Tuesday Poster Session
Category: GI Bleeding
P5184 - Are DOACs Driving GI Bleeding Deaths? Population Trends vs Patient-Level Risk
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Haris Latif, MD (he/him/his)
SSM St Mary's Hospital
St. Louis, MO
Presenting Author(s)
Muhammad Haris Latif, MD1, Kahee A. Mohammed, MD1, Eman Mazhar, MBBS2, Zoha Noor, MBBS3, Kamran Qureshi, MD4
1SSM St Mary's Hospital, St. Louis, MO; 2Nishtar Medical University, St. Louis, FL; 3Sialkot medical college, Orlando, FL; 4Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Direct oral anticoagulants (DOACs) have largely replaced warfarin in clinical practice due to their convenience and favorable safety profile. However, gastrointestinal (GI) bleeding remains a key complication. This study investigates the impact of DOAC adoption on GI bleeding-related mortality at the population level in the United States. It examines per-user fatality trends to clarify risk over time.
Methods: We conducted a retrospective, observational interrupted time series (ITS) study using CDC WONDER Multiple Cause of Death data (2010–2020). GI bleeding deaths were identified by ICD-10 codes and limited to cases with atrial fibrillation, pulmonary embolism, or deep vein thrombosis listed as underlying or contributing causes—surrogate markers for anticoagulant exposure. Annual oral anticoagulant utilization was estimated using CMS Medicare Part D data and published prevalence studies. GI bleeding mortality was assessed both at the population level (age-adjusted rates per 100,000) and per 100,000 estimated DOAC users. Exposure-adjusted mortality per 100,000 DOAC users was analyzed from 2010 onward, the first year with measurable DOAC use. An ITS regression model assessed changes in mortality trends pre- and post-DOAC adoption (2014 defined as the intervention point).
Results: From 2010 to 2020, age-adjusted GI bleeding mortality rose from 0.6 to 1.3 per 100,000. DOAC use increased from 0% to 72% of oral anticoagulant prescriptions during this period. Despite the population-wide rise in mortality, GI bleeding deaths per 100,000 estimated DOAC users declined sharply, from 245.4 in 2010 to 20.0 in 2020. Segmented regression showed a significant pre-DOAC upward trend (β = 0.0321, p = 0.047), a non-significant immediate drop in 2014 (β = –0.296, p = 0.082), and a non-significant slope change post-DOAC (β = 0.0357, p = 0.106).
Discussion: While overall GI bleeding mortality has increased, exposure-adjusted analysis reveals a substantial decline in fatal GI bleeding rates among DOAC users over time. These findings suggest that the per-user risk of fatal GI bleeding has decreased, potentially due to improved prescribing, better risk stratification, and enhanced management. Population-wide trends may reflect other factors, including aging demographics and broader anticoagulant use. Exposure-adjusted metrics are essential for accurate risk assessment in real-world pharmacovigilance.
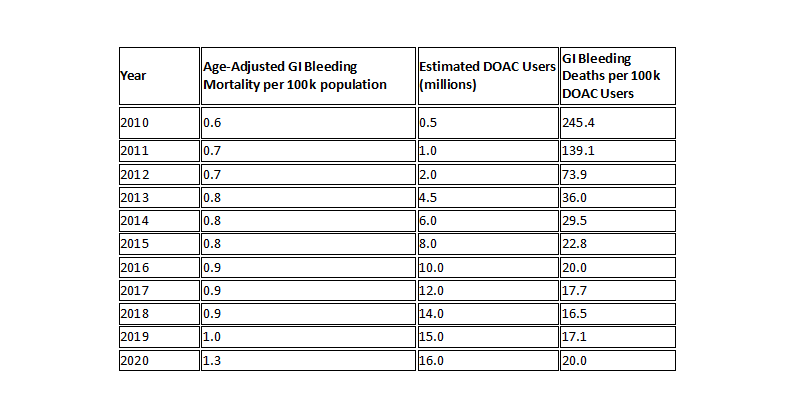
Figure: Trends in GI bleeding mortality, 2010–2020: While age-adjusted population-level mortality increased (blue), GI bleeding deaths per 100,000 DOAC users decreased significantly (red). The dashed line indicates the year of widespread DOAC adoption (2014).
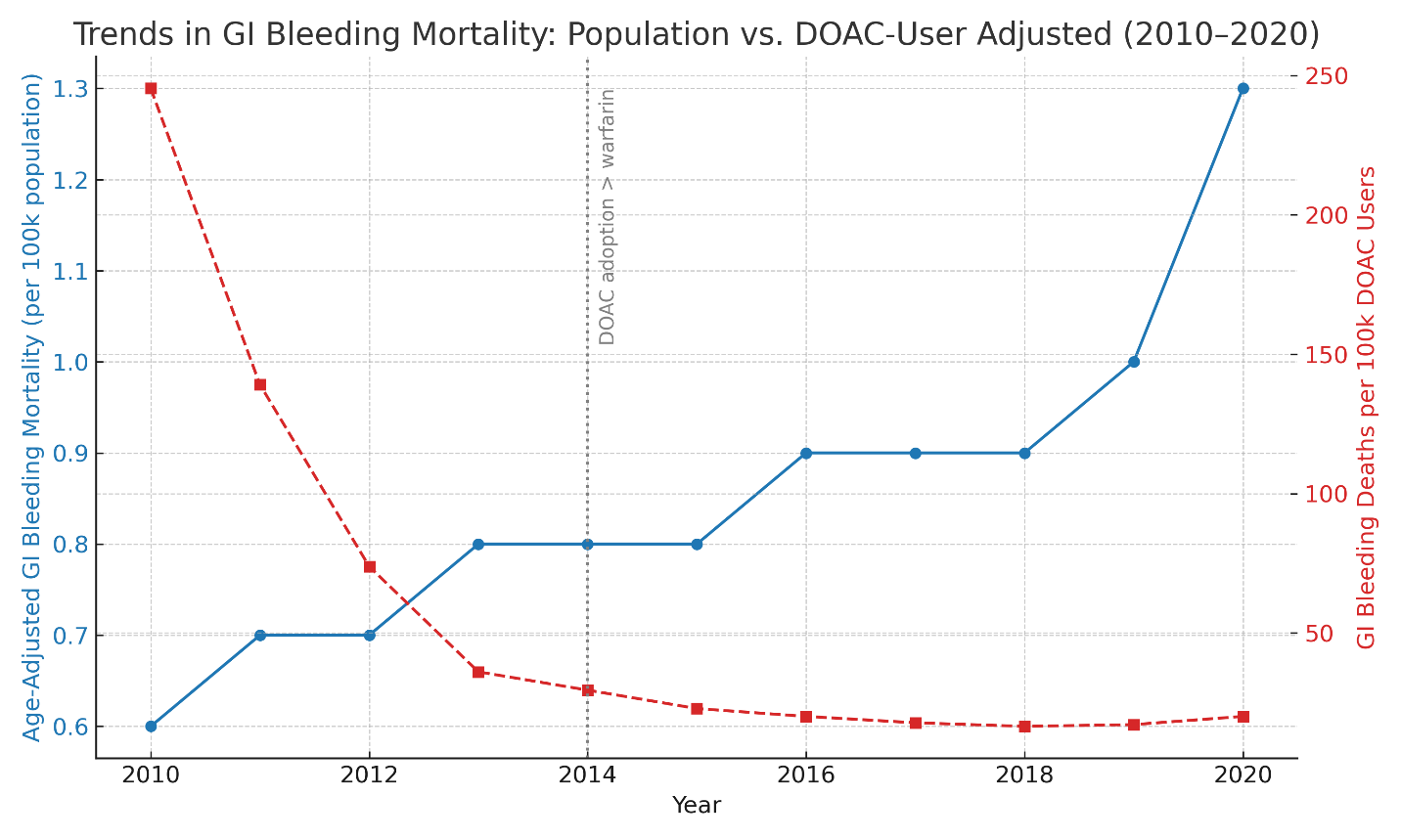
Figure: Trends in GI Bleeding Mortality: Population vs. DOAC-User–Adjusted Rates, 2010–2020
Disclosures:
Muhammad Haris Latif indicated no relevant financial relationships.
Kahee A. Mohammed indicated no relevant financial relationships.
Eman Mazhar indicated no relevant financial relationships.
Zoha Noor indicated no relevant financial relationships.
Kamran Qureshi: Gilead Sciences – Speakers Bureau. Intercept Pharmaceuticals – Speakers Bureau. Madrigal Pharmaceuticals – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Muhammad Haris Latif, MD1, Kahee A. Mohammed, MD1, Eman Mazhar, MBBS2, Zoha Noor, MBBS3, Kamran Qureshi, MD4. P5184 - Are DOACs Driving GI Bleeding Deaths? Population Trends vs Patient-Level Risk, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM St Mary's Hospital, St. Louis, MO; 2Nishtar Medical University, St. Louis, FL; 3Sialkot medical college, Orlando, FL; 4Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Direct oral anticoagulants (DOACs) have largely replaced warfarin in clinical practice due to their convenience and favorable safety profile. However, gastrointestinal (GI) bleeding remains a key complication. This study investigates the impact of DOAC adoption on GI bleeding-related mortality at the population level in the United States. It examines per-user fatality trends to clarify risk over time.
Methods: We conducted a retrospective, observational interrupted time series (ITS) study using CDC WONDER Multiple Cause of Death data (2010–2020). GI bleeding deaths were identified by ICD-10 codes and limited to cases with atrial fibrillation, pulmonary embolism, or deep vein thrombosis listed as underlying or contributing causes—surrogate markers for anticoagulant exposure. Annual oral anticoagulant utilization was estimated using CMS Medicare Part D data and published prevalence studies. GI bleeding mortality was assessed both at the population level (age-adjusted rates per 100,000) and per 100,000 estimated DOAC users. Exposure-adjusted mortality per 100,000 DOAC users was analyzed from 2010 onward, the first year with measurable DOAC use. An ITS regression model assessed changes in mortality trends pre- and post-DOAC adoption (2014 defined as the intervention point).
Results: From 2010 to 2020, age-adjusted GI bleeding mortality rose from 0.6 to 1.3 per 100,000. DOAC use increased from 0% to 72% of oral anticoagulant prescriptions during this period. Despite the population-wide rise in mortality, GI bleeding deaths per 100,000 estimated DOAC users declined sharply, from 245.4 in 2010 to 20.0 in 2020. Segmented regression showed a significant pre-DOAC upward trend (β = 0.0321, p = 0.047), a non-significant immediate drop in 2014 (β = –0.296, p = 0.082), and a non-significant slope change post-DOAC (β = 0.0357, p = 0.106).
Discussion: While overall GI bleeding mortality has increased, exposure-adjusted analysis reveals a substantial decline in fatal GI bleeding rates among DOAC users over time. These findings suggest that the per-user risk of fatal GI bleeding has decreased, potentially due to improved prescribing, better risk stratification, and enhanced management. Population-wide trends may reflect other factors, including aging demographics and broader anticoagulant use. Exposure-adjusted metrics are essential for accurate risk assessment in real-world pharmacovigilance.
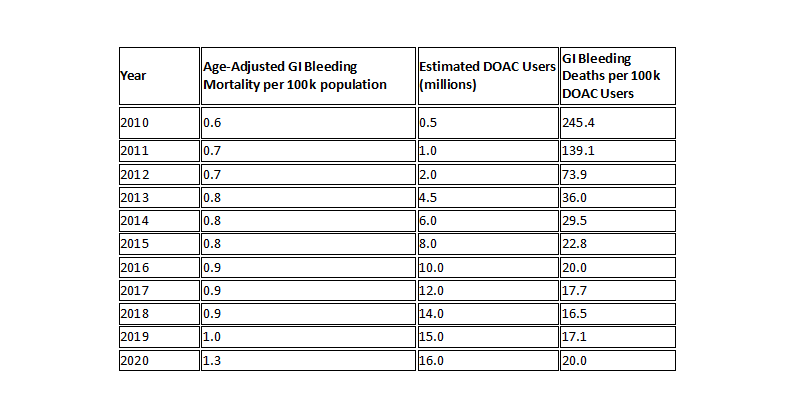
Figure: Trends in GI bleeding mortality, 2010–2020: While age-adjusted population-level mortality increased (blue), GI bleeding deaths per 100,000 DOAC users decreased significantly (red). The dashed line indicates the year of widespread DOAC adoption (2014).
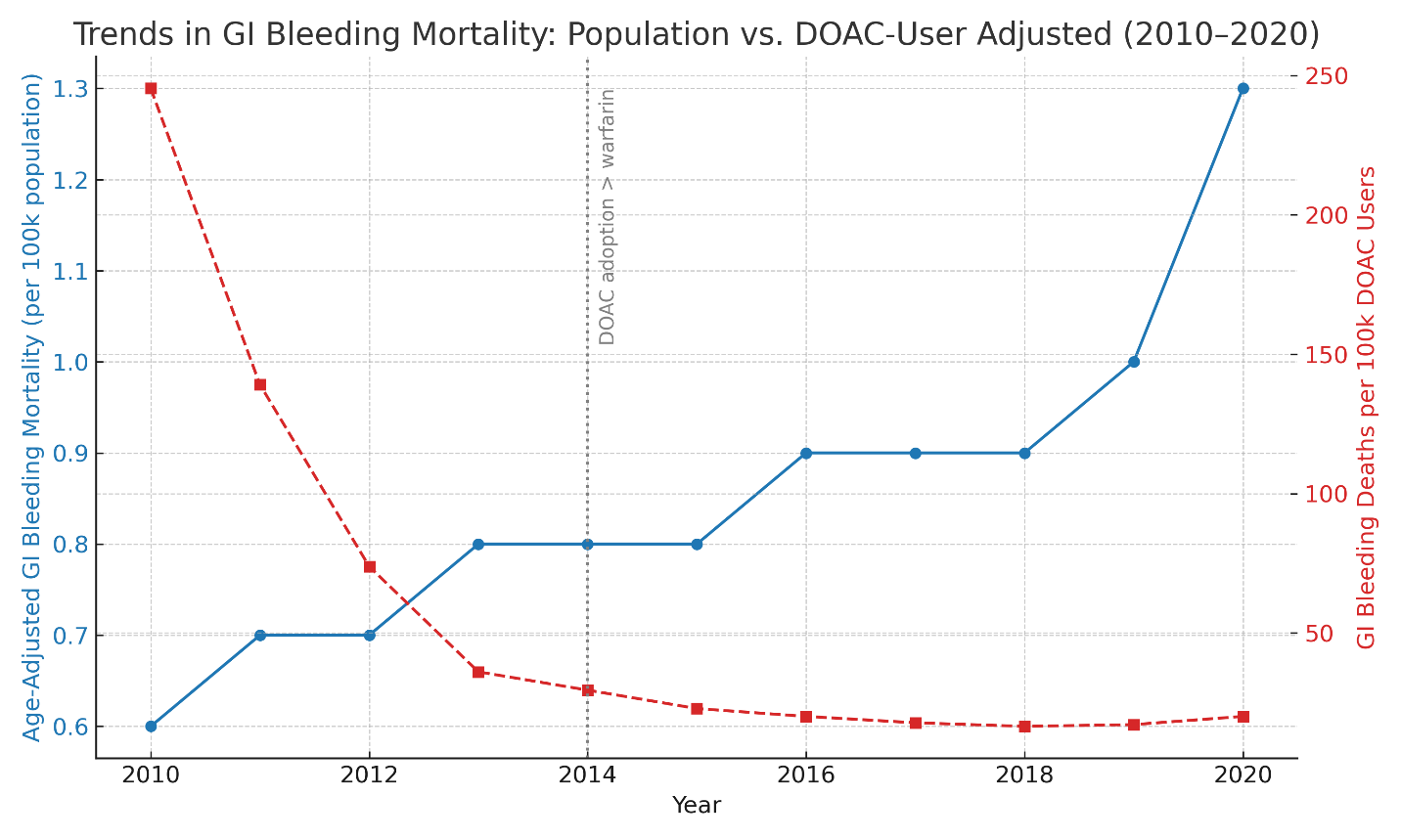
Figure: Trends in GI Bleeding Mortality: Population vs. DOAC-User–Adjusted Rates, 2010–2020
Disclosures:
Muhammad Haris Latif indicated no relevant financial relationships.
Kahee A. Mohammed indicated no relevant financial relationships.
Eman Mazhar indicated no relevant financial relationships.
Zoha Noor indicated no relevant financial relationships.
Kamran Qureshi: Gilead Sciences – Speakers Bureau. Intercept Pharmaceuticals – Speakers Bureau. Madrigal Pharmaceuticals – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Muhammad Haris Latif, MD1, Kahee A. Mohammed, MD1, Eman Mazhar, MBBS2, Zoha Noor, MBBS3, Kamran Qureshi, MD4. P5184 - Are DOACs Driving GI Bleeding Deaths? Population Trends vs Patient-Level Risk, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
