Tuesday Poster Session
Category: GI Bleeding
P5259 - Metastatic Mantle Cell Lymphoma Presenting as Hematemesis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samar Pal S. Sandhu, MBBS
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Samar Pal S. Sandhu, MBBS, Tanuj Chokshi, DO, Henry Brejt, MD
Maimonides Medical Center, Brooklyn, NY
Introduction: Mantle cell lymphoma (MCL) is a B-cell non-Hodgkin lymphoma, with the gastrointestinal(GI) tract being the most common extranodal site. It is characterized by the malignant transformation of B cells, classically with the t(11;14) chromosomal translocation. MCL is considered a rare cause of GI bleeding; if present, it is scarcely severe. We present a case of MCL presenting as a severe GI bleed in the form of hematemesis.
Case Description/
Methods: A 78-year-old male with a history of hypertension, type 2 diabetes mellitus, and a former heavy smoker presented with hematemesis and melena. He had recently been hospitalized for peripheral arterial disease complicated by left third toe gangrene requiring amputation, after which he was discharged on rivaroxaban. On presentation, he was hemodynamically stable but profoundly anemic (Hb 5.2 g/dL; baseline ~9 g/dL) with a BUN/Cr ratio of 52/1.4, suggestive of upper GI bleeding. He denied NSAID use or prior GI bleeding. Following transfusion of 2 units of packed red blood cells, esophagogastroduodenoscopy(EGD) revealed a large, ulcerated, fungating mass at the gastroesophageal junction and gastric cardia with stigmata of recent bleeding, initially suggestive of a Siewert type II adenocarcinoma. Additional findings included erythematous fundic mucosa, non-bleeding gastric ulcers, and a duodenal ulcer. Histopathology demonstrated an atypical lymphoid infiltrate with plasmacytic differentiation. Immunohistochemistry was positive for CD20, PAX-5, cyclin D1, SOX11, and CD5 (dim), and negative for CD10, CD23, and BCL-6, consistent with MCL. Ki-67 revealed a low proliferative index. Imaging showed gastric wall thickening, intra-abdominal lymphadenopathy, pulmonary nodules, and splenomegaly. Hematology was consulted for systemic MCL management.
Discussion: MCL has a heterogeneous presentation. GI tract involvement is common, with the majority being subclinical; however, it can range from asymptomatic to nonspecific symptoms like abdominal pain, diarrhea, weight loss, or occult to overt GI bleeding. MCL can present endoscopically as isolated or confluent polypoid lesions, submucosal nodules, and, less commonly, as ulcerative, fungating, or infiltrative masses, making it indistinguishable from other GI cancers. Our case underscores a rare primary presentation of MCL as severe GI bleeding and emphasizes the critical role of early biopsy and immunophenotyping for accurate diagnosis due to its endoscopic overlap with gastric adenocarcinoma.
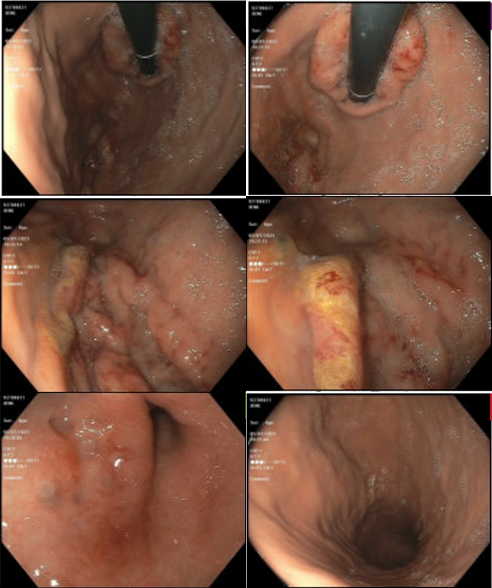
Figure: EGD showing a large, ulcerated, fungating mass at the gastroesophageal junction and gastric cardia with stigmata of recent bleeding
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Henry Brejt indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS, Tanuj Chokshi, DO, Henry Brejt, MD. P5259 - Metastatic Mantle Cell Lymphoma Presenting as Hematemesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Maimonides Medical Center, Brooklyn, NY
Introduction: Mantle cell lymphoma (MCL) is a B-cell non-Hodgkin lymphoma, with the gastrointestinal(GI) tract being the most common extranodal site. It is characterized by the malignant transformation of B cells, classically with the t(11;14) chromosomal translocation. MCL is considered a rare cause of GI bleeding; if present, it is scarcely severe. We present a case of MCL presenting as a severe GI bleed in the form of hematemesis.
Case Description/
Methods: A 78-year-old male with a history of hypertension, type 2 diabetes mellitus, and a former heavy smoker presented with hematemesis and melena. He had recently been hospitalized for peripheral arterial disease complicated by left third toe gangrene requiring amputation, after which he was discharged on rivaroxaban. On presentation, he was hemodynamically stable but profoundly anemic (Hb 5.2 g/dL; baseline ~9 g/dL) with a BUN/Cr ratio of 52/1.4, suggestive of upper GI bleeding. He denied NSAID use or prior GI bleeding. Following transfusion of 2 units of packed red blood cells, esophagogastroduodenoscopy(EGD) revealed a large, ulcerated, fungating mass at the gastroesophageal junction and gastric cardia with stigmata of recent bleeding, initially suggestive of a Siewert type II adenocarcinoma. Additional findings included erythematous fundic mucosa, non-bleeding gastric ulcers, and a duodenal ulcer. Histopathology demonstrated an atypical lymphoid infiltrate with plasmacytic differentiation. Immunohistochemistry was positive for CD20, PAX-5, cyclin D1, SOX11, and CD5 (dim), and negative for CD10, CD23, and BCL-6, consistent with MCL. Ki-67 revealed a low proliferative index. Imaging showed gastric wall thickening, intra-abdominal lymphadenopathy, pulmonary nodules, and splenomegaly. Hematology was consulted for systemic MCL management.
Discussion: MCL has a heterogeneous presentation. GI tract involvement is common, with the majority being subclinical; however, it can range from asymptomatic to nonspecific symptoms like abdominal pain, diarrhea, weight loss, or occult to overt GI bleeding. MCL can present endoscopically as isolated or confluent polypoid lesions, submucosal nodules, and, less commonly, as ulcerative, fungating, or infiltrative masses, making it indistinguishable from other GI cancers. Our case underscores a rare primary presentation of MCL as severe GI bleeding and emphasizes the critical role of early biopsy and immunophenotyping for accurate diagnosis due to its endoscopic overlap with gastric adenocarcinoma.
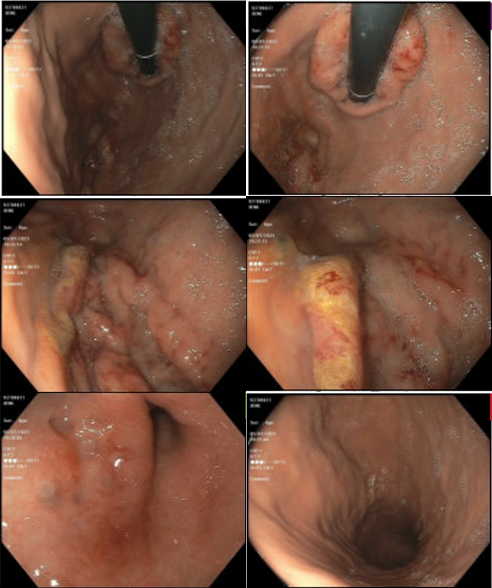
Figure: EGD showing a large, ulcerated, fungating mass at the gastroesophageal junction and gastric cardia with stigmata of recent bleeding
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Henry Brejt indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS, Tanuj Chokshi, DO, Henry Brejt, MD. P5259 - Metastatic Mantle Cell Lymphoma Presenting as Hematemesis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
