Tuesday Poster Session
Category: General Endoscopy
P5180 - Buried Bumper Syndrome of a DPEJ Tube in a Medically Complex Young Adult: Successful Endoscopic Salvage
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mina Awadallah, MD, MSc
University of Utah
Salt Lake City, UT
Presenting Author(s)
Mina Awadallah, MD, MSc1, Jessica Stout, DO1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Buried bumper syndrome (BBS) is a well recognized complication of PEG tubes, but its occurrence in direct percutaneous endoscopic jejunostomy (DPEJ) tubes is not well reported, rare and technically challenging to manage. The deeper anatomical location, thinner jejunal wall, and limited tract accessibility increase the complexity of intervention. When endoscopic salvage is not feasible, surgical management is often considered, We present a case of DPEJ-related BBS in a medically complex young adult, successfully managed endoscopically without the need for surgery, thus preserving jejunal enteral access.
Case Description/
Methods: A 21-year-old female with multiple chronic conditions—including hypermobile Ehlers-Danlos syndrome, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome, malnutrition, and long-standing reliance on both total parenteral nutrition (TPN) and enteral feeding—presented with pain and minimal oozing of viscouse fluid at the DPEJ stoma site. She also had a separate venting PEG tube. Enteroscopy revealed a buried bumper at 95 cm from the incisors with an epithelialized fistulous tract extending into the jejunal lumen. A 0.035 guidewire was passed through DPEJ tube externally then through the fistulous tract into the jejunal lumen with endoscopic visualization. The DPEJ tube was then removed via external traction over the wire. Then a 8-9-10 mm anastomotic balloon was passed over the guidewire, was used to serially dilate the tract. The stoma length measured at 3.5 cm. A 14F, 4.0 cm low-profile balloon jejunostomy tube was placed through the existing tract, and correct intrajejunal positioning was confirmed endoscopically. The procedure was completed without complication, and the patient resumed enteral feeding shortly thereafter.
Discussion: This case highlights a rare presentation of BBS involving a DPEJ tube successfully managed using a minimally invasive endoscopic approach. Although PEG-related BBS is commonly treated endoscopically, jejunal cases pose greater technical challenges due to anatomic location and tissue fragility. In complex patients, such as those with connective tissue disorders like Ehlers-Danlos syndrome, endoscopic salvage—when achievable—offers a preferable alternative to surgery, reducing procedural risk and preserving enteral access. This case adds to the limited but growing literature supporting endoscopic management of buried bumper DPEJ tubes.
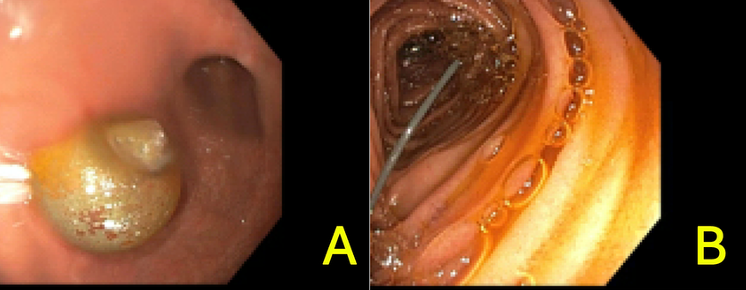
Figure: A.Buried bumper seen in the jejunum.
B.Guidwire insertion.
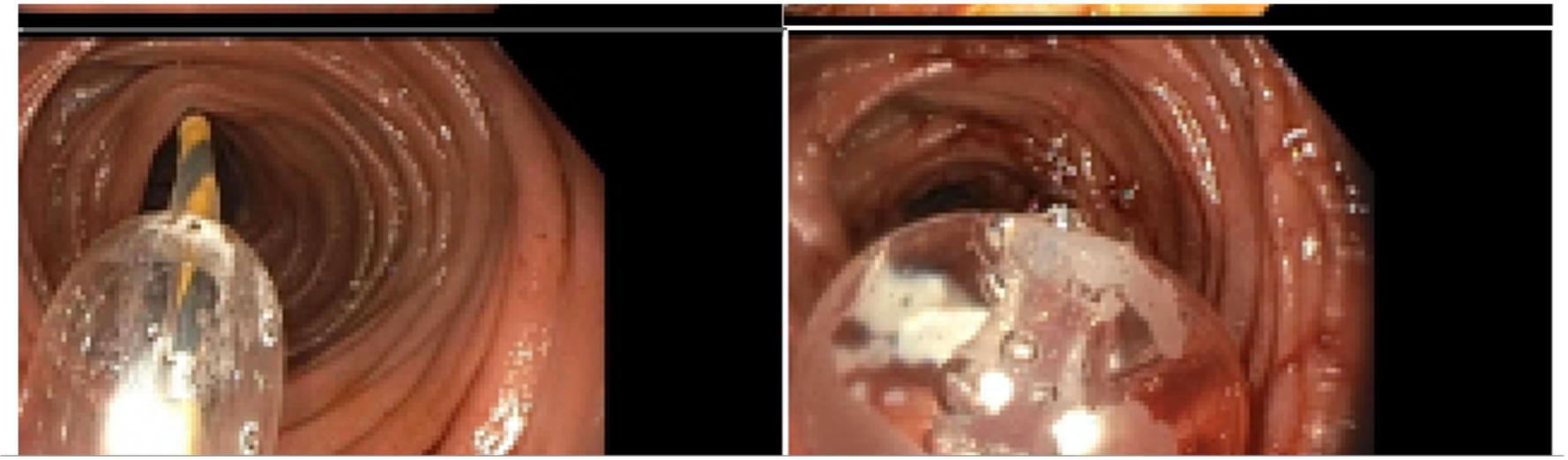
Figure: C.Serial Balloon dilation.
D.Placement of new PEJ through the dilated stoma.
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Jessica Stout: Recursion – Principle Investigator in Sponsored Trial.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Jessica Stout, DO1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2. P5180 - Buried Bumper Syndrome of a DPEJ Tube in a Medically Complex Young Adult: Successful Endoscopic Salvage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2University of Utah Health, Salt Lake City, UT
Introduction: Buried bumper syndrome (BBS) is a well recognized complication of PEG tubes, but its occurrence in direct percutaneous endoscopic jejunostomy (DPEJ) tubes is not well reported, rare and technically challenging to manage. The deeper anatomical location, thinner jejunal wall, and limited tract accessibility increase the complexity of intervention. When endoscopic salvage is not feasible, surgical management is often considered, We present a case of DPEJ-related BBS in a medically complex young adult, successfully managed endoscopically without the need for surgery, thus preserving jejunal enteral access.
Case Description/
Methods: A 21-year-old female with multiple chronic conditions—including hypermobile Ehlers-Danlos syndrome, postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome, malnutrition, and long-standing reliance on both total parenteral nutrition (TPN) and enteral feeding—presented with pain and minimal oozing of viscouse fluid at the DPEJ stoma site. She also had a separate venting PEG tube. Enteroscopy revealed a buried bumper at 95 cm from the incisors with an epithelialized fistulous tract extending into the jejunal lumen. A 0.035 guidewire was passed through DPEJ tube externally then through the fistulous tract into the jejunal lumen with endoscopic visualization. The DPEJ tube was then removed via external traction over the wire. Then a 8-9-10 mm anastomotic balloon was passed over the guidewire, was used to serially dilate the tract. The stoma length measured at 3.5 cm. A 14F, 4.0 cm low-profile balloon jejunostomy tube was placed through the existing tract, and correct intrajejunal positioning was confirmed endoscopically. The procedure was completed without complication, and the patient resumed enteral feeding shortly thereafter.
Discussion: This case highlights a rare presentation of BBS involving a DPEJ tube successfully managed using a minimally invasive endoscopic approach. Although PEG-related BBS is commonly treated endoscopically, jejunal cases pose greater technical challenges due to anatomic location and tissue fragility. In complex patients, such as those with connective tissue disorders like Ehlers-Danlos syndrome, endoscopic salvage—when achievable—offers a preferable alternative to surgery, reducing procedural risk and preserving enteral access. This case adds to the limited but growing literature supporting endoscopic management of buried bumper DPEJ tubes.
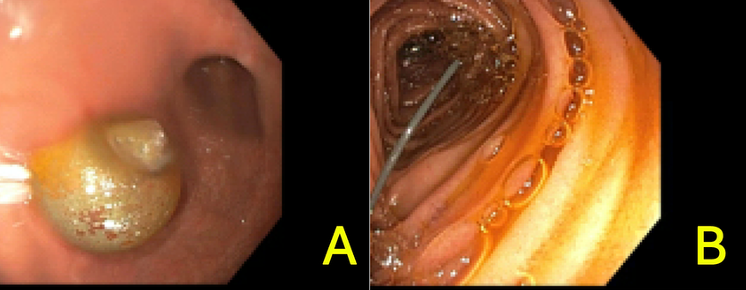
Figure: A.Buried bumper seen in the jejunum.
B.Guidwire insertion.
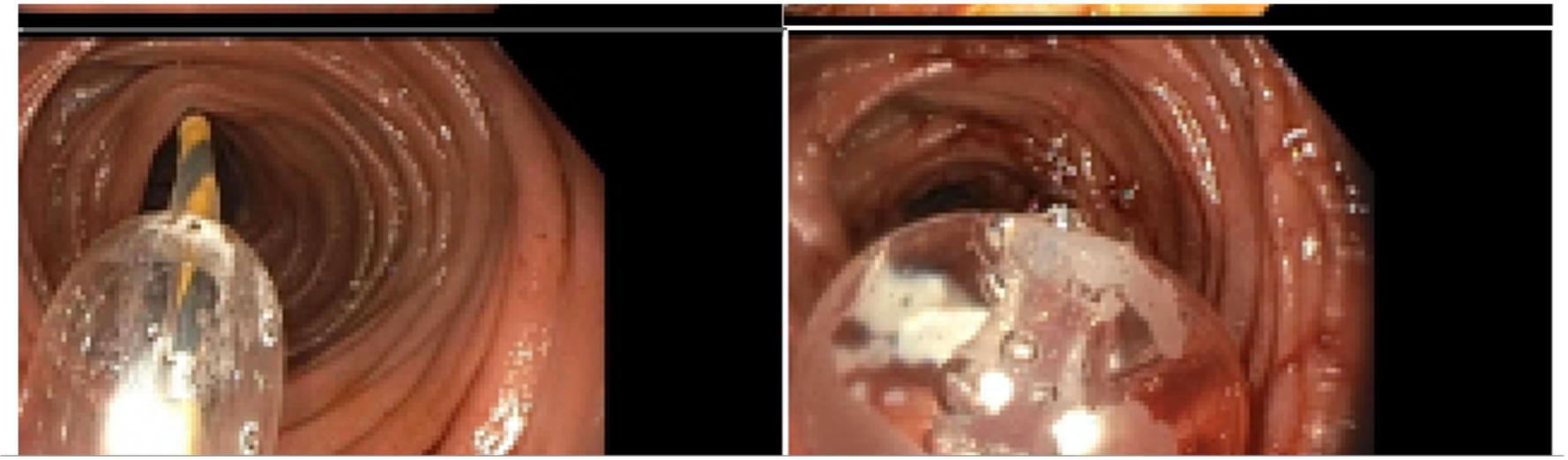
Figure: C.Serial Balloon dilation.
D.Placement of new PEJ through the dilated stoma.
Disclosures:
Mina Awadallah indicated no relevant financial relationships.
Jessica Stout: Recursion – Principle Investigator in Sponsored Trial.
John Fang: Aspero Medical – Consultant. Circa Scientific – Consultant. Merit – Consultant.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Mina Awadallah, MD, MSc1, Jessica Stout, DO1, John Fang, MD1, John Erikson Yap, MD, MBA, FACG2. P5180 - Buried Bumper Syndrome of a DPEJ Tube in a Medically Complex Young Adult: Successful Endoscopic Salvage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
