Tuesday Poster Session
Category: Esophagus
P5034 - Radiation-Induced Esophageal Stricture: An Unconventional Approach to a Common Side Effect
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Shehadah, MD (he/him/his)
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
Ahmed Shehadah, MD1, Fawad Talat, MD1, AbdulSubhan Talpur, MD1, Usama Sakhawat, MD2, Khandokar Talib, MD3, Gowthami Ramar, MD1, Alshaima Yousef, MD4, Amanke Oranu, MD1, Toseef Javaid, MD2
1United Health Services, Wilson Medical Center, Binghamton, NY; 2United Health Services, Wilson Medical Center, Johnson City, NY; 3United Health Services, Johnson City, NY; 4Rochester General Hospital, Rochester, NY
Introduction: Radiation-induced esophageal stricture (RIES) is a common problem encountered by patients who undergo radiation therapy for a variety of oncological malignancies. 5-20 % of patients who undergo head/neck and thoracic radiation develop RIES. We describe an unconventional approach for management of dysphagia in a patient with RIES.
Case Description/
Methods: 79-year-old male with history of invasive keratinizing squamous cell carcinoma of vocal cord, history of preemptive PEG tube placement prior to chemotherapy and radiotherapy, who presented to the GI office 6 months after starting chemotherapy and radiotherapy with an inability to tolerate secretions along with frequent coughing. An upper endoscopy was attempted to delineate the cause of dysphagia, but no esophageal lumen could be visualized. Upper endoscopy was then reattempted under anesthesia and fluoroscopic guidance.
Multiple attempts were made to advance the gastroscope into the esophageal lumen, but all attempts were unsuccessful. Pediatric gastroscope was also used but could not be advanced as there was complete occlusion of esophageal lumen at upper esophageal sphincter due to fibrotic membrane secondary to radiation therapy. An alternative approach was then used. The pediatric gastroscope was advanced through the G-tube lumen into the stomach. From the stomach, it was advanced in retrograde fashion under fluoroscopic guidance into the esophagus up to the level of upper esophageal sphincter. A 450 cm x 0.035 inch guidewire was then advanced through the pediatric gastroscope. The sharp end of the guidewire was used to puncture the membrane that was occluding the upper esophageal sphincter. Following that, adult gastroscope was advanced through the patient's mouth, and the guidewire was grasped. Under fluoroscopic guidance, the esophagus was serially dilated over the guidewire up to 10 mm using savory dilator. The patient tolerated the procedure well. Following recovery, patient was able to tolerate a mechanically soft diet.
Discussion: RIES is a frequently encountered problem that necessitates thorough evaluation on a case-by-case basis to guide appropriate management. In our patient, our approach was to access the G-tube lumen and enter esophagus in a retrograde fashion and use a guidewire's sharp end to obtain adequate positioning under fluoroscopy for safe dilation to take place. Further research is needed to determine the safety and efficacy of this approach.
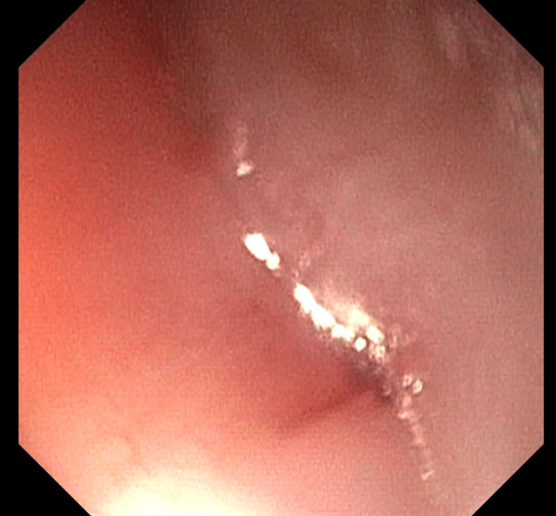
Figure: Stenosed upper esophageal stricture due to RIES
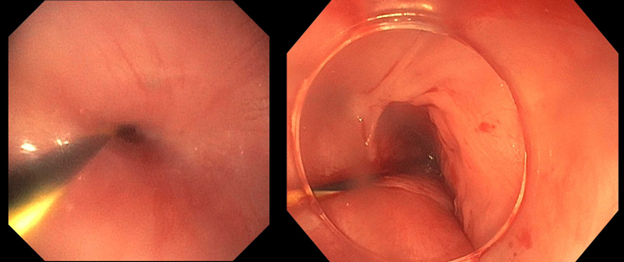
Figure: Left image showing retrograde endoscopic view of upper esophageal stenosis through G-Tube using pediatric gastroscope.
Right image showing moderate mucosal disruption at upper esophageal sphincter post dilation.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Fawad Talat, MD1, AbdulSubhan Talpur, MD1, Usama Sakhawat, MD2, Khandokar Talib, MD3, Gowthami Ramar, MD1, Alshaima Yousef, MD4, Amanke Oranu, MD1, Toseef Javaid, MD2. P5034 - Radiation-Induced Esophageal Stricture: An Unconventional Approach to a Common Side Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Binghamton, NY; 2United Health Services, Wilson Medical Center, Johnson City, NY; 3United Health Services, Johnson City, NY; 4Rochester General Hospital, Rochester, NY
Introduction: Radiation-induced esophageal stricture (RIES) is a common problem encountered by patients who undergo radiation therapy for a variety of oncological malignancies. 5-20 % of patients who undergo head/neck and thoracic radiation develop RIES. We describe an unconventional approach for management of dysphagia in a patient with RIES.
Case Description/
Methods: 79-year-old male with history of invasive keratinizing squamous cell carcinoma of vocal cord, history of preemptive PEG tube placement prior to chemotherapy and radiotherapy, who presented to the GI office 6 months after starting chemotherapy and radiotherapy with an inability to tolerate secretions along with frequent coughing. An upper endoscopy was attempted to delineate the cause of dysphagia, but no esophageal lumen could be visualized. Upper endoscopy was then reattempted under anesthesia and fluoroscopic guidance.
Multiple attempts were made to advance the gastroscope into the esophageal lumen, but all attempts were unsuccessful. Pediatric gastroscope was also used but could not be advanced as there was complete occlusion of esophageal lumen at upper esophageal sphincter due to fibrotic membrane secondary to radiation therapy. An alternative approach was then used. The pediatric gastroscope was advanced through the G-tube lumen into the stomach. From the stomach, it was advanced in retrograde fashion under fluoroscopic guidance into the esophagus up to the level of upper esophageal sphincter. A 450 cm x 0.035 inch guidewire was then advanced through the pediatric gastroscope. The sharp end of the guidewire was used to puncture the membrane that was occluding the upper esophageal sphincter. Following that, adult gastroscope was advanced through the patient's mouth, and the guidewire was grasped. Under fluoroscopic guidance, the esophagus was serially dilated over the guidewire up to 10 mm using savory dilator. The patient tolerated the procedure well. Following recovery, patient was able to tolerate a mechanically soft diet.
Discussion: RIES is a frequently encountered problem that necessitates thorough evaluation on a case-by-case basis to guide appropriate management. In our patient, our approach was to access the G-tube lumen and enter esophagus in a retrograde fashion and use a guidewire's sharp end to obtain adequate positioning under fluoroscopy for safe dilation to take place. Further research is needed to determine the safety and efficacy of this approach.
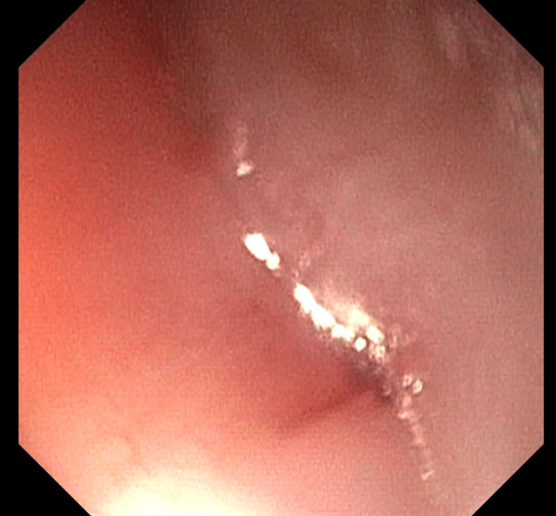
Figure: Stenosed upper esophageal stricture due to RIES
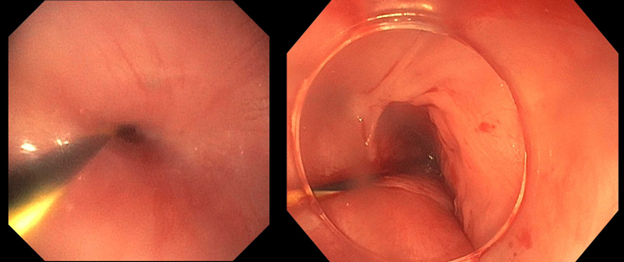
Figure: Left image showing retrograde endoscopic view of upper esophageal stenosis through G-Tube using pediatric gastroscope.
Right image showing moderate mucosal disruption at upper esophageal sphincter post dilation.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Fawad Talat indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Gowthami Ramar indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Fawad Talat, MD1, AbdulSubhan Talpur, MD1, Usama Sakhawat, MD2, Khandokar Talib, MD3, Gowthami Ramar, MD1, Alshaima Yousef, MD4, Amanke Oranu, MD1, Toseef Javaid, MD2. P5034 - Radiation-Induced Esophageal Stricture: An Unconventional Approach to a Common Side Effect, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
