Tuesday Poster Session
Category: GI Bleeding
P5260 - Refractory Hematemesis in ESRD: When the Clot Blocks the Way
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nicole Villa, MD (she/her/hers)
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Nicole Villa, MD, Fnu Samaksh, MD, Julio C. Valencia-Manrique, MD, Jennifer Harley, MD
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Upper gastrointestinal bleeding (UGIB) remains an emergency requiring timely diagnosis and intervention. In patients with ESRD, the risk and severity of bleeding are increased due to platelet dysfunction, uremic coagulopathy, and comorbidities. This case illustrates a challenging scenario of recurrent hematemesis requiring multidisciplinary intervention.
Case Description/
Methods: A 59-year-old woman with a history of ESRD, type 2 diabetes, hypertension, obesity, asthma, and treated endometrial carcinoma presented with hematemesis. She reported several episodes of red blood emesis associated to abdominal pain. On arrival, she was tachycardic to 110 bpm; pale and exhibited epigastric tenderness. Laboratory studies revealed a hemoglobin of 6.9 g/dL (baseline ~9 g/dL), BUN 37 mg/dL, and creatinine 3.7 mg/dL. Her coagulation profile was normal. She was intubated for airway protection and underwent urgent EGD, which revealed pooling of blood in the hypopharynx and a large, adherent clot occluding the proximal esophagus, precluding the passage of even a neonatal scope. Attempts to disrupt the clot using a Roth net or rat-tooth forceps were unsuccessful. The procedure was aborted due to limited visualization and concern for bleeding upon clot dislodgment. Emergent CT angiography demonstrated no active bleeding. Despite transfusion of 4 units of PRBCs, hemoglobin rose only to 7.3 g/dL. Given the concerns for ongoing hemorrhage, the patient was transferred to a tertiary care center with cardiothoracic surgical support. Unexpectedly, repeat EGD revealed Los Angeles D esophagitis without active bleeding, ulceration, or mucosal tears. She was managed with PPI therapy and discharged home. Five months later, she was readmitted with recurrent hematemesis. EGD revealed extensive blood clots in the gastroesophageal junction and stomach, which could not be cleared, preventing identification of the source. Interventional radiology was consulted, and emergent embolization of the gastroduodenal artery was successfully performed.
Discussion: Compared to the general population, ESRD patients face a five-fold increased risk of UGIB. Common causes include ulcers, erosions, and angiodysplasia. Despite advances in endoscopic and imaging techniques, active bleeding may go undetected, particularly in intermittent or low-flow cases. This case highlights the limitations of conventional diagnostic tools and underscores the importance of interdisciplinary collaboration to manage complex bleeding in high-risk populations.
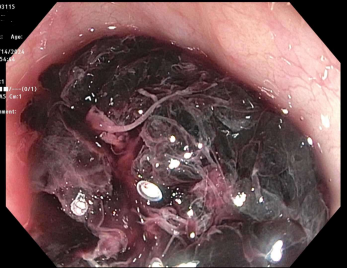
Figure: Significant amount of clotted blood in the upper third of the esophagus blocking passage of scope
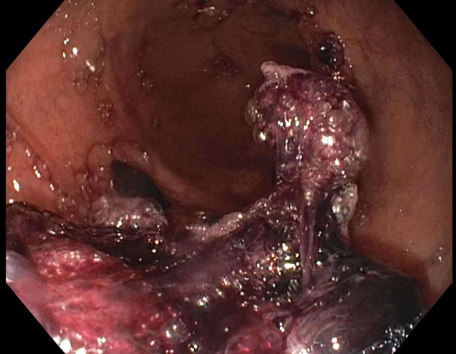
Figure: Extensive blood clots covering the stomach were appreciated on repeat EGD on the second admission
Disclosures:
Nicole Villa indicated no relevant financial relationships.
Fnu Samaksh indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Nicole Villa, MD, Fnu Samaksh, MD, Julio C. Valencia-Manrique, MD, Jennifer Harley, MD. P5260 - Refractory Hematemesis in ESRD: When the Clot Blocks the Way, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Upper gastrointestinal bleeding (UGIB) remains an emergency requiring timely diagnosis and intervention. In patients with ESRD, the risk and severity of bleeding are increased due to platelet dysfunction, uremic coagulopathy, and comorbidities. This case illustrates a challenging scenario of recurrent hematemesis requiring multidisciplinary intervention.
Case Description/
Methods: A 59-year-old woman with a history of ESRD, type 2 diabetes, hypertension, obesity, asthma, and treated endometrial carcinoma presented with hematemesis. She reported several episodes of red blood emesis associated to abdominal pain. On arrival, she was tachycardic to 110 bpm; pale and exhibited epigastric tenderness. Laboratory studies revealed a hemoglobin of 6.9 g/dL (baseline ~9 g/dL), BUN 37 mg/dL, and creatinine 3.7 mg/dL. Her coagulation profile was normal. She was intubated for airway protection and underwent urgent EGD, which revealed pooling of blood in the hypopharynx and a large, adherent clot occluding the proximal esophagus, precluding the passage of even a neonatal scope. Attempts to disrupt the clot using a Roth net or rat-tooth forceps were unsuccessful. The procedure was aborted due to limited visualization and concern for bleeding upon clot dislodgment. Emergent CT angiography demonstrated no active bleeding. Despite transfusion of 4 units of PRBCs, hemoglobin rose only to 7.3 g/dL. Given the concerns for ongoing hemorrhage, the patient was transferred to a tertiary care center with cardiothoracic surgical support. Unexpectedly, repeat EGD revealed Los Angeles D esophagitis without active bleeding, ulceration, or mucosal tears. She was managed with PPI therapy and discharged home. Five months later, she was readmitted with recurrent hematemesis. EGD revealed extensive blood clots in the gastroesophageal junction and stomach, which could not be cleared, preventing identification of the source. Interventional radiology was consulted, and emergent embolization of the gastroduodenal artery was successfully performed.
Discussion: Compared to the general population, ESRD patients face a five-fold increased risk of UGIB. Common causes include ulcers, erosions, and angiodysplasia. Despite advances in endoscopic and imaging techniques, active bleeding may go undetected, particularly in intermittent or low-flow cases. This case highlights the limitations of conventional diagnostic tools and underscores the importance of interdisciplinary collaboration to manage complex bleeding in high-risk populations.
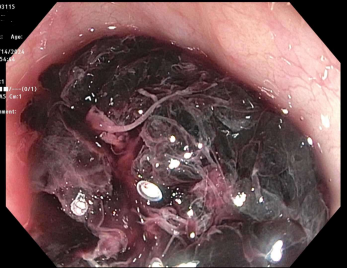
Figure: Significant amount of clotted blood in the upper third of the esophagus blocking passage of scope
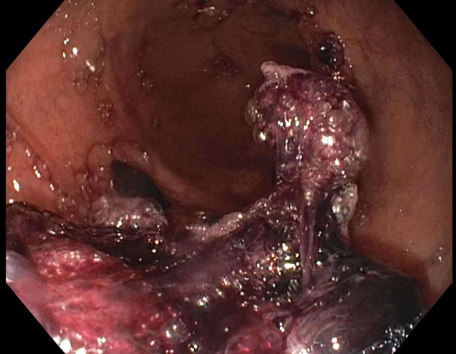
Figure: Extensive blood clots covering the stomach were appreciated on repeat EGD on the second admission
Disclosures:
Nicole Villa indicated no relevant financial relationships.
Fnu Samaksh indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Nicole Villa, MD, Fnu Samaksh, MD, Julio C. Valencia-Manrique, MD, Jennifer Harley, MD. P5260 - Refractory Hematemesis in ESRD: When the Clot Blocks the Way, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
