Tuesday Poster Session
Category: IBD
P5345 - Human Immunodeficiency Virus Co-infection and Cancer Risk in Inflammatory Bowel Disease: Results From a Large National Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MM
Mouhand Mohamed, MBBS, MS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mouhand Mohamed, MBBS, MS1, Osama Hamid, MD2, Azizullah Beran, MD3, Jana G. Hashash, MD, MSc, FACG4, Victor Chedid, MD, MSc1
1Mayo Clinic, Rochester, MN; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Indiana University School of Medicine, Indianapolis, IN; 4Mayo Clinic, Jacksonville, FL
Introduction: Recent data suggest that inflammatory bowel disease (IBD) in people living with HIV (PLWH) often follows a less aggressive course and is managed with fewer advanced therapies. Both HIV infection and IBD independently increase cancer risk, yet it is unclear whether the combined burden further amplifies that risk.
Methods: We queried the U.S. TriNetX collaborative network (comprising >100 million patient records). Using ICD 10 codes, we identified Adults (≥18 y) with ≥3 IBD encounters who received an IBD therapy. We compared IBD in PLWH compared to IBD alone. A propensity score matching (PSM) was performed for age, sex, race, and key comorbidities. Outcomes included risks of colorectal or anal cancer, colorectal cancer alone, anal cancer, anal cancer or dysplasia, colectomy, and risk of skin cancers. Hazard ratios (HR) with corresponding 95% confidence intervals were estimated; P value < 0.05 suggested statistical significance.
Results: After PSM, 1,329 patients were included in each group. The median follow-up duration was 1,425 days in the IBD-HIV cohort, compared to 1,610 days in the controls. HIV co-infection was not associated with higher hazards of combined colorectal or anal cancer (HR 1.30, 95 % CI 0.84–2.03, p = 0.22) or colorectal cancer alone (HR 1.10, 0.68–1.78, p = 0.41). In contrast, anal cancer ( HR 4.80, 1.82–12.61, p = < 0.001) and anal cancer or dysplasia risks (HR 11.54, 6.53–20.39, p = 0.007) were markedly increased. Colectomy occurred less often with HIV (HR 0.52, 0.32–0.85, p = 0.008). Cutaneous melanoma/skin cancer risk did not differ (HR 1.43, 0.92–2.23, p = 0.63).
Discussion: In this large, matched cohort, HIV did not increase colorectal cancer risk in IBD but was strongly associated with anal cancer and anal dysplasia while appearing protective against colectomy. These findings argue for better screening strategies in PLWH with IBD while maintaining standard colorectal dysplasia screening. Prospective studies are needed to clarify the mechanisms underlying these observations and to verify whether the relatively milder IBD course activity in PLWH persists long term. Limitations of this study include the retrospective nature, reliance on ICD codes, and potential for residual confounding. Thus, further research is warranted to validate these findings.
Disclosure: Supervised AI assisted with table generation but not data analysis.
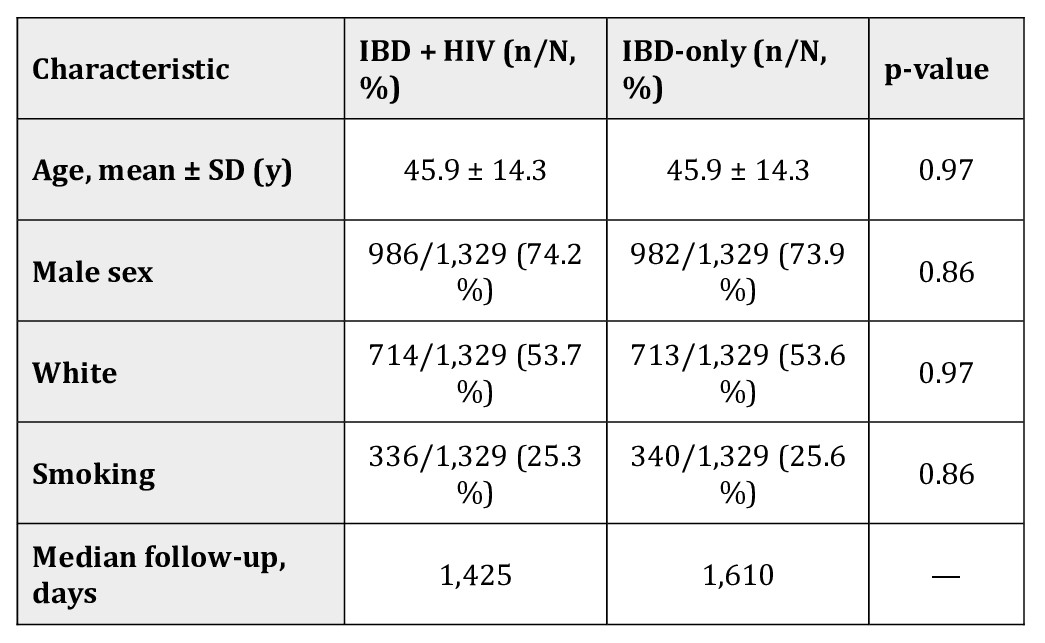
Figure: Table 1. Baseline characteristics after propensity-score matching
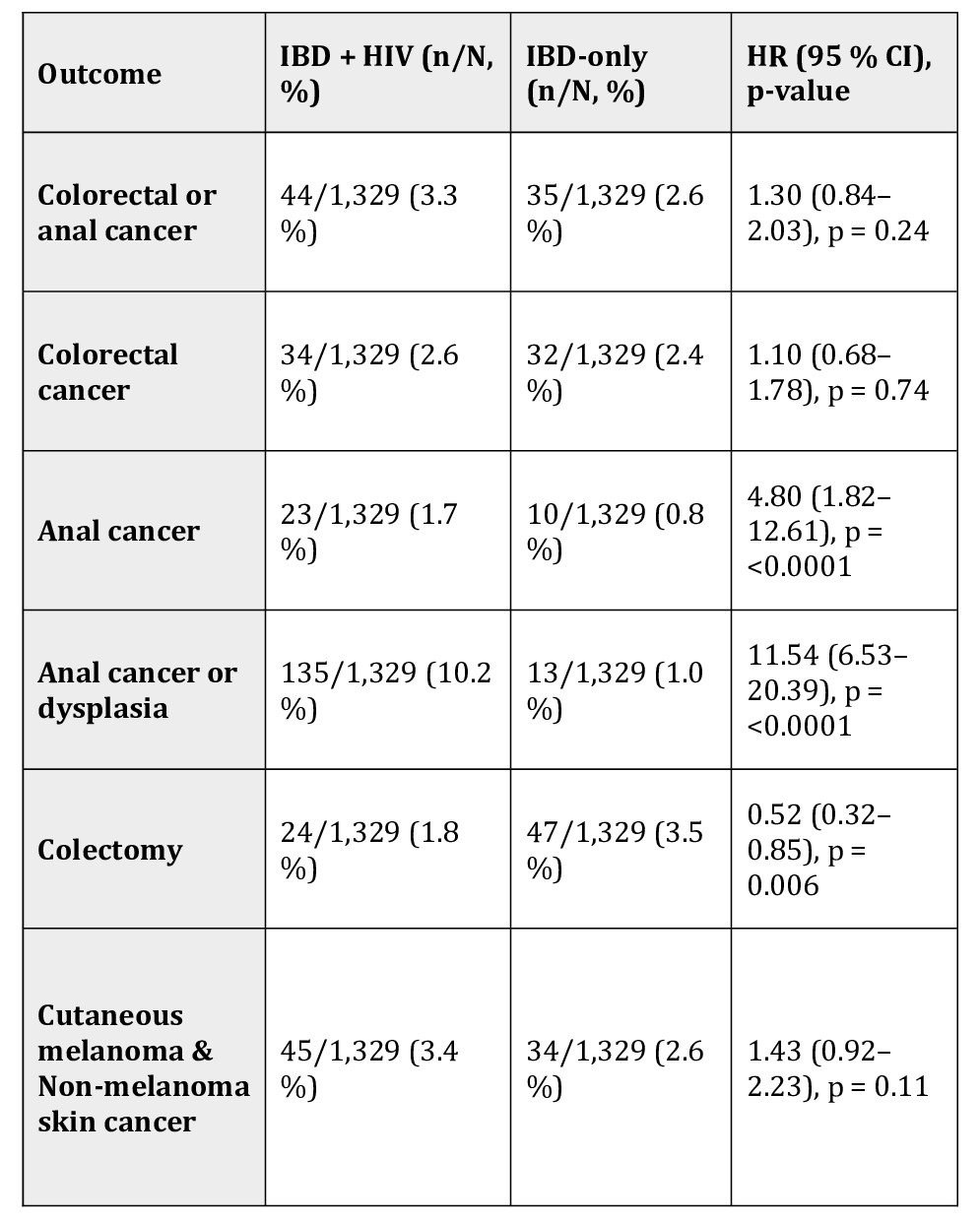
Figure: Table 2. Summary of study outcomes
Disclosures:
Mouhand Mohamed indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Jana Hashash: BMS – Ad Board.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Mouhand Mohamed, MBBS, MS1, Osama Hamid, MD2, Azizullah Beran, MD3, Jana G. Hashash, MD, MSc, FACG4, Victor Chedid, MD, MSc1. P5345 - Human Immunodeficiency Virus Co-infection and Cancer Risk in Inflammatory Bowel Disease: Results From a Large National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Indiana University School of Medicine, Indianapolis, IN; 4Mayo Clinic, Jacksonville, FL
Introduction: Recent data suggest that inflammatory bowel disease (IBD) in people living with HIV (PLWH) often follows a less aggressive course and is managed with fewer advanced therapies. Both HIV infection and IBD independently increase cancer risk, yet it is unclear whether the combined burden further amplifies that risk.
Methods: We queried the U.S. TriNetX collaborative network (comprising >100 million patient records). Using ICD 10 codes, we identified Adults (≥18 y) with ≥3 IBD encounters who received an IBD therapy. We compared IBD in PLWH compared to IBD alone. A propensity score matching (PSM) was performed for age, sex, race, and key comorbidities. Outcomes included risks of colorectal or anal cancer, colorectal cancer alone, anal cancer, anal cancer or dysplasia, colectomy, and risk of skin cancers. Hazard ratios (HR) with corresponding 95% confidence intervals were estimated; P value < 0.05 suggested statistical significance.
Results: After PSM, 1,329 patients were included in each group. The median follow-up duration was 1,425 days in the IBD-HIV cohort, compared to 1,610 days in the controls. HIV co-infection was not associated with higher hazards of combined colorectal or anal cancer (HR 1.30, 95 % CI 0.84–2.03, p = 0.22) or colorectal cancer alone (HR 1.10, 0.68–1.78, p = 0.41). In contrast, anal cancer ( HR 4.80, 1.82–12.61, p = < 0.001) and anal cancer or dysplasia risks (HR 11.54, 6.53–20.39, p = 0.007) were markedly increased. Colectomy occurred less often with HIV (HR 0.52, 0.32–0.85, p = 0.008). Cutaneous melanoma/skin cancer risk did not differ (HR 1.43, 0.92–2.23, p = 0.63).
Discussion: In this large, matched cohort, HIV did not increase colorectal cancer risk in IBD but was strongly associated with anal cancer and anal dysplasia while appearing protective against colectomy. These findings argue for better screening strategies in PLWH with IBD while maintaining standard colorectal dysplasia screening. Prospective studies are needed to clarify the mechanisms underlying these observations and to verify whether the relatively milder IBD course activity in PLWH persists long term. Limitations of this study include the retrospective nature, reliance on ICD codes, and potential for residual confounding. Thus, further research is warranted to validate these findings.
Disclosure: Supervised AI assisted with table generation but not data analysis.
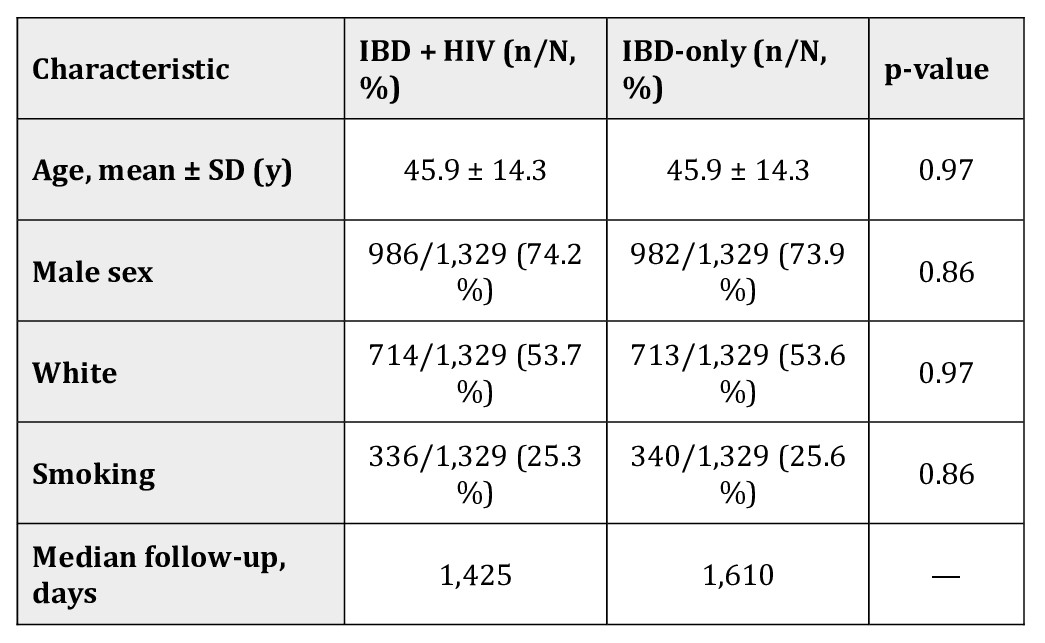
Figure: Table 1. Baseline characteristics after propensity-score matching
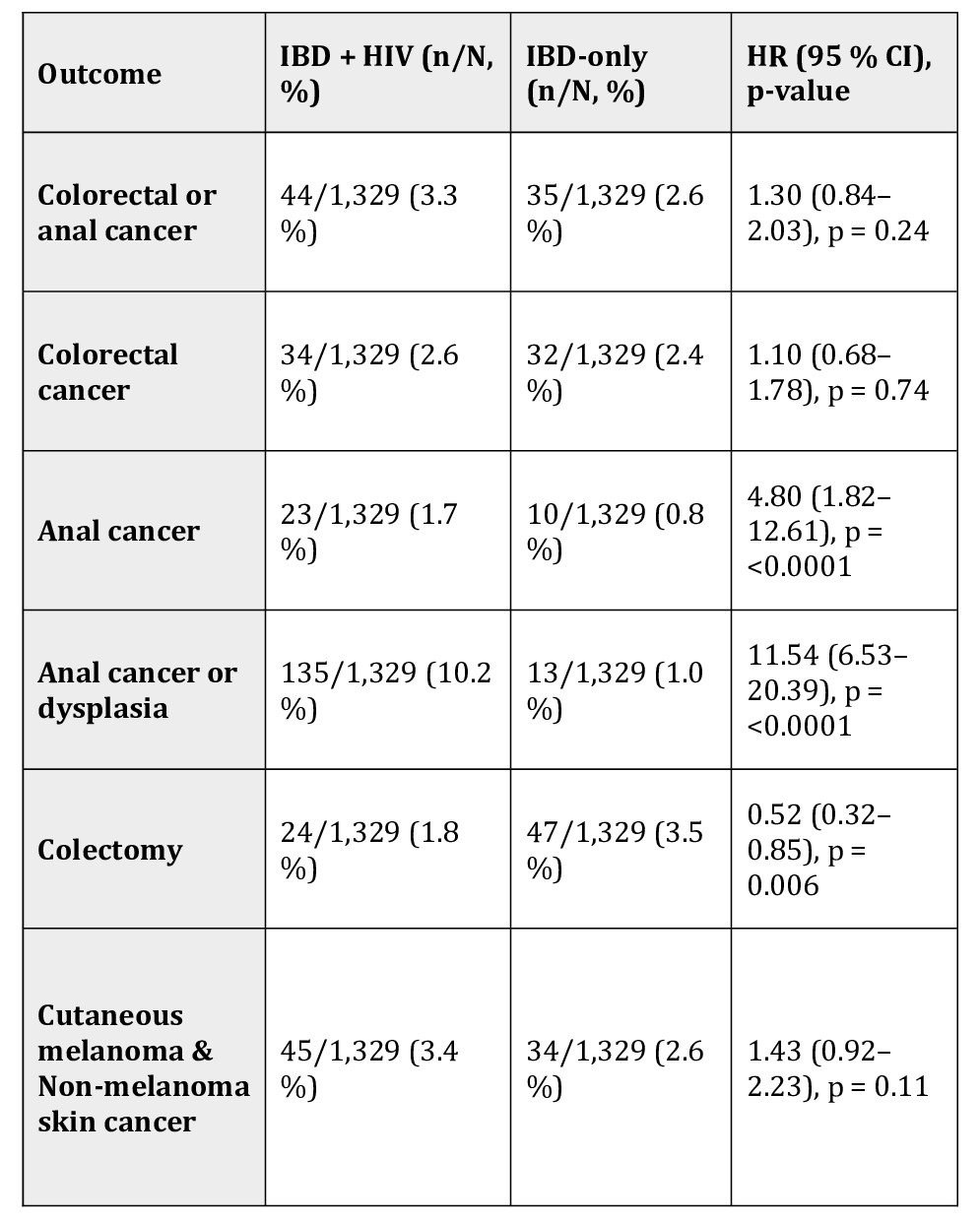
Figure: Table 2. Summary of study outcomes
Disclosures:
Mouhand Mohamed indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Jana Hashash: BMS – Ad Board.
Victor Chedid: Pfizer – Grant/Research Support. Takeda – Consultant.
Mouhand Mohamed, MBBS, MS1, Osama Hamid, MD2, Azizullah Beran, MD3, Jana G. Hashash, MD, MSc, FACG4, Victor Chedid, MD, MSc1. P5345 - Human Immunodeficiency Virus Co-infection and Cancer Risk in Inflammatory Bowel Disease: Results From a Large National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
