Tuesday Poster Session
Category: Esophagus
P5035 - A Rare Complication of a Rare Disease: Tracheoesophageal Fistula Formation in a Patient With Esophageal Squamous Papillomatosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Megan B. Ghai, MD, MPH, MA
University of Minnesota Medical School
Minneapolis, MN
Presenting Author(s)
Megan B.. Ghai, MD, MPH, MA1, Angelika Zalewski, MD1, Stephanie H. Rodriguez, MD2, Brian Hanson, MD3
1University of Minnesota Medical School, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Esophageal squamous papillomatosis (ESP) is a benign condition marked by multiple papillomas throughout the esophagus. Only 53 cases of ESP are documented in the English language literature. Proposed risk factors include mucosal irritation and infection with human papilloma virus. Clinical presentations vary from asymptomatic to severe dysphagia with stricture formation. Due to its rarity, there is limited understanding of its clinical progression and no established management guidelines. We report a rare case of tracheoesophageal fistula (TEF) formation in a patient with ESP.
Case Description/
Methods: A 70-year-old male with chronic dysphagia was diagnosed with ESP. Severe malnutrition precluded esophagectomy, thus the decision was made to attempt serial esophagogastroduodenoscopies (EGDs) for endoscopic spray cryotherapy and dilation every 7–10 days. Over 6 weeks, the patient showed marked symptomatic and endoscopic improvement. However, upon reducing treatment frequency to monthly, symptoms and strictures recurred.
After a routine follow-up EGD revealed recurrent ESP that was debulked using cold snare and endoscopic cap, the patient developed acute hypoxic respiratory failure. Computed tomography (CT) of the chest showed extravasation of contrast from the esophagus into the left bronchus consistent with a TEF (figure 1). There were no signs of free air or acute perforation. Repeat EGD confirmed the TEF, thought to have been previously occluded by ESP (figure 2a). After biopsies of the esophagus and TEF again revealed ESP without dysplasia or malignancy, a 22 mm by 150 mm fully covered metal esophageal stent was placed under fluoroscopic guidance. Follow-up CT imaging showed the stent in good position occluding the TEF and the patient was able to tolerate a soft diet.
Discussion: While ESP is characterized by the presence of multiple wart-like projections in the esophagus, the underlying mucosa is normal. Therefore, it is unclear what led to this transmural pathology. It is possible that repeated trauma from serial dilations and cryotherapy led to transmural inflammation and fistula formation, exacerbated by the patient’s malnourished state. While malignancy can result in TEF formation, this was ruled out with repeat esophageal biopsies and subsequent bronchoscopy. This case represents the first documented instance of ESP complicated by a TEF, contributing to the limited literature and raising questions about the natural history and potential risks of treatment-related trauma in this disease.
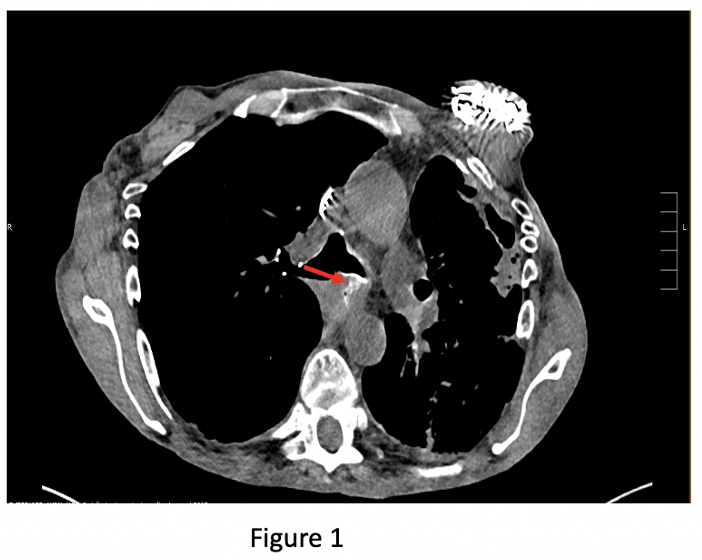
Figure: Figure 1: Computed tomography of the chest demonstrating extravasation of contrast from the esophageal lumen into the left bronchus (red arrow) concerning for the presence of a tracheoesophageal fistula.
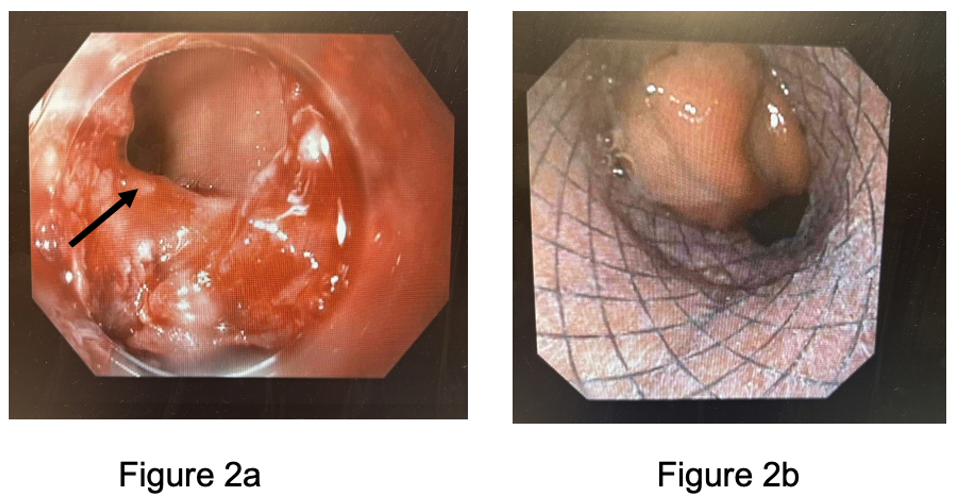
Figure: Figure 2a: Esophagogastroduodenoscopy image revealing the presence of a 10-millimeter mid-esophageal fistula communicating with the left bronchus (black arrow).
Figure 2b: Esophagogastroduodenoscopy image showing placement of a 22-millimeter by 150-millimeter covered stent over the tracheoesophageal fistula.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Angelika Zalewski indicated no relevant financial relationships.
Stephanie Rodriguez indicated no relevant financial relationships.
Brian Hanson indicated no relevant financial relationships.
Megan B.. Ghai, MD, MPH, MA1, Angelika Zalewski, MD1, Stephanie H. Rodriguez, MD2, Brian Hanson, MD3. P5035 - A Rare Complication of a Rare Disease: Tracheoesophageal Fistula Formation in a Patient With Esophageal Squamous Papillomatosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota Medical School, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Esophageal squamous papillomatosis (ESP) is a benign condition marked by multiple papillomas throughout the esophagus. Only 53 cases of ESP are documented in the English language literature. Proposed risk factors include mucosal irritation and infection with human papilloma virus. Clinical presentations vary from asymptomatic to severe dysphagia with stricture formation. Due to its rarity, there is limited understanding of its clinical progression and no established management guidelines. We report a rare case of tracheoesophageal fistula (TEF) formation in a patient with ESP.
Case Description/
Methods: A 70-year-old male with chronic dysphagia was diagnosed with ESP. Severe malnutrition precluded esophagectomy, thus the decision was made to attempt serial esophagogastroduodenoscopies (EGDs) for endoscopic spray cryotherapy and dilation every 7–10 days. Over 6 weeks, the patient showed marked symptomatic and endoscopic improvement. However, upon reducing treatment frequency to monthly, symptoms and strictures recurred.
After a routine follow-up EGD revealed recurrent ESP that was debulked using cold snare and endoscopic cap, the patient developed acute hypoxic respiratory failure. Computed tomography (CT) of the chest showed extravasation of contrast from the esophagus into the left bronchus consistent with a TEF (figure 1). There were no signs of free air or acute perforation. Repeat EGD confirmed the TEF, thought to have been previously occluded by ESP (figure 2a). After biopsies of the esophagus and TEF again revealed ESP without dysplasia or malignancy, a 22 mm by 150 mm fully covered metal esophageal stent was placed under fluoroscopic guidance. Follow-up CT imaging showed the stent in good position occluding the TEF and the patient was able to tolerate a soft diet.
Discussion: While ESP is characterized by the presence of multiple wart-like projections in the esophagus, the underlying mucosa is normal. Therefore, it is unclear what led to this transmural pathology. It is possible that repeated trauma from serial dilations and cryotherapy led to transmural inflammation and fistula formation, exacerbated by the patient’s malnourished state. While malignancy can result in TEF formation, this was ruled out with repeat esophageal biopsies and subsequent bronchoscopy. This case represents the first documented instance of ESP complicated by a TEF, contributing to the limited literature and raising questions about the natural history and potential risks of treatment-related trauma in this disease.
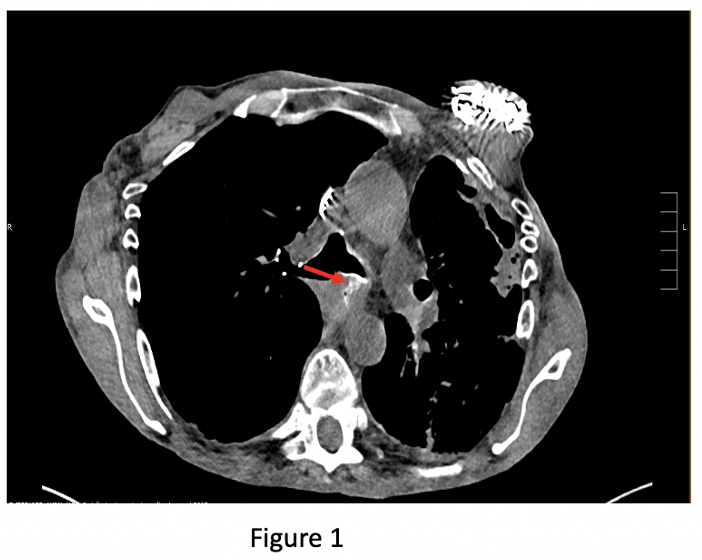
Figure: Figure 1: Computed tomography of the chest demonstrating extravasation of contrast from the esophageal lumen into the left bronchus (red arrow) concerning for the presence of a tracheoesophageal fistula.
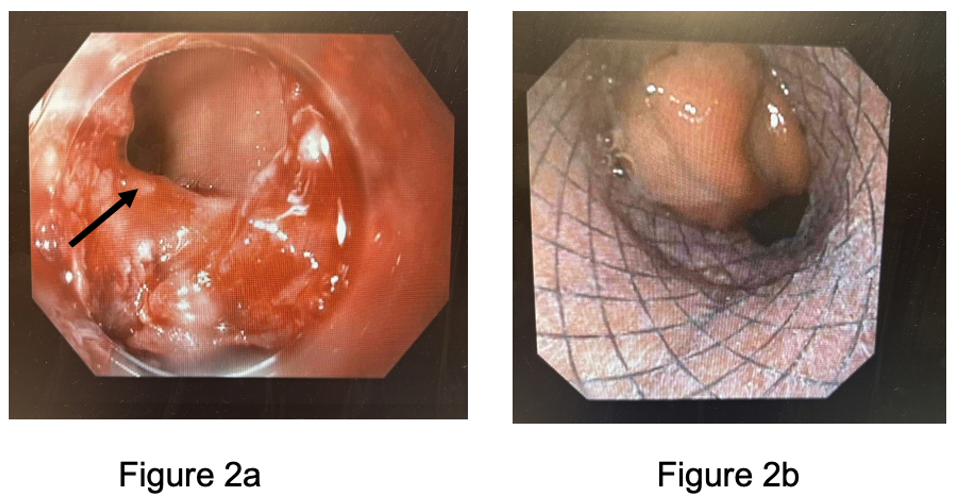
Figure: Figure 2a: Esophagogastroduodenoscopy image revealing the presence of a 10-millimeter mid-esophageal fistula communicating with the left bronchus (black arrow).
Figure 2b: Esophagogastroduodenoscopy image showing placement of a 22-millimeter by 150-millimeter covered stent over the tracheoesophageal fistula.
Disclosures:
Megan Ghai indicated no relevant financial relationships.
Angelika Zalewski indicated no relevant financial relationships.
Stephanie Rodriguez indicated no relevant financial relationships.
Brian Hanson indicated no relevant financial relationships.
Megan B.. Ghai, MD, MPH, MA1, Angelika Zalewski, MD1, Stephanie H. Rodriguez, MD2, Brian Hanson, MD3. P5035 - A Rare Complication of a Rare Disease: Tracheoesophageal Fistula Formation in a Patient With Esophageal Squamous Papillomatosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
