Tuesday Poster Session
Category: GI Bleeding
P5258 - Hidden Culprit: Dieulafoy Lesion Within a Distal Duodenal Diverticulum Causing Severe GI Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samar Pal S. Sandhu, MBBS
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Brandon M. Cunha, BS2, Tanuj Chokshi, DO1, Ira Mayer, MD, FACG1, Seth Lapin, DO1
1Maimonides Medical Center, Brooklyn, NY; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ
Introduction: A Dieulafoy lesion (DL) is a dilated, tortuous submucosal vessel that erodes through the epithelium without any surrounding ulceration. These lesions are typically identified in the stomach, but can manifest anywhere along the GI tract. We present a case of severe GI bleeding due to DL present in a diverticulum in the distal part of the duodenum.
Case Description/
Methods: A 92-year-old male with a history of atrial fibrillation on apixaban, heart failure with preserved ejection fraction (EF 60%), and chronic kidney disease presented to the hospital with several days of melena followed by acute hematemesis. Initial evaluation revealed a hemoglobin drop from 11.0 g/dL to 7.7 g/dL with relative hemodynamic instability. CT angiography identified active arterial extravasation in the duodenum, which was not amenable to endovascular embolization.
Esophagogastroduodenoscopy (EGD) was initially deferred due to left lower lobe pneumonia, causing respiratory failure. The patient was stabilized and underwent EGD, which revealed a bleeding DL within a diverticulum in the distal part of the duodenum (D4). Endoscopic hemostasis was achieved with epinephrine injection, dual endoclip placement, and topical hemostatic material. Despite this, the patient experienced recurrent melena with ongoing transfusion requirements and further hemoglobin decline.
Given persistent bleeding, the patient underwent empiric coil embolization of the inferior pancreaticoduodenal artery (IPDA) by interventional radiology. Post-procedurally, there was no further evidence of gastrointestinal bleeding, hemoglobin levels stabilized, and the patient was discharged home.
Discussion: Extra gastric DL are most commonly located in the duodenum bulb and are rare in the distal portion of the duodenum. They can often be difficult to diagnose endoscopically given their subtle appearance, propensity to bleed intermittently, and location in atypical or anatomically complex locations, as seen in our case, resulting in potentially life-threatening bleeding. Despite endoscopic hemostasis being first line, it may not be definitive in diverticular DL, due to the higher risk of rebleeding and perforation given the thinner wall of duodenal diverticulum. Our case emphasizes the necessity for exhaustive endoscopic assessment for accurate diagnosis and the need for early escalation to multimodal management if rebleeding occurs despite endoscopic intervention to prevent morbidity and mortality.
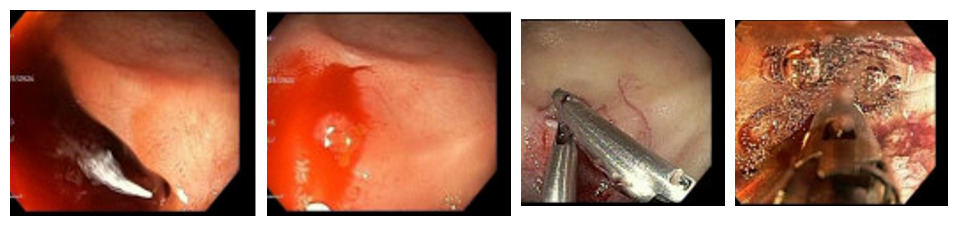
Figure: EGD showing a Dieulafoy lesion in the distal duodenal diverticulum before and after hemostasis
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Brandon Cunha indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Ira Mayer indicated no relevant financial relationships.
Seth Lapin indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Brandon M. Cunha, BS2, Tanuj Chokshi, DO1, Ira Mayer, MD, FACG1, Seth Lapin, DO1. P5258 - Hidden Culprit: Dieulafoy Lesion Within a Distal Duodenal Diverticulum Causing Severe GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ
Introduction: A Dieulafoy lesion (DL) is a dilated, tortuous submucosal vessel that erodes through the epithelium without any surrounding ulceration. These lesions are typically identified in the stomach, but can manifest anywhere along the GI tract. We present a case of severe GI bleeding due to DL present in a diverticulum in the distal part of the duodenum.
Case Description/
Methods: A 92-year-old male with a history of atrial fibrillation on apixaban, heart failure with preserved ejection fraction (EF 60%), and chronic kidney disease presented to the hospital with several days of melena followed by acute hematemesis. Initial evaluation revealed a hemoglobin drop from 11.0 g/dL to 7.7 g/dL with relative hemodynamic instability. CT angiography identified active arterial extravasation in the duodenum, which was not amenable to endovascular embolization.
Esophagogastroduodenoscopy (EGD) was initially deferred due to left lower lobe pneumonia, causing respiratory failure. The patient was stabilized and underwent EGD, which revealed a bleeding DL within a diverticulum in the distal part of the duodenum (D4). Endoscopic hemostasis was achieved with epinephrine injection, dual endoclip placement, and topical hemostatic material. Despite this, the patient experienced recurrent melena with ongoing transfusion requirements and further hemoglobin decline.
Given persistent bleeding, the patient underwent empiric coil embolization of the inferior pancreaticoduodenal artery (IPDA) by interventional radiology. Post-procedurally, there was no further evidence of gastrointestinal bleeding, hemoglobin levels stabilized, and the patient was discharged home.
Discussion: Extra gastric DL are most commonly located in the duodenum bulb and are rare in the distal portion of the duodenum. They can often be difficult to diagnose endoscopically given their subtle appearance, propensity to bleed intermittently, and location in atypical or anatomically complex locations, as seen in our case, resulting in potentially life-threatening bleeding. Despite endoscopic hemostasis being first line, it may not be definitive in diverticular DL, due to the higher risk of rebleeding and perforation given the thinner wall of duodenal diverticulum. Our case emphasizes the necessity for exhaustive endoscopic assessment for accurate diagnosis and the need for early escalation to multimodal management if rebleeding occurs despite endoscopic intervention to prevent morbidity and mortality.
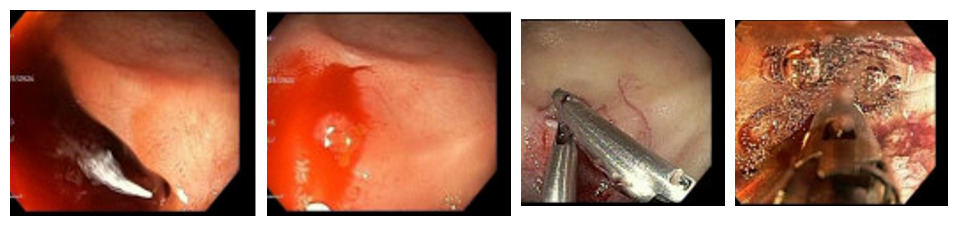
Figure: EGD showing a Dieulafoy lesion in the distal duodenal diverticulum before and after hemostasis
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Brandon Cunha indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Ira Mayer indicated no relevant financial relationships.
Seth Lapin indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Brandon M. Cunha, BS2, Tanuj Chokshi, DO1, Ira Mayer, MD, FACG1, Seth Lapin, DO1. P5258 - Hidden Culprit: Dieulafoy Lesion Within a Distal Duodenal Diverticulum Causing Severe GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
