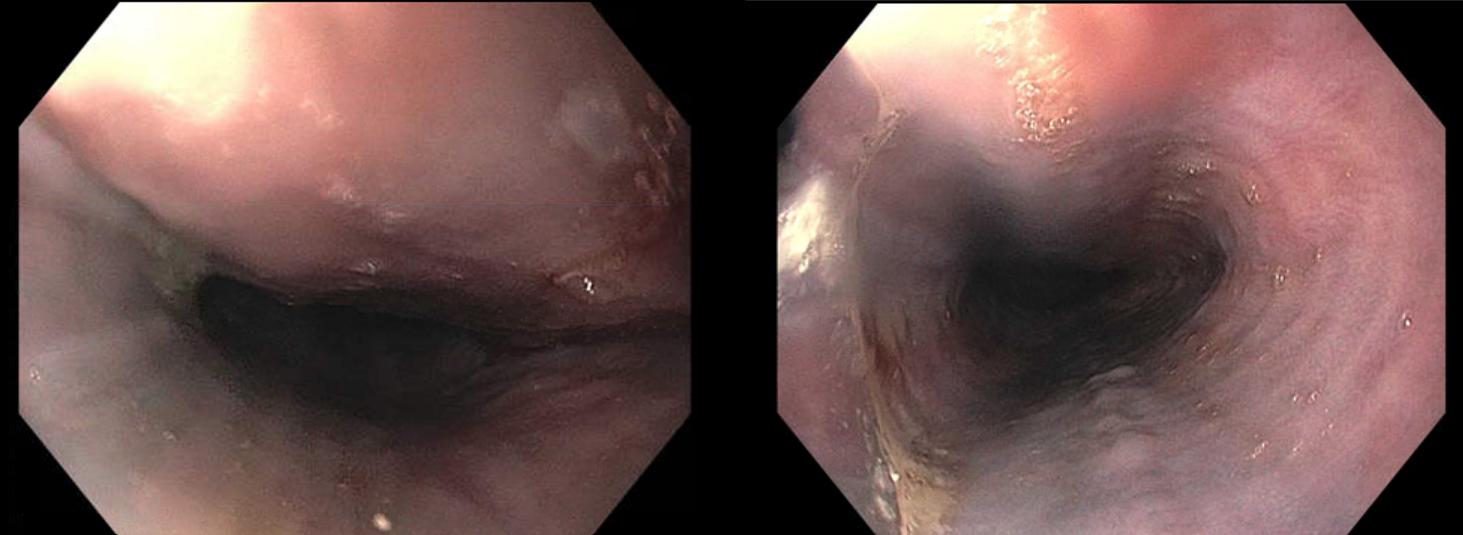
Figure: Figure 1: An external compression with mucosal discoloration in the mid-distal esophagus. No intraluminal mass in the esophagus.
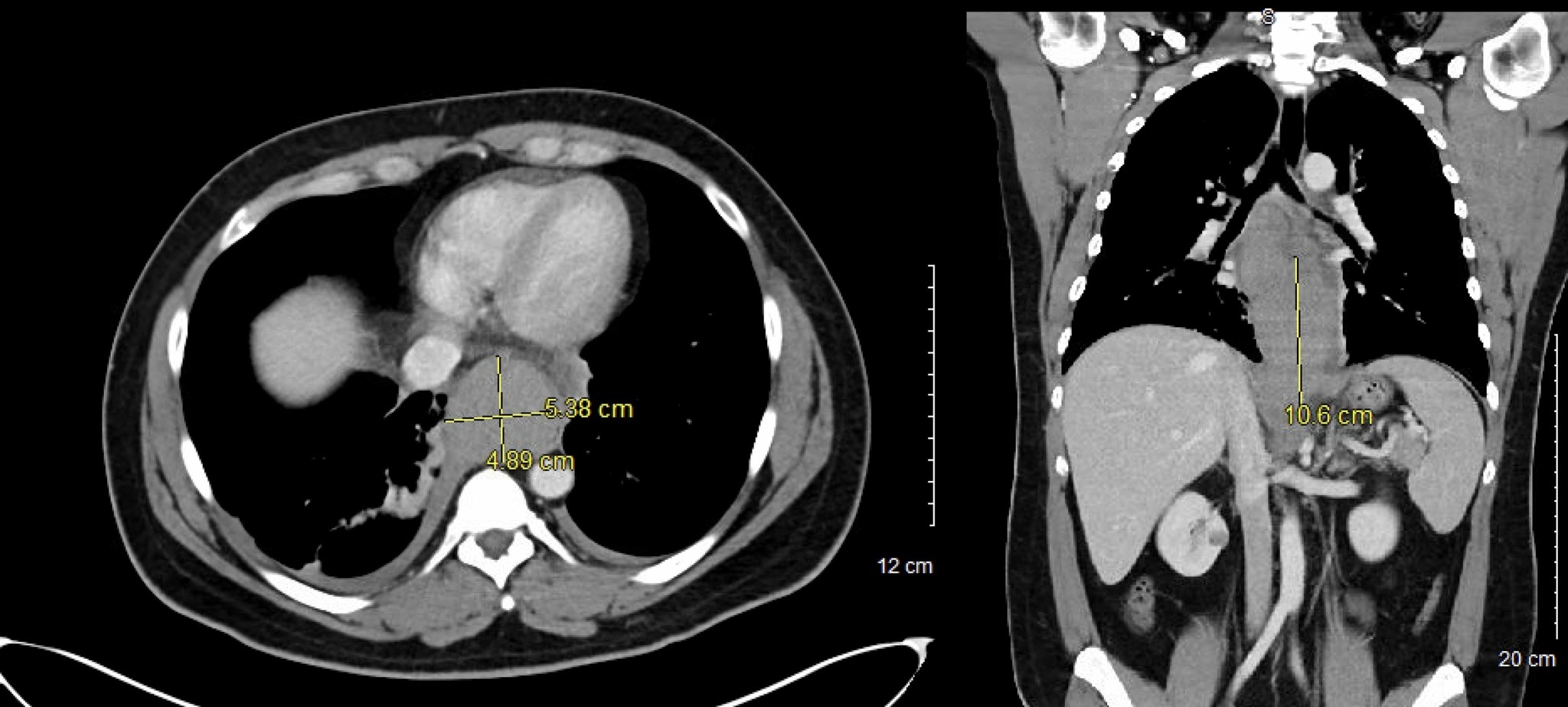
Figure: Figure 2: Posterior mediastinal in the Subcarinal region extending into the Gastroesophageal junction and upper part of the lower abdomen measuring 4.9 x 5.4 x 10.6 cm.
Disclosures:
Imroz Apon indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Rahat Elahi indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Imroz Apon, MD1, Khandokar A. Talib, MD1, Ahmed Shehadah, MD2, Gowthami Ramar, MD1, Hammad Qadri, DO1, Rahat Elahi, 3, Amanke Oranu, MD2, Toseef Javaid, MD4. P5048 - Hemophilia Masquerading as Cancer: Extraluminal Esophageal Hematoma in a Young Male, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
