Tuesday Poster Session
Category: General Endoscopy
P5114 - Development and Validation of a Simplified Tool to Predict Endoscopist-Rated Utility of Tattoo Placement for Colorectal Polyp Localization
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Natalie J. Wilson, MD (she/her/hers)
University of Minnesota
Chapel Hill, NC
Presenting Author(s)
Award: ACG Presidential Poster Award
Natalie J. Wilson, MD1, Hassam Ali, MD2, Rahul Karna, MD3, Mohanad Awadalla, MD4, Frances Dang, MD, MSc5, Ronald C. Turner, MD6, Roya Dastjerdi, MPH4, Markus Goldschmiedt, MD6, John G. Lee, MD7, Douglas Pleskow, MD4, Tyler M. Berzin, MD4, Shawn L. Shah, MD6, Thomas Tielleman, MD6, Jason Samarasena, MD, MBA, FACG8, Moamen Gabr, MD9, Mohammad Bilal, MD, FACG10
1University of Minnesota, Minneapolis, MN; 2East Carolina University/Brody School of Medicine, Greenville, NC; 3University of Minnesota Medical Center, Minneapolis, MN; 4Beth Israel Deaconess Medical Center, Boston, MA; 5University of California Irvine, Irvine, CA; 6University of Texas Southwestern Medical Center, Dallas, TX; 7UC Irvine Digestive Health Institute, Orange, CA; 8University of California Irvine, Orange, CA; 9University of Cincinnati College of Medicine, Cincinnati, OH; 10University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Tattoo placement is recommended for large colorectal polyps (CRPs) referred for endoscopic resection (ER). However, it is unclear whether endoscopists performing ER find tattoo placement helpful. We aimed to develop a clinical model to predict endoscopist-rated tattoo usefulness based on prospectively collected data.
Methods: This was a prospective, multicenter study. Adults referred for ER of a previously tattooed CRP were enrolled at 7 sites from February 2024 to December 2024. After ER, endoscopists completed a 7-item, 5-point Likert survey evaluating tattoo usefulness.
The prediction model was developed using Least Absolute Shrinkage and Selection Operator (LASSO) logistic regression with 5-fold cross-validation to select from >50 variables. A simplified logistic regression model was constructed using the most predictive clinical variables. Model discrimination was assessed using cross-validated and bootstrapped area under the curve (AUCs). Calibration was evaluated using the GiViTI calibration belt.
Results: A total of 103 CRPs from 101 patients were tattooed and referred for ER. Tattoo placement was rated as helpful in 43% (44/103). Patient and polyp details are outlined in Table 1A and survey responses in 1B.
LASSO logistic regression identified 7 key predictors and demonstrated strong discrimination (cross-validated AUC 0.88; 95% CI, 0.77–0.94) but poor calibration (GiViTI p=0.003). A simplified multivariable logistic regression model was constructed using LASSO-selected variables. The final model included the following variables: colonoscopy indication, polyp size, location, ileocecal valve involvement, polyp fibrosis/scarring, morphology, and suspected histology. The model demonstrated excellent performance (AUC 0.83; bootstrap 95% CI, 0.77–0.93) with good calibration (GiViTI p=0.124) [Figure 1A]. Using an optimal probability threshold (≥0.467), the model achieved 80% sensitivity, 78% specificity, 71.4% PPV, 83% NPV, and 77.5% overall accuracy.
To facilitate clinical implementation, a web-based calculator (https://bit.ly/PolypTattoo) that predicts the probability of tattoo usefulness was created using variables from the final prediction model [Figure 1B].
Discussion: Using prospectively collected data, we developed a 7-variable model using routinely available colonoscopy data that can accurately predict when tattoo placement will be helpful for lesion localization for future ER. The model demonstrated excellent performance, though external validation is needed.
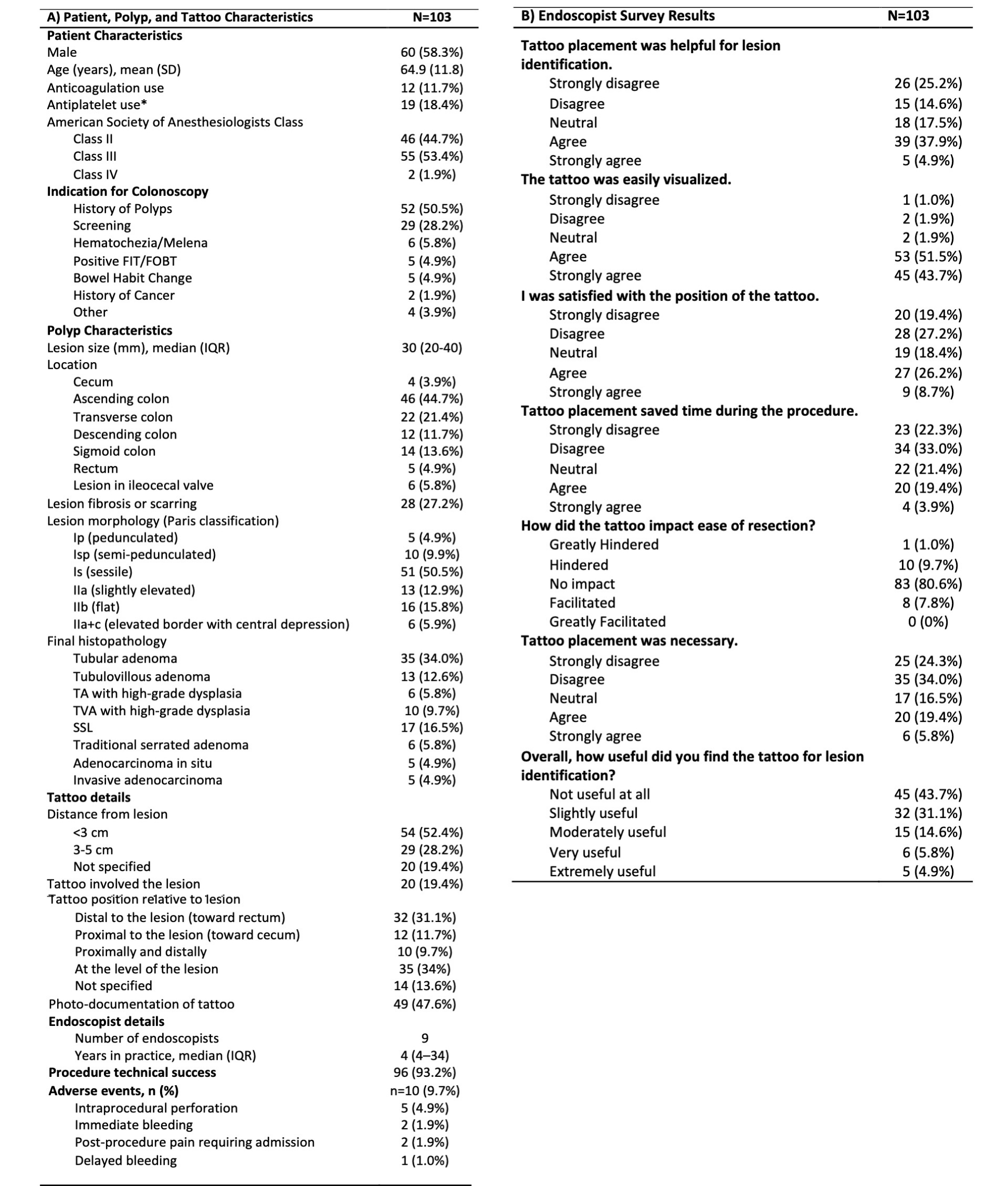
Figure: Table 1. Patient, Polyp, and Tattoo Characteristics (A) and Endoscopist Survey Responses Evaluating the Utility of Tattoo Placement for Lesion Identification (B)
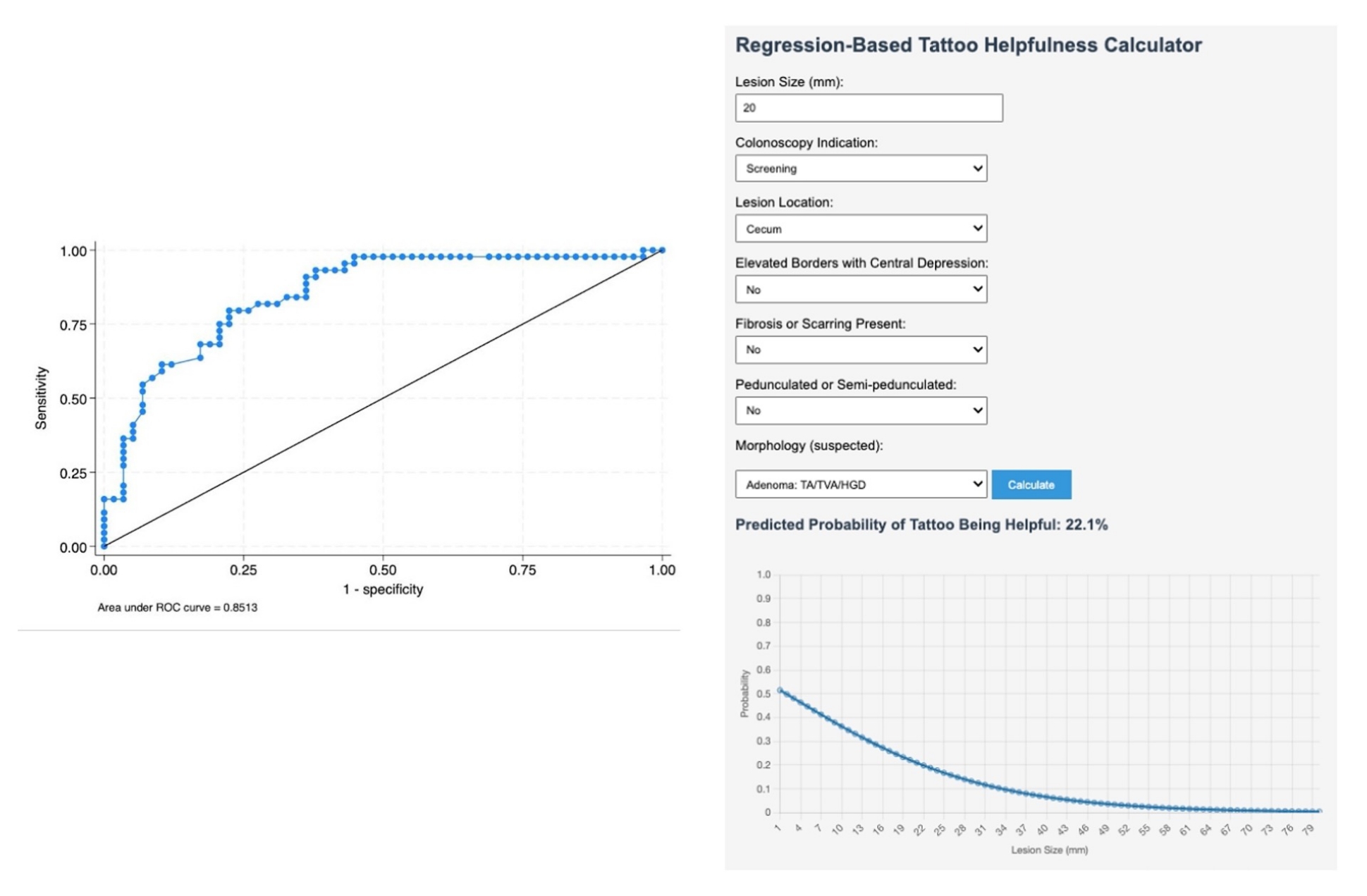
Figure: Figure 1. A (left): Receiver operating curve of the final prediction model demonstrates an area under the curve (AUC) of 0.83 (bootstrap 95% CI: 0.77–0.93). B (right): Web-based calculator estimating the usefulness of tattoo placement for colorectal polyps referred for endoscopic resection developed from the final prediction model. The calculator can be accessed at https://bit.ly/PolypTattoo
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Ronald Turner indicated no relevant financial relationships.
Roya Dastjerdi indicated no relevant financial relationships.
Markus Goldschmiedt indicated no relevant financial relationships.
John Lee indicated no relevant financial relationships.
Douglas Pleskow indicated no relevant financial relationships.
Tyler Berzin: Boston Scientific – Consultant. Medtronic – Consultant. Wision AI – Consultant.
Shawn Shah indicated no relevant financial relationships.
Thomas Tielleman: ConMed – Consultant.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Moamen Gabr indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Natalie J. Wilson, MD1, Hassam Ali, MD2, Rahul Karna, MD3, Mohanad Awadalla, MD4, Frances Dang, MD, MSc5, Ronald C. Turner, MD6, Roya Dastjerdi, MPH4, Markus Goldschmiedt, MD6, John G. Lee, MD7, Douglas Pleskow, MD4, Tyler M. Berzin, MD4, Shawn L. Shah, MD6, Thomas Tielleman, MD6, Jason Samarasena, MD, MBA, FACG8, Moamen Gabr, MD9, Mohammad Bilal, MD, FACG10. P5114 - Development and Validation of a Simplified Tool to Predict Endoscopist-Rated Utility of Tattoo Placement for Colorectal Polyp Localization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Natalie J. Wilson, MD1, Hassam Ali, MD2, Rahul Karna, MD3, Mohanad Awadalla, MD4, Frances Dang, MD, MSc5, Ronald C. Turner, MD6, Roya Dastjerdi, MPH4, Markus Goldschmiedt, MD6, John G. Lee, MD7, Douglas Pleskow, MD4, Tyler M. Berzin, MD4, Shawn L. Shah, MD6, Thomas Tielleman, MD6, Jason Samarasena, MD, MBA, FACG8, Moamen Gabr, MD9, Mohammad Bilal, MD, FACG10
1University of Minnesota, Minneapolis, MN; 2East Carolina University/Brody School of Medicine, Greenville, NC; 3University of Minnesota Medical Center, Minneapolis, MN; 4Beth Israel Deaconess Medical Center, Boston, MA; 5University of California Irvine, Irvine, CA; 6University of Texas Southwestern Medical Center, Dallas, TX; 7UC Irvine Digestive Health Institute, Orange, CA; 8University of California Irvine, Orange, CA; 9University of Cincinnati College of Medicine, Cincinnati, OH; 10University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Tattoo placement is recommended for large colorectal polyps (CRPs) referred for endoscopic resection (ER). However, it is unclear whether endoscopists performing ER find tattoo placement helpful. We aimed to develop a clinical model to predict endoscopist-rated tattoo usefulness based on prospectively collected data.
Methods: This was a prospective, multicenter study. Adults referred for ER of a previously tattooed CRP were enrolled at 7 sites from February 2024 to December 2024. After ER, endoscopists completed a 7-item, 5-point Likert survey evaluating tattoo usefulness.
The prediction model was developed using Least Absolute Shrinkage and Selection Operator (LASSO) logistic regression with 5-fold cross-validation to select from >50 variables. A simplified logistic regression model was constructed using the most predictive clinical variables. Model discrimination was assessed using cross-validated and bootstrapped area under the curve (AUCs). Calibration was evaluated using the GiViTI calibration belt.
Results: A total of 103 CRPs from 101 patients were tattooed and referred for ER. Tattoo placement was rated as helpful in 43% (44/103). Patient and polyp details are outlined in Table 1A and survey responses in 1B.
LASSO logistic regression identified 7 key predictors and demonstrated strong discrimination (cross-validated AUC 0.88; 95% CI, 0.77–0.94) but poor calibration (GiViTI p=0.003). A simplified multivariable logistic regression model was constructed using LASSO-selected variables. The final model included the following variables: colonoscopy indication, polyp size, location, ileocecal valve involvement, polyp fibrosis/scarring, morphology, and suspected histology. The model demonstrated excellent performance (AUC 0.83; bootstrap 95% CI, 0.77–0.93) with good calibration (GiViTI p=0.124) [Figure 1A]. Using an optimal probability threshold (≥0.467), the model achieved 80% sensitivity, 78% specificity, 71.4% PPV, 83% NPV, and 77.5% overall accuracy.
To facilitate clinical implementation, a web-based calculator (https://bit.ly/PolypTattoo) that predicts the probability of tattoo usefulness was created using variables from the final prediction model [Figure 1B].
Discussion: Using prospectively collected data, we developed a 7-variable model using routinely available colonoscopy data that can accurately predict when tattoo placement will be helpful for lesion localization for future ER. The model demonstrated excellent performance, though external validation is needed.
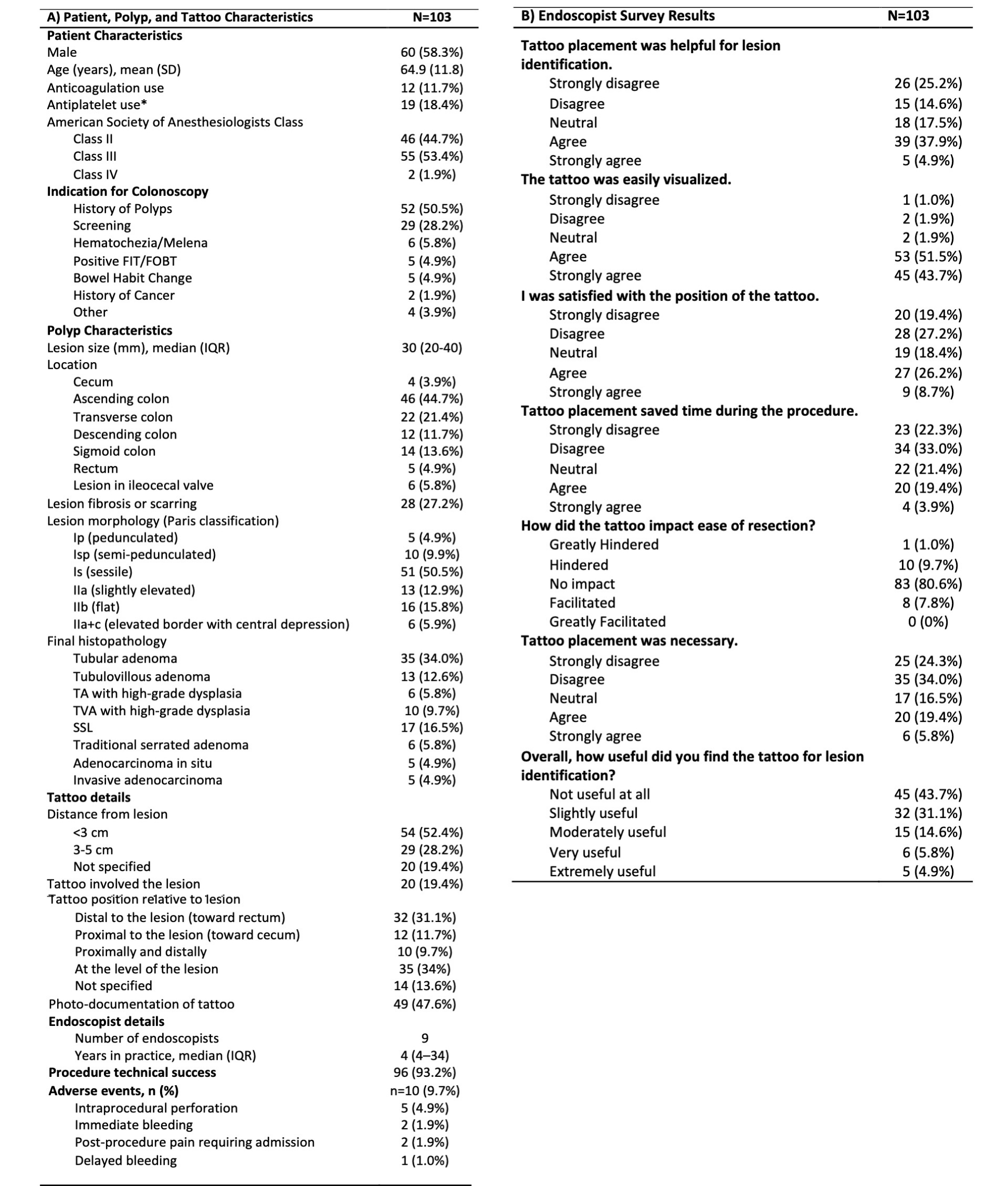
Figure: Table 1. Patient, Polyp, and Tattoo Characteristics (A) and Endoscopist Survey Responses Evaluating the Utility of Tattoo Placement for Lesion Identification (B)
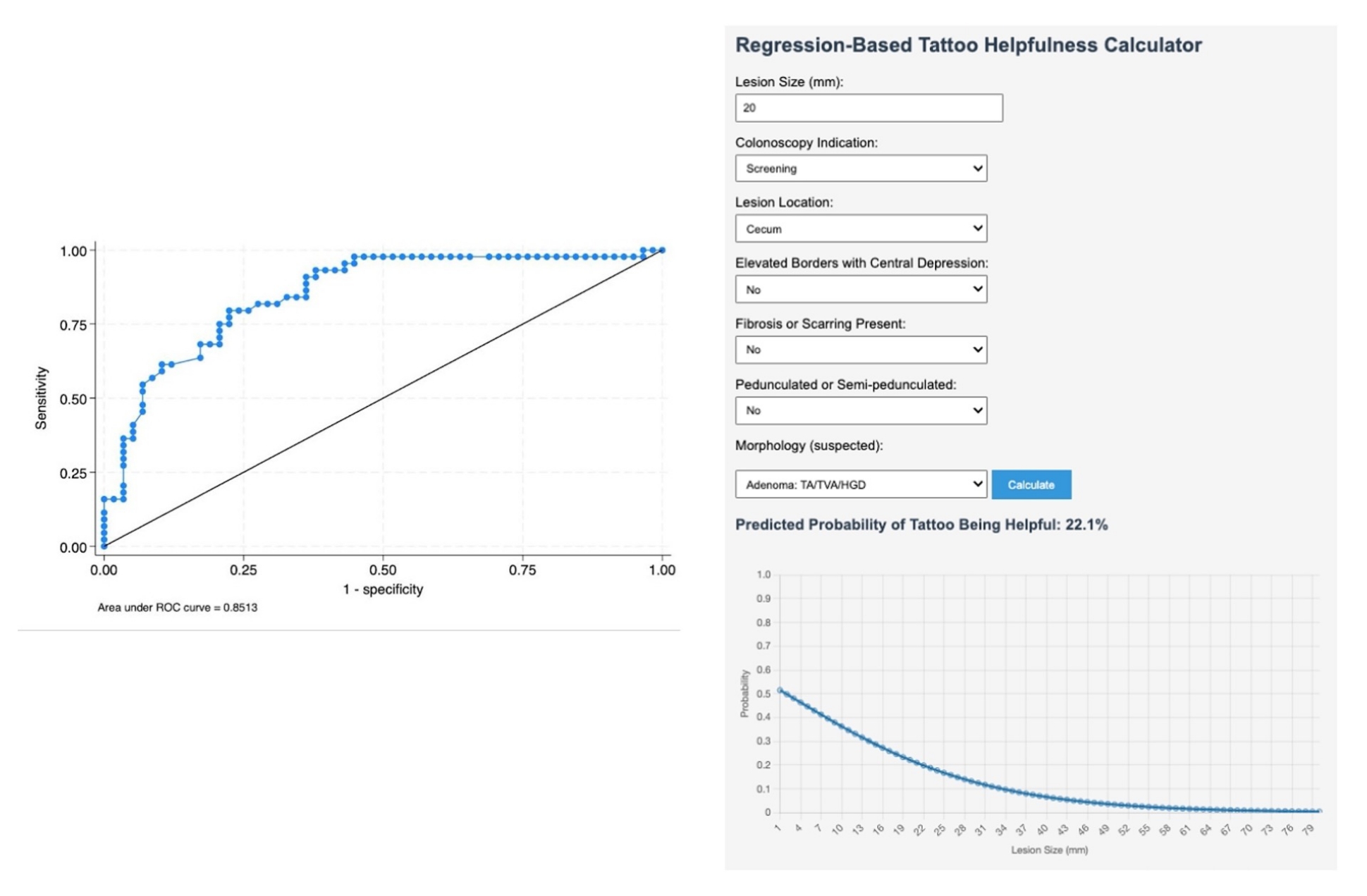
Figure: Figure 1. A (left): Receiver operating curve of the final prediction model demonstrates an area under the curve (AUC) of 0.83 (bootstrap 95% CI: 0.77–0.93). B (right): Web-based calculator estimating the usefulness of tattoo placement for colorectal polyps referred for endoscopic resection developed from the final prediction model. The calculator can be accessed at https://bit.ly/PolypTattoo
Disclosures:
Natalie Wilson indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohanad Awadalla indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Ronald Turner indicated no relevant financial relationships.
Roya Dastjerdi indicated no relevant financial relationships.
Markus Goldschmiedt indicated no relevant financial relationships.
John Lee indicated no relevant financial relationships.
Douglas Pleskow indicated no relevant financial relationships.
Tyler Berzin: Boston Scientific – Consultant. Medtronic – Consultant. Wision AI – Consultant.
Shawn Shah indicated no relevant financial relationships.
Thomas Tielleman: ConMed – Consultant.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Moamen Gabr indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Natalie J. Wilson, MD1, Hassam Ali, MD2, Rahul Karna, MD3, Mohanad Awadalla, MD4, Frances Dang, MD, MSc5, Ronald C. Turner, MD6, Roya Dastjerdi, MPH4, Markus Goldschmiedt, MD6, John G. Lee, MD7, Douglas Pleskow, MD4, Tyler M. Berzin, MD4, Shawn L. Shah, MD6, Thomas Tielleman, MD6, Jason Samarasena, MD, MBA, FACG8, Moamen Gabr, MD9, Mohammad Bilal, MD, FACG10. P5114 - Development and Validation of a Simplified Tool to Predict Endoscopist-Rated Utility of Tattoo Placement for Colorectal Polyp Localization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

