Tuesday Poster Session
Category: GI Bleeding
P5261 - Severe Metastatic Melanoma Unamenable to Therapeutic Interventions
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Neel Matiwala, MD
Saint Louis University School of Medicine
Saint Louis, MO
Presenting Author(s)
Neel Matiwala, MD1, Nikhil Jacob, BS2, Christian Khmoro, BS3, Rohan Tripathi, MD1, Erica C. Becker, MD, MPH4, Ameya Deshmukh, DO4, Adam D. Farmer, MD, PhD5
1Saint Louis University School of Medicine, Saint Louis, MO; 2Kansas City University College of Osteopathic Medicine, Joplin, MO; 3A.T Still University - Kirksville College of Osteopathic Medicine, Kirksville, MO; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: Melanoma, characterized by uncontrolled melanocyte proliferation, is highly metastatic, often spreading to the gastrointestinal (GI) tract. GI metastases may cause obstruction, abdominal pain, or bleeding. It is diagnosed via imaging and endoscopy. Management options include endoscopic procedures, radiation, systemic therapies, or resection. We report a severe case of metastatic melanoma with diffuse polypoid GI lesions, indicating a poor prognosis and limited therapeutic options due to extensive disease progression.
Case Description/
Methods: A 56-year-old male with metastatic melanoma presented with a new rash following immunotherapy initiation. He was diagnosed two months earlier with imaging revealing widespread lesions in the lungs, liver, spleen, and subcutaneous tissues. He was admitted for suspected checkpoint inhibitor-related dermatitis although his hospital course was complicated by hematemesis, hematochezia, and recurrent hemoglobin drops to ~6 g/dL without hemodynamic instability. Abdominal CT demonstrated hepatosplenic metastases and enhancing bowel nodules. Esophagogastroduodenoscopy revealed extensive nodular mucosa in the lower esophagus, stomach, and duodenum. Colonoscopy identified smaller nodules in the left colon with friable mucosa. Histology confirmed diffuse infiltrative melanoma as the likely source of GI bleeding. Due to extensive infiltration, endoscopic interventions, palliative surgery, or radiation were not viable. After multidisciplinary input, the patient was transitioned to end of life care.
Discussion: This case underscores the aggressive nature of metastatic melanoma, with GI involvement often affecting the small bowel and stomach, as observed here. Metastatic risk correlates with primary melanoma thickness. No specific risk factors for GI metastasis have been conclusively established, but early skin cancer detection is critical. The extensive disease precluded guideline-based interventions, highlighting the need for timely diagnosis to improve prognosis and treatment options.
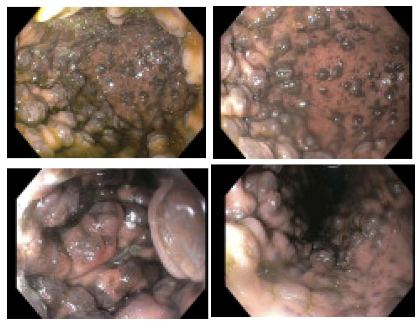
Figure: Severe malignant melanoma within the lumen of the stomach identified during EGD.
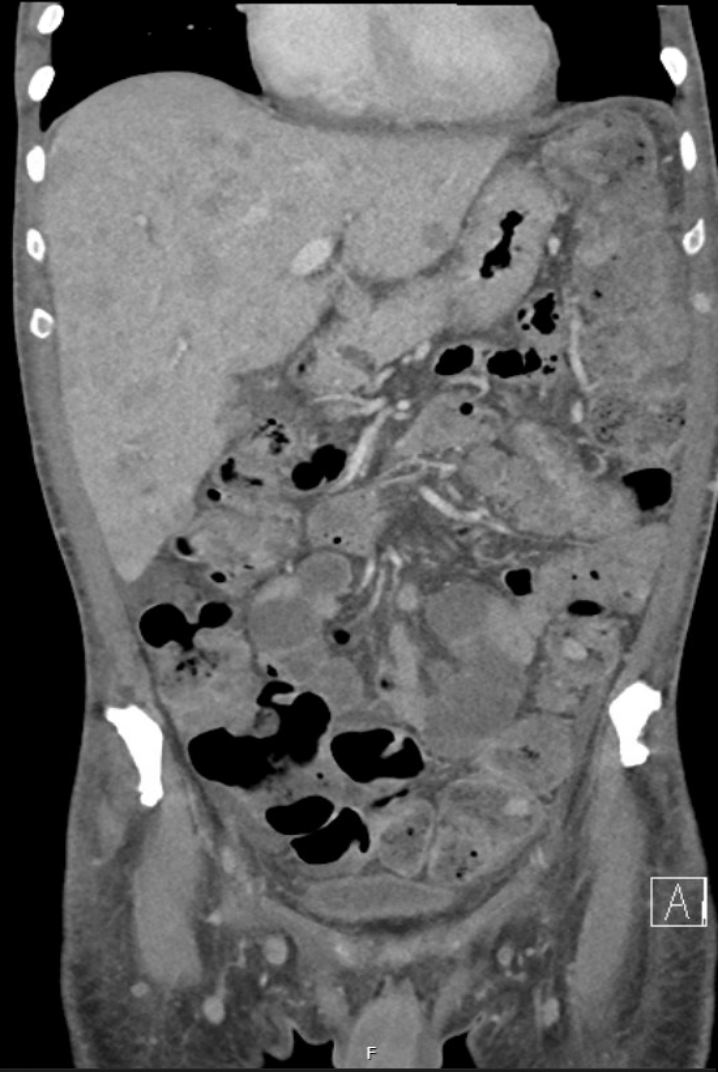
Figure: Severe hepatosplenic metastases with nodules throughout bowel on CT abdomen.
Disclosures:
Neel Matiwala indicated no relevant financial relationships.
Nikhil Jacob indicated no relevant financial relationships.
Christian Khmoro indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Erica Becker indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Neel Matiwala, MD1, Nikhil Jacob, BS2, Christian Khmoro, BS3, Rohan Tripathi, MD1, Erica C. Becker, MD, MPH4, Ameya Deshmukh, DO4, Adam D. Farmer, MD, PhD5. P5261 - Severe Metastatic Melanoma Unamenable to Therapeutic Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Louis University School of Medicine, Saint Louis, MO; 2Kansas City University College of Osteopathic Medicine, Joplin, MO; 3A.T Still University - Kirksville College of Osteopathic Medicine, Kirksville, MO; 4SSM Health Saint Louis University Hospital, St. Louis, MO; 5SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: Melanoma, characterized by uncontrolled melanocyte proliferation, is highly metastatic, often spreading to the gastrointestinal (GI) tract. GI metastases may cause obstruction, abdominal pain, or bleeding. It is diagnosed via imaging and endoscopy. Management options include endoscopic procedures, radiation, systemic therapies, or resection. We report a severe case of metastatic melanoma with diffuse polypoid GI lesions, indicating a poor prognosis and limited therapeutic options due to extensive disease progression.
Case Description/
Methods: A 56-year-old male with metastatic melanoma presented with a new rash following immunotherapy initiation. He was diagnosed two months earlier with imaging revealing widespread lesions in the lungs, liver, spleen, and subcutaneous tissues. He was admitted for suspected checkpoint inhibitor-related dermatitis although his hospital course was complicated by hematemesis, hematochezia, and recurrent hemoglobin drops to ~6 g/dL without hemodynamic instability. Abdominal CT demonstrated hepatosplenic metastases and enhancing bowel nodules. Esophagogastroduodenoscopy revealed extensive nodular mucosa in the lower esophagus, stomach, and duodenum. Colonoscopy identified smaller nodules in the left colon with friable mucosa. Histology confirmed diffuse infiltrative melanoma as the likely source of GI bleeding. Due to extensive infiltration, endoscopic interventions, palliative surgery, or radiation were not viable. After multidisciplinary input, the patient was transitioned to end of life care.
Discussion: This case underscores the aggressive nature of metastatic melanoma, with GI involvement often affecting the small bowel and stomach, as observed here. Metastatic risk correlates with primary melanoma thickness. No specific risk factors for GI metastasis have been conclusively established, but early skin cancer detection is critical. The extensive disease precluded guideline-based interventions, highlighting the need for timely diagnosis to improve prognosis and treatment options.
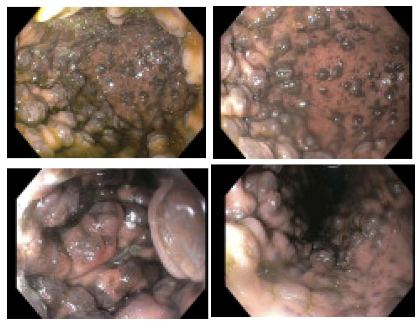
Figure: Severe malignant melanoma within the lumen of the stomach identified during EGD.
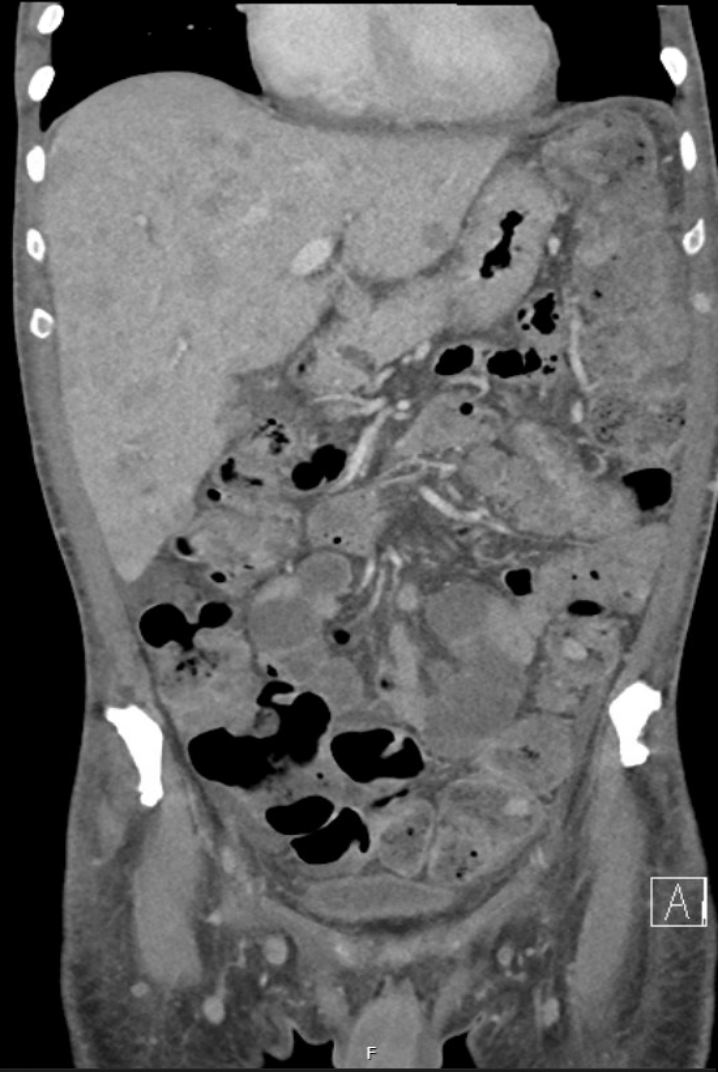
Figure: Severe hepatosplenic metastases with nodules throughout bowel on CT abdomen.
Disclosures:
Neel Matiwala indicated no relevant financial relationships.
Nikhil Jacob indicated no relevant financial relationships.
Christian Khmoro indicated no relevant financial relationships.
Rohan Tripathi indicated no relevant financial relationships.
Erica Becker indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Neel Matiwala, MD1, Nikhil Jacob, BS2, Christian Khmoro, BS3, Rohan Tripathi, MD1, Erica C. Becker, MD, MPH4, Ameya Deshmukh, DO4, Adam D. Farmer, MD, PhD5. P5261 - Severe Metastatic Melanoma Unamenable to Therapeutic Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
