Tuesday Poster Session
Category: Esophagus
P5033 - Pan-Esophageal Intramural Hematoma: A Rare Complication of Food Impaction in Esophageal Scleroderma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Shehadah, MD (he/him/his)
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Moheudin Khan, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Amanke Oranu, MD1, Toseef Javaid, MD3
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY
Introduction: Esophageal intramural hematoma (EIH) is a rare, potentially life-threatening condition, often associated with anticoagulant therapy. This case highlights a unique presentation and a novel management approach of a severe EIH in a patient with scleroderma presenting with food impaction and hematemesis. EIH in a scleroderma patient and its management using stent in stent technique has not been previously reported in the literature.
Case Description/
Methods: A 71-year-old female with a history of scleroderma, coronary artery disease on aspirin, and pulmonary embolism on rivaroxaban presented with inability to tolerate secretions and hematemesis. Computed tomography (CT) neck and chest showed diffuse intramural esophageal hematoma with a non visible esophageal lumen (EL). The esophagus measured 4 × 3 cm in the upper thoracic and 5 × 4 cm in the lower thoracic region.
Esophagogastroduodenoscopy (EGD) was done under general anesthesia and revealed complete occlusion of the EL caused by a large EIH beginning 2 cm below the upper esophageal sphincter. The EIH compressed the EL, caused mucosal disruption with active bleeding, and posed a significant risk of perforation. A therapeutic gastroscope was advanced carefully to the gastroesophageal junction, where food material was identified. A fully covered 18 mm × 97 mm self-expanding metallic stent was placed under fluoroscopic guidance, and positioned at the upper level of bleeding. Due to the extensive EIH, the EL remained occluded after the first stent placement. Consequently, a second stent was deployed using the stent-in-stent technique. Successful tamponade was achieved, and secretions appropriately drained.
The patient’s diet was gradually advanced the following days and was discharged. Repeat EGD 2 weeks later confirmed proper stent positioning and complete resolution of the previously noted EIH. Both stents were successfully removed under fluoroscopic guidance, revealing a patent EL demonstrating clinical success.
Discussion: This case highlights a rare presentation of severe panesophageal EIH in a patient with scleroderma on anticoagulant therapy, a condition not previously reported. Due to the high risk of perforation and inability to tolerate secretions a novel stent-in-stent endoscopic technique was successfully employed, achieving tamponade and resolving the obstruction. Further studies are needed to demonstrate the safety and efficacy of stent-in-stent technique for EIH.

Figure: CT Imaging Demonstrating Extensive Esophageal Intramural Hematoma in a Cross Section and Coronal View
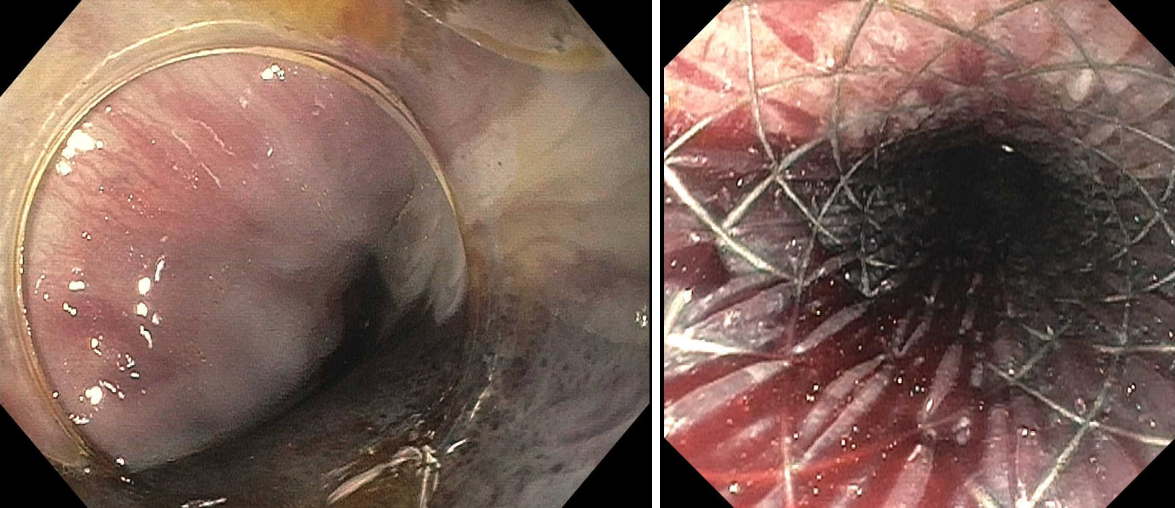
Figure: Endoscopic View Demonstrating Stent in Stent Technique with Expansion of Esophageal Lumen
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Moheudin Khan, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Amanke Oranu, MD1, Toseef Javaid, MD3. P5033 - Pan-Esophageal Intramural Hematoma: A Rare Complication of Food Impaction in Esophageal Scleroderma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Moheudin Khan, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Amanke Oranu, MD1, Toseef Javaid, MD3
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY
Introduction: Esophageal intramural hematoma (EIH) is a rare, potentially life-threatening condition, often associated with anticoagulant therapy. This case highlights a unique presentation and a novel management approach of a severe EIH in a patient with scleroderma presenting with food impaction and hematemesis. EIH in a scleroderma patient and its management using stent in stent technique has not been previously reported in the literature.
Case Description/
Methods: A 71-year-old female with a history of scleroderma, coronary artery disease on aspirin, and pulmonary embolism on rivaroxaban presented with inability to tolerate secretions and hematemesis. Computed tomography (CT) neck and chest showed diffuse intramural esophageal hematoma with a non visible esophageal lumen (EL). The esophagus measured 4 × 3 cm in the upper thoracic and 5 × 4 cm in the lower thoracic region.
Esophagogastroduodenoscopy (EGD) was done under general anesthesia and revealed complete occlusion of the EL caused by a large EIH beginning 2 cm below the upper esophageal sphincter. The EIH compressed the EL, caused mucosal disruption with active bleeding, and posed a significant risk of perforation. A therapeutic gastroscope was advanced carefully to the gastroesophageal junction, where food material was identified. A fully covered 18 mm × 97 mm self-expanding metallic stent was placed under fluoroscopic guidance, and positioned at the upper level of bleeding. Due to the extensive EIH, the EL remained occluded after the first stent placement. Consequently, a second stent was deployed using the stent-in-stent technique. Successful tamponade was achieved, and secretions appropriately drained.
The patient’s diet was gradually advanced the following days and was discharged. Repeat EGD 2 weeks later confirmed proper stent positioning and complete resolution of the previously noted EIH. Both stents were successfully removed under fluoroscopic guidance, revealing a patent EL demonstrating clinical success.
Discussion: This case highlights a rare presentation of severe panesophageal EIH in a patient with scleroderma on anticoagulant therapy, a condition not previously reported. Due to the high risk of perforation and inability to tolerate secretions a novel stent-in-stent endoscopic technique was successfully employed, achieving tamponade and resolving the obstruction. Further studies are needed to demonstrate the safety and efficacy of stent-in-stent technique for EIH.

Figure: CT Imaging Demonstrating Extensive Esophageal Intramural Hematoma in a Cross Section and Coronal View
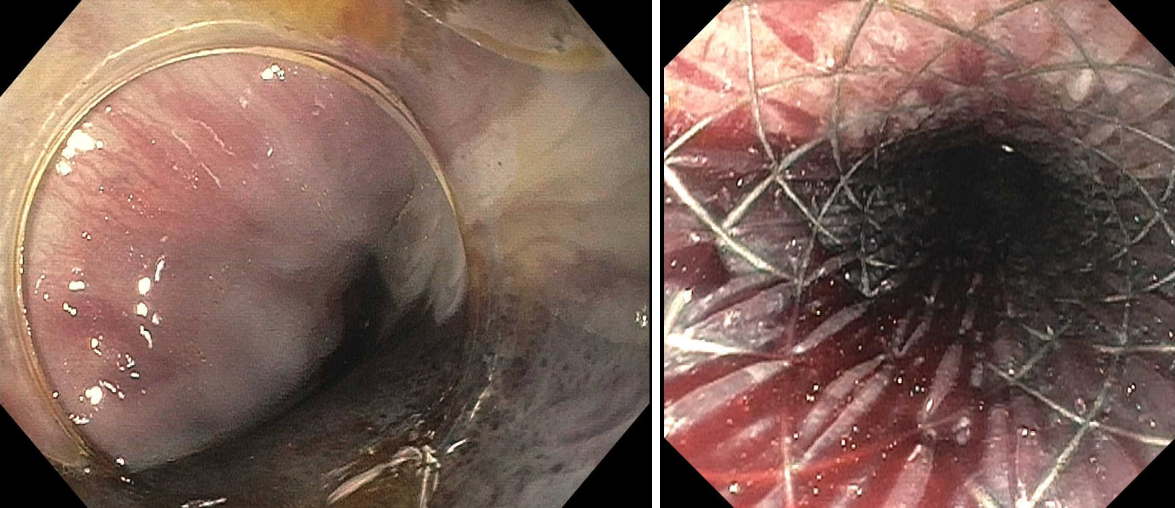
Figure: Endoscopic View Demonstrating Stent in Stent Technique with Expansion of Esophageal Lumen
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Moheudin Khan indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Amanke Oranu indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Khandokar Talib, MD4, Moheudin Khan, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Amanke Oranu, MD1, Toseef Javaid, MD3. P5033 - Pan-Esophageal Intramural Hematoma: A Rare Complication of Food Impaction in Esophageal Scleroderma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

