Tuesday Poster Session
Category: Esophagus
P5039 - Small Cell, Big Impact: A Rare Case of Dysphagia and Dyspnea Secondary to Mediastinal Small Cell Esophageal Carcinoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jared Fehlman, MD (he/him/his)
Huntington Hospital
Pasadena, CA
Presenting Author(s)
Jared Fehlman, MD, Myrna Mousa, MD, Rajkumar Dasgupta, MD
Huntington Hospital, Pasadena, CA
Introduction: Making up less than 3% of all esophageal malignancies, small cell carcinoma of the esophagus (SCEC) is a very rare cause of esophageal malignancy. It often develops in the lower and middle part of the esophagus and is highly invasive and aggressive. Radiographic findings include esophageal wall thickening, narrowing of the lumen, and enlargement of regional lymph nodes. In this case, the mass effect from the circumferential mass resulted in hoarseness of breath, tracheal compression, and dysphagia.
Case Description/
Methods: A 42-year-old male with no past medical history presents with worsening shortness of breath predominantly in the supine position, tightness in the throat and upper chest, dysphagia and gradual loss of voice. The patient saw pulmonology and otolaryngology (ENT) and was diagnosed with obstructive sleep apnea and vocal cord paralysis. An outpatient CT scan of the head and neck was ordered which showed possible mediastinal mass prompting the patient’s ENT to refer him to the ED for worsening symptoms. In the ED, CT scan revealed a 6.3 x 7.1 x 6.9 cm mediastinal mass displacing the esophagus and trachea. Patient subsequently underwent bronchoscopy which showed narrowing of the upper airway and esophagoscopy (EGD) identified circumferential ulcerated mass. This finding prompted a biopsy that confirmed diagnosis of small cell carcinoma. Because of impending respiratory distress, the patient underwent an open tracheostomy. Oncology was consulted and started cisplatin and etoposide. To manage dysphagia, GI placed an esophageal stent.
Discussion: This case serves as an important teaching point to highlight a unique cause of dysphagia and dyspnea. Not only is primary SCEC rare, but this presentation in the posterior mediastinum, and higher in the esophagus lead to a constellation of symptoms and risks not traditionally seen in SCEC. The mass effect seen in our patient made the initial diagnosis in our patient challenging and clinicians should be aware of the potential for airway compromise when approaching biopsy and have a plan in place for managing it. Ultimately, the complexity of the case required a multidisciplinary approach among critical care, gastroenterology, otolaryngology, thoracic surgery and oncology.
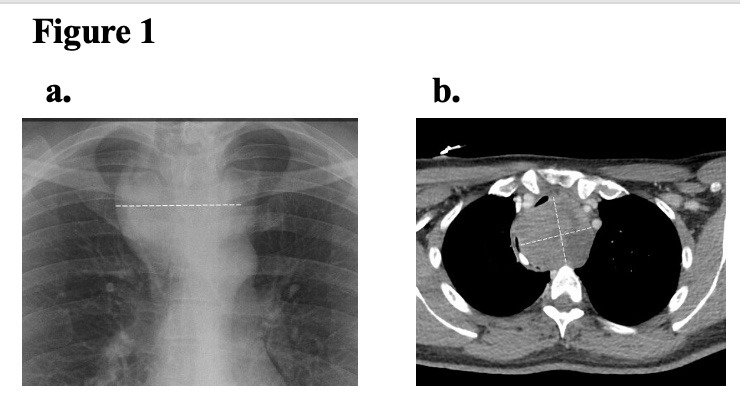
Figure: Figure 1A. Initial chest x-ray showing esophageal mass 2B. CT chest, abdomen, pelvis with contrast demonstrating mass
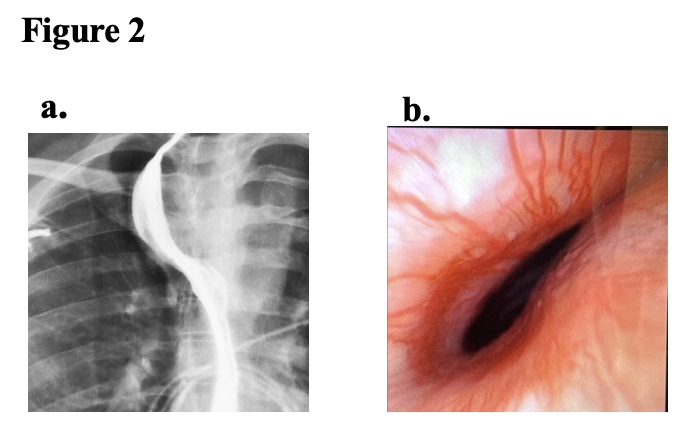
Figure: Figure 2A. Barium esophagram demonstrating esophageal displacement secondary to mass effect 2B. Airway compression visualized on bronchoscopy secondary to mass effect
Disclosures:
Jared Fehlman indicated no relevant financial relationships.
Myrna Mousa indicated no relevant financial relationships.
Rajkumar Dasgupta: ANI pharmaceuticals – Speakers Bureau. Baxter – Speakers Bureau. Gilead – Speakers Bureau. GSK – Speakers Bureau. Idorsia – Speakers Bureau. La Jolla – Speakers Bureau. Mallinckrodt – Speakers Bureau. MERCK – Speakers Bureau.
Jared Fehlman, MD, Myrna Mousa, MD, Rajkumar Dasgupta, MD. P5039 - Small Cell, Big Impact: A Rare Case of Dysphagia and Dyspnea Secondary to Mediastinal Small Cell Esophageal Carcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Huntington Hospital, Pasadena, CA
Introduction: Making up less than 3% of all esophageal malignancies, small cell carcinoma of the esophagus (SCEC) is a very rare cause of esophageal malignancy. It often develops in the lower and middle part of the esophagus and is highly invasive and aggressive. Radiographic findings include esophageal wall thickening, narrowing of the lumen, and enlargement of regional lymph nodes. In this case, the mass effect from the circumferential mass resulted in hoarseness of breath, tracheal compression, and dysphagia.
Case Description/
Methods: A 42-year-old male with no past medical history presents with worsening shortness of breath predominantly in the supine position, tightness in the throat and upper chest, dysphagia and gradual loss of voice. The patient saw pulmonology and otolaryngology (ENT) and was diagnosed with obstructive sleep apnea and vocal cord paralysis. An outpatient CT scan of the head and neck was ordered which showed possible mediastinal mass prompting the patient’s ENT to refer him to the ED for worsening symptoms. In the ED, CT scan revealed a 6.3 x 7.1 x 6.9 cm mediastinal mass displacing the esophagus and trachea. Patient subsequently underwent bronchoscopy which showed narrowing of the upper airway and esophagoscopy (EGD) identified circumferential ulcerated mass. This finding prompted a biopsy that confirmed diagnosis of small cell carcinoma. Because of impending respiratory distress, the patient underwent an open tracheostomy. Oncology was consulted and started cisplatin and etoposide. To manage dysphagia, GI placed an esophageal stent.
Discussion: This case serves as an important teaching point to highlight a unique cause of dysphagia and dyspnea. Not only is primary SCEC rare, but this presentation in the posterior mediastinum, and higher in the esophagus lead to a constellation of symptoms and risks not traditionally seen in SCEC. The mass effect seen in our patient made the initial diagnosis in our patient challenging and clinicians should be aware of the potential for airway compromise when approaching biopsy and have a plan in place for managing it. Ultimately, the complexity of the case required a multidisciplinary approach among critical care, gastroenterology, otolaryngology, thoracic surgery and oncology.
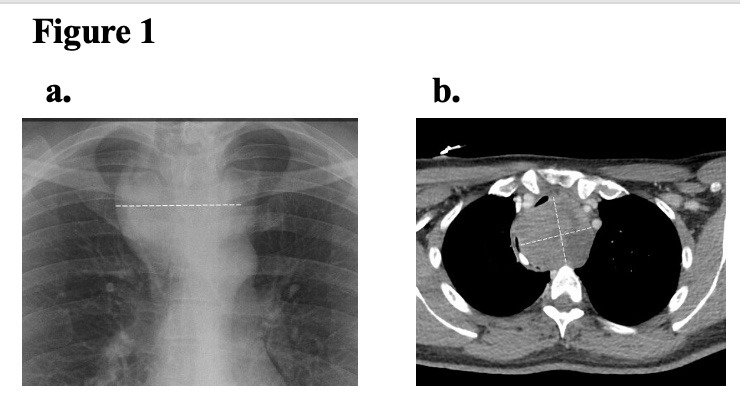
Figure: Figure 1A. Initial chest x-ray showing esophageal mass 2B. CT chest, abdomen, pelvis with contrast demonstrating mass
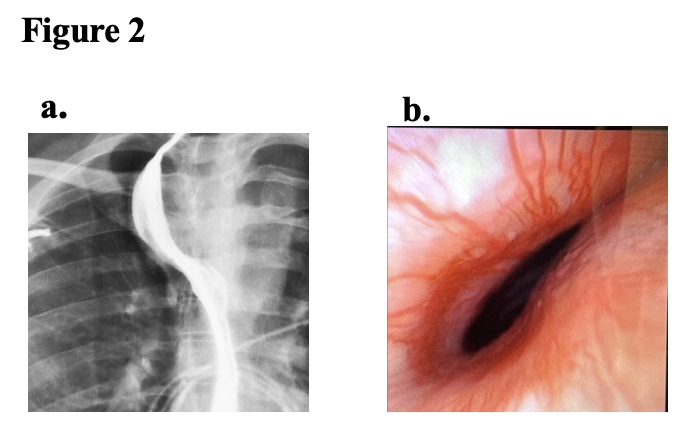
Figure: Figure 2A. Barium esophagram demonstrating esophageal displacement secondary to mass effect 2B. Airway compression visualized on bronchoscopy secondary to mass effect
Disclosures:
Jared Fehlman indicated no relevant financial relationships.
Myrna Mousa indicated no relevant financial relationships.
Rajkumar Dasgupta: ANI pharmaceuticals – Speakers Bureau. Baxter – Speakers Bureau. Gilead – Speakers Bureau. GSK – Speakers Bureau. Idorsia – Speakers Bureau. La Jolla – Speakers Bureau. Mallinckrodt – Speakers Bureau. MERCK – Speakers Bureau.
Jared Fehlman, MD, Myrna Mousa, MD, Rajkumar Dasgupta, MD. P5039 - Small Cell, Big Impact: A Rare Case of Dysphagia and Dyspnea Secondary to Mediastinal Small Cell Esophageal Carcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
