Tuesday Poster Session
Category: Esophagus
P5036 - Unmasking the Uncommon: A Case Report of Esophagitis Caused by Herpes Simplex Virus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark R. Baniqued, MD
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Christina Sisliyan, DO1, Soonwook Hong, MD2, Daniel Cole, MD, MPH1
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Herpes Simplex Virus (HSV)-associated diseases are among the most common viral infections, affecting many adults worldwide. HSV-1 primarily causes non-genital infections, while HSV-2 causes genital infections. Rarely, HSV manifests as esophagitis, which is particularly uncommon, with only a few documented cases. We present a case of extensive HSV-1 and HSV-2 esophagitis, confirmed by biopsy, in a patient admitted for sepsis.
Case Description/
Methods: A 51-year-old male with a history of gastroesophageal reflux disease, chronic kidney disease, and heart failure presented with altered mental status. He was hypotensive and tachycardic with leukocytosis. He was fluid resuscitated and started on empiric antibiotics, ceftriaxone and vancomycin. Blood cultures identified Gram-positive cocci, and an echocardiogram showed a cardiac thrombus. Thus, he was started on a continuous heparin drip. That night, he developed coffee ground emesis, followed by overt hematemesis the next morning, and his hemoglobin decreased from 11.6 g/dL on admission to 8.2 g/dL. Gastroenterology recommended esophagogastroduodenoscopy (EGD) and twice-daily intravenous (IV) 40 mg proton pump inhibitor (PPI), advising to hold the heparin drip while coordinating with Cardiology. EGD was performed, revealing severe esophagitis with long segments of ulceration from 25 cm to 40 cm from the incisors (Figure 1). Multiple biopsies were taken, and he started a continuous PPI drip for 72 hours, followed by IV PPI twice daily. He was started on sucralfate four times daily for 14 days, and heparin was held as safely as possible, pending a repeat EGD in two months. Days later, biopsies were negative for Helicobacter Pylori and malignancy, but the esophageal biopsies raised concerns for HSV, with immunostaining positive for both HSV-1 and HSV-2. He had no further episodes of hematemesis, and his hemoglobin remained stable. The patient left the hospital against medical advice and was lost to follow-up.
Discussion: HSV esophagitis presents with odynophagia, dysphagia, and chest pain. Gastrointestinal bleeding is seen in one-third of cases. Diagnosis is based on endoscopy and confirmed by histopathology, with immunostaining as additional support. Endoscopic signs include friable mucosa, ulceration, and white exudates in the distal esophagus. Treatment lacks consensus, but like other esophagitis types, it often involves PPI. Some studies suggest oral or IV acyclovir may ease symptoms, while others suggest the condition is self-limiting.
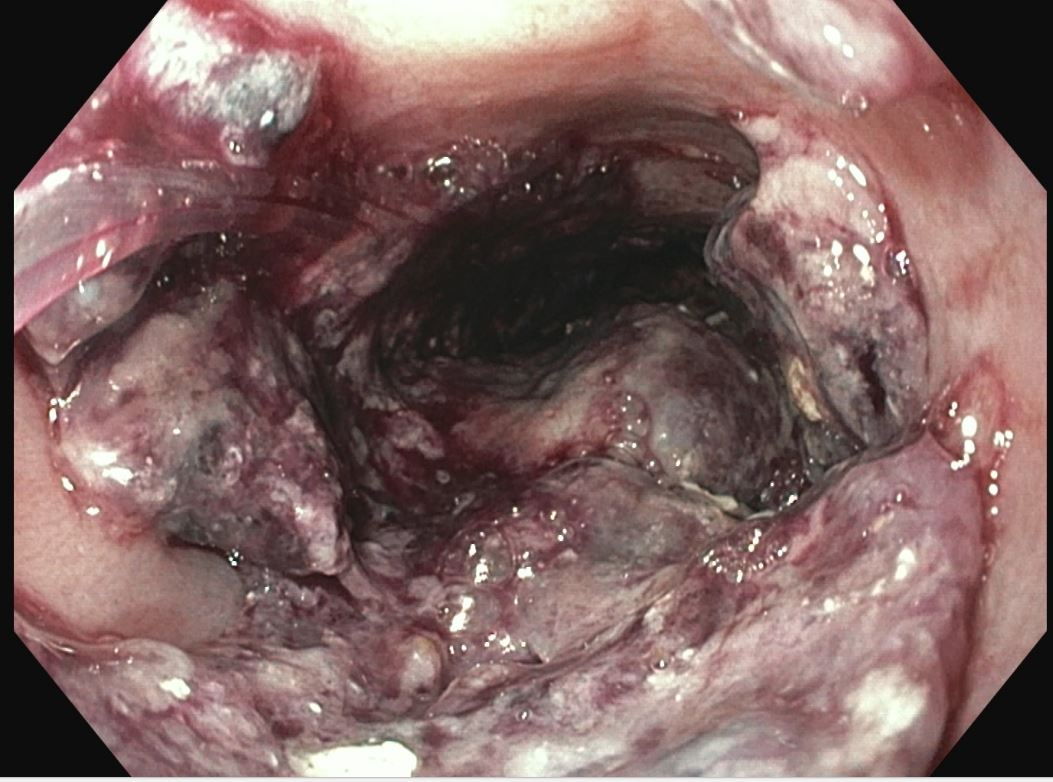
Figure: 1A: Esophagus Mucosa Severe (LA Class D) ulcerative esophagitis with spontaneous bleeding seen throughout the esophagus starting at 25 cm and going up to 40 cm from the incisors. The GEJ appeared to be at 40 cm and the diaphragmatic pinch was at 45cm compatible with a 5cm hiatal hernia.
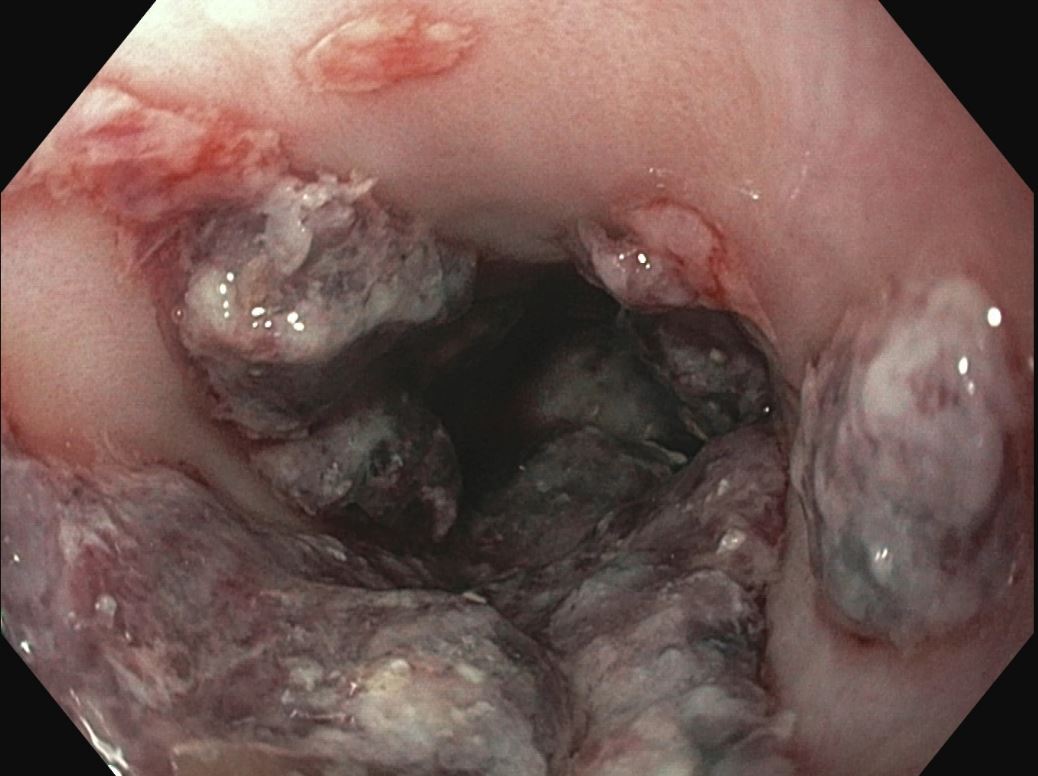
Figure: 1B
Disclosures:
Mark Baniqued indicated no relevant financial relationships.
Rhett Harmon indicated no relevant financial relationships.
Christina Sisliyan indicated no relevant financial relationships.
Soonwook Hong indicated no relevant financial relationships.
Daniel Cole indicated no relevant financial relationships.
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Christina Sisliyan, DO1, Soonwook Hong, MD2, Daniel Cole, MD, MPH1. P5036 - Unmasking the Uncommon: A Case Report of Esophagitis Caused by Herpes Simplex Virus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Herpes Simplex Virus (HSV)-associated diseases are among the most common viral infections, affecting many adults worldwide. HSV-1 primarily causes non-genital infections, while HSV-2 causes genital infections. Rarely, HSV manifests as esophagitis, which is particularly uncommon, with only a few documented cases. We present a case of extensive HSV-1 and HSV-2 esophagitis, confirmed by biopsy, in a patient admitted for sepsis.
Case Description/
Methods: A 51-year-old male with a history of gastroesophageal reflux disease, chronic kidney disease, and heart failure presented with altered mental status. He was hypotensive and tachycardic with leukocytosis. He was fluid resuscitated and started on empiric antibiotics, ceftriaxone and vancomycin. Blood cultures identified Gram-positive cocci, and an echocardiogram showed a cardiac thrombus. Thus, he was started on a continuous heparin drip. That night, he developed coffee ground emesis, followed by overt hematemesis the next morning, and his hemoglobin decreased from 11.6 g/dL on admission to 8.2 g/dL. Gastroenterology recommended esophagogastroduodenoscopy (EGD) and twice-daily intravenous (IV) 40 mg proton pump inhibitor (PPI), advising to hold the heparin drip while coordinating with Cardiology. EGD was performed, revealing severe esophagitis with long segments of ulceration from 25 cm to 40 cm from the incisors (Figure 1). Multiple biopsies were taken, and he started a continuous PPI drip for 72 hours, followed by IV PPI twice daily. He was started on sucralfate four times daily for 14 days, and heparin was held as safely as possible, pending a repeat EGD in two months. Days later, biopsies were negative for Helicobacter Pylori and malignancy, but the esophageal biopsies raised concerns for HSV, with immunostaining positive for both HSV-1 and HSV-2. He had no further episodes of hematemesis, and his hemoglobin remained stable. The patient left the hospital against medical advice and was lost to follow-up.
Discussion: HSV esophagitis presents with odynophagia, dysphagia, and chest pain. Gastrointestinal bleeding is seen in one-third of cases. Diagnosis is based on endoscopy and confirmed by histopathology, with immunostaining as additional support. Endoscopic signs include friable mucosa, ulceration, and white exudates in the distal esophagus. Treatment lacks consensus, but like other esophagitis types, it often involves PPI. Some studies suggest oral or IV acyclovir may ease symptoms, while others suggest the condition is self-limiting.
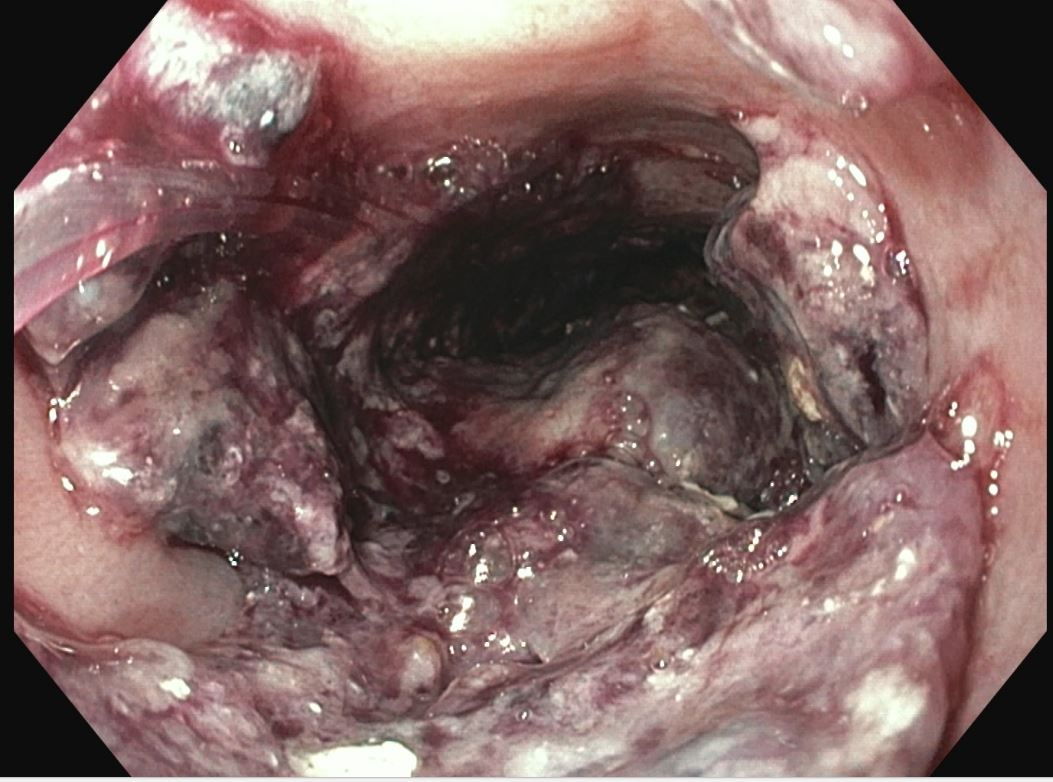
Figure: 1A: Esophagus Mucosa Severe (LA Class D) ulcerative esophagitis with spontaneous bleeding seen throughout the esophagus starting at 25 cm and going up to 40 cm from the incisors. The GEJ appeared to be at 40 cm and the diaphragmatic pinch was at 45cm compatible with a 5cm hiatal hernia.
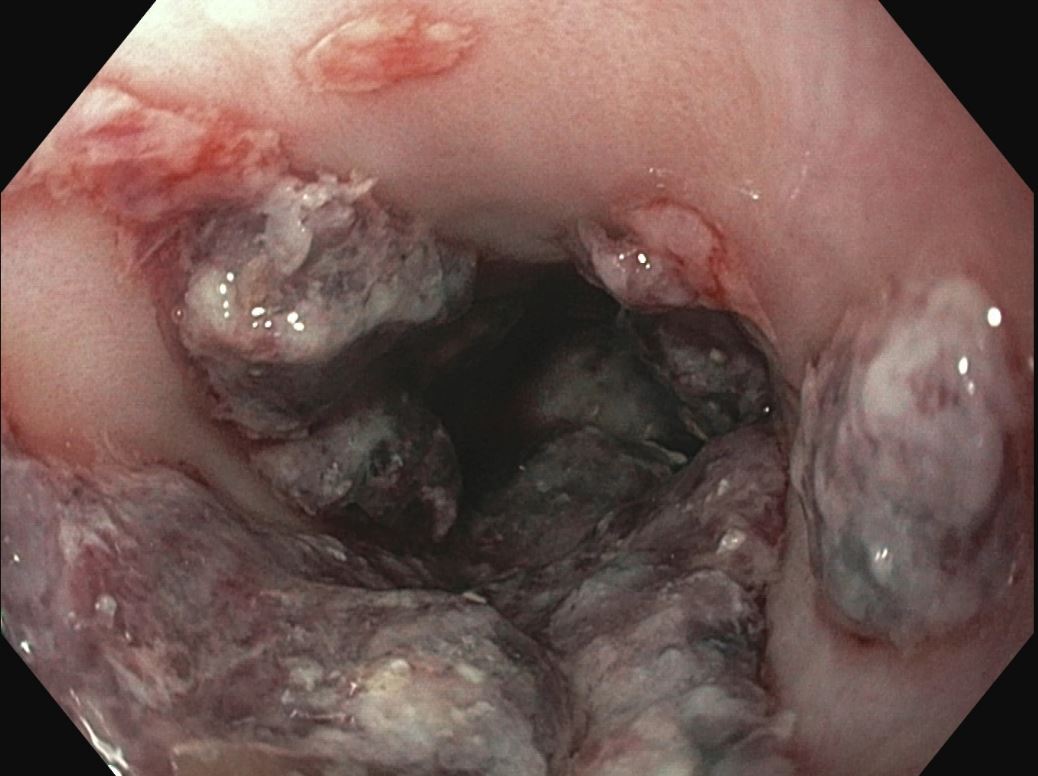
Figure: 1B
Disclosures:
Mark Baniqued indicated no relevant financial relationships.
Rhett Harmon indicated no relevant financial relationships.
Christina Sisliyan indicated no relevant financial relationships.
Soonwook Hong indicated no relevant financial relationships.
Daniel Cole indicated no relevant financial relationships.
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Christina Sisliyan, DO1, Soonwook Hong, MD2, Daniel Cole, MD, MPH1. P5036 - Unmasking the Uncommon: A Case Report of Esophagitis Caused by Herpes Simplex Virus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
