Tuesday Poster Session
Category: Esophagus
P5040 - A Case Report of Idiopathic Esophageal Ulcer in a Renal Transplant Patient Responsive to Steroid Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ingrid Hirte, MD (she/her/hers)
Mayo Clinic
Byron, MN
Presenting Author(s)
Ingrid Hirte, MD1, Riya Gupta, MBBS2, Sarah Khan, MD2, Xiao Jing Wang, MD2
1Mayo Clinic, Byron, MN; 2Mayo Clinic, Rochester, MN
Introduction: Idiopathic giant esophageal ulcers have been reported most often in patients with HIV/AIDS but only four cases have been reported in HIV negative patients. We describe a case of idiopathic esophageal ulceration ultimately responsive to steroid therapy in an immunosuppressed, HIV-negative renal transplant patient.
Case Description/
Methods: A 59-year-old female with renal transplant in 2023 for ADPKD presented with odynophagia after a week-long course of doxycycline for outpatient pneumonia treatment. EGD was unremarkable and her symptoms improved. Five weeks later she developed epigastric and right upper quadrant pain. Endoscopy showed an ulcer encompassing 50% of the esophageal circumference with heaped margins in the mid-esophagus. Serologies and tissue samples from the esophageal ulcer were negative for malignancy and infectious etiologies. Celiac testing was negative and biopsies from small and large bowel were negative for infectious, malignant and autoimmune conditions. She was initially treated with daily pantoprazole, famotidine, sucralfate and an NG tube was placed for nutrition. Her odynophagia continued and a month later repeat EGD showed persistence of the ulcer for which Vonoprazan was started. Repeat biopsies continued to be negative for infection or malignancy. Acyclovir was initiated and NG tube was transitioned to a PEG tube to facilitate healing. Despite these efforts, her odynophagia continued. Due to suspicion for idiopathic giant esophageal ulcer, she was trialed on a prednisone taper of 40 mg, decreasing by 10 mg each week. Repeat EGD after completion of the steroid course showed ulcer healing and patient odynophagia had improved.
Discussion: In the literature, cases of idiopathic esophageal ulcer in HIV patients respond well to therapy with steroids, however the basis for steroid efficacy in treating these ulcers is unknown. Previously successful prednisone regimens have consisted of 40 mg/day tapering by 10 mg/week. For this patient, she improved both symptomatically and endoscopically with the use of this proposed steroid regimen after months of failed alternative therapies that would otherwise treat common causes of esophagitis or ulcers. Idiopathic esophageal ulcer should be considered on the differential for esophageal ulceration in solid organ transplant recipients. In immunocompromised patients who have esophageal ulcers refractory to standard therapy, a trial of steroids should be considered for treatment when infectious and autoimmune etiologies are ruled out.

Figure: Initial endoscopic findings of esophageal ulcer
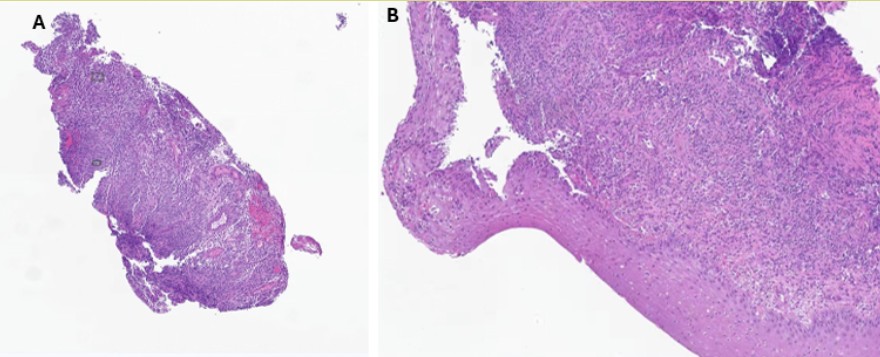
Figure: Pathology Report of Tissue Biopsies:
A: Ulcer with granulation tissue. Typical granulation in response to injury with hyperplastic vessels, fibrosis and inflammatory cells. Inflammation is non-specific. No findings of malignancy but otherwise no specific etiology is suggested
B: Normal mucosal lining with overlying infiltrate. Staining for CMV, HSV, VZV, EBV negative. No fungal organisms visualized.
Disclosures:
Ingrid Hirte indicated no relevant financial relationships.
Riya Gupta indicated no relevant financial relationships.
Sarah Khan indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Ingrid Hirte, MD1, Riya Gupta, MBBS2, Sarah Khan, MD2, Xiao Jing Wang, MD2. P5040 - A Case Report of Idiopathic Esophageal Ulcer in a Renal Transplant Patient Responsive to Steroid Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Byron, MN; 2Mayo Clinic, Rochester, MN
Introduction: Idiopathic giant esophageal ulcers have been reported most often in patients with HIV/AIDS but only four cases have been reported in HIV negative patients. We describe a case of idiopathic esophageal ulceration ultimately responsive to steroid therapy in an immunosuppressed, HIV-negative renal transplant patient.
Case Description/
Methods: A 59-year-old female with renal transplant in 2023 for ADPKD presented with odynophagia after a week-long course of doxycycline for outpatient pneumonia treatment. EGD was unremarkable and her symptoms improved. Five weeks later she developed epigastric and right upper quadrant pain. Endoscopy showed an ulcer encompassing 50% of the esophageal circumference with heaped margins in the mid-esophagus. Serologies and tissue samples from the esophageal ulcer were negative for malignancy and infectious etiologies. Celiac testing was negative and biopsies from small and large bowel were negative for infectious, malignant and autoimmune conditions. She was initially treated with daily pantoprazole, famotidine, sucralfate and an NG tube was placed for nutrition. Her odynophagia continued and a month later repeat EGD showed persistence of the ulcer for which Vonoprazan was started. Repeat biopsies continued to be negative for infection or malignancy. Acyclovir was initiated and NG tube was transitioned to a PEG tube to facilitate healing. Despite these efforts, her odynophagia continued. Due to suspicion for idiopathic giant esophageal ulcer, she was trialed on a prednisone taper of 40 mg, decreasing by 10 mg each week. Repeat EGD after completion of the steroid course showed ulcer healing and patient odynophagia had improved.
Discussion: In the literature, cases of idiopathic esophageal ulcer in HIV patients respond well to therapy with steroids, however the basis for steroid efficacy in treating these ulcers is unknown. Previously successful prednisone regimens have consisted of 40 mg/day tapering by 10 mg/week. For this patient, she improved both symptomatically and endoscopically with the use of this proposed steroid regimen after months of failed alternative therapies that would otherwise treat common causes of esophagitis or ulcers. Idiopathic esophageal ulcer should be considered on the differential for esophageal ulceration in solid organ transplant recipients. In immunocompromised patients who have esophageal ulcers refractory to standard therapy, a trial of steroids should be considered for treatment when infectious and autoimmune etiologies are ruled out.

Figure: Initial endoscopic findings of esophageal ulcer
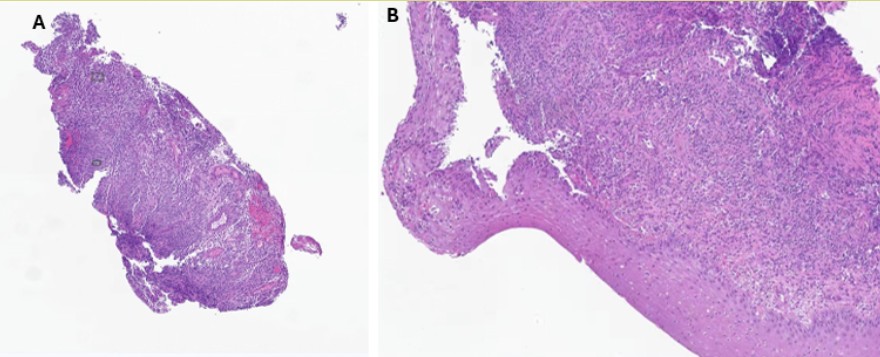
Figure: Pathology Report of Tissue Biopsies:
A: Ulcer with granulation tissue. Typical granulation in response to injury with hyperplastic vessels, fibrosis and inflammatory cells. Inflammation is non-specific. No findings of malignancy but otherwise no specific etiology is suggested
B: Normal mucosal lining with overlying infiltrate. Staining for CMV, HSV, VZV, EBV negative. No fungal organisms visualized.
Disclosures:
Ingrid Hirte indicated no relevant financial relationships.
Riya Gupta indicated no relevant financial relationships.
Sarah Khan indicated no relevant financial relationships.
Xiao Jing Wang indicated no relevant financial relationships.
Ingrid Hirte, MD1, Riya Gupta, MBBS2, Sarah Khan, MD2, Xiao Jing Wang, MD2. P5040 - A Case Report of Idiopathic Esophageal Ulcer in a Renal Transplant Patient Responsive to Steroid Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
