Tuesday Poster Session
Category: IBD
P5331 - Effect of Timing of Postoperative Anti-TNF Therapy on Long-Term Outcomes in Crohn’s Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamed Nadeem, MD
Cleveland Clinic Foundation
Fairview Park, OH
Presenting Author(s)
Mohamed Nadeem, MD1, Prabhat Kumar, MD2, Somtochukwu Onwuzo, MD3, Shilpa Junna, MD4, Stephen J. Bickston, MD, FACG5
1Cleveland Clinic Foundation, Fairview Park, OH; 2Virginia Commonwealth University, Richmond, VA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5Virginia Commonwealth University Health System, Richmond, VA
Introduction: Optimal timing for initiation of anti-tumor necrosis factor (TNF) inhibitor therapy after surgery in Crohn’s disease (CD) remains uncertain. Recent data suggest that early initiation of biological therapy post-surgery, as opposed to no biological therapy, may reduce endoscopic recurrence risk and enhance long-term clinical outcomes, including lower hospitalization and repeat surgery rates. This study compares clinical outcomes associated with early (immediately post-surgery) versus late (1-year post-surgery) initiation of anti-TNFs.
Methods: We performed a retrospective cohort analysis using TrinetX database, a global health network. Propensity score matching was used to balance the two cohorts based on comorbidities and prior Crohn’s treatment. Two cohorts, early and late anti-TNF initiation, comprising of 980 patients each were identified. Early anti-TNF initiation is defined as starting anti-TNF immediately after surgery and late anti-TNF initiation is defined as starting at 1 year post bowel surgery. Anti-TNF therapy comprised of infliximab and adalimumab. Primary outcomes included all-cause hospitalization, steroid use (Methylprednisone, prednisone) escalation of Crohn’s therapy either biologics (Ustekinumab, vedolizumab, Risankizumab, mirikizumab, guselkumab) or small molecules (upadacitinib, tofacitinib), repeat bowel surgery, all emergency department (ED) visits 10 years post-surgery. Patients with ulcerative colitis were excluded. Risks, risk differences, odds ratios (OR), and confidence intervals (CI) were calculated.
Results: Early anti-TNF initiation significantly reduced risks of hospitalization (46.7% vs 58.3%; OR 0.63,CI 0.53–0.75; p< 0.001), steroid use (50.4% vs 64.1%; OR 0.57,CI 0.48–0.68; p< 0.001), escalation of Crohn’s therapy (24.3% vs 32.4%; OR 0.67,CI 0.55–0.81; p< 0.001), and ED visits (35.2% vs 48.9%; OR 0.57,CI 0.47–0.68; p< 0.001) compared to late anti-TNF initiation. However, early anti-TNF initiation increased the risk of repeat surgery (33.0% vs 27.8%; OR 1.28, CI 1.06–1.55; p=0.012).
Discussion: Early postoperative initiation of anti-TNF therapy in Crohn’s disease is associated with significantly improved long-term clinical outcomes, including reductions in hospitalizations, steroid use, therapy escalation, and emergency department visits. While a modest increase in repeat surgery rates was observed, the overall benefit supports the early, prophylactic use of anti-TNFs following bowel surgery as a potentially more effective strategy than delayed initiation.
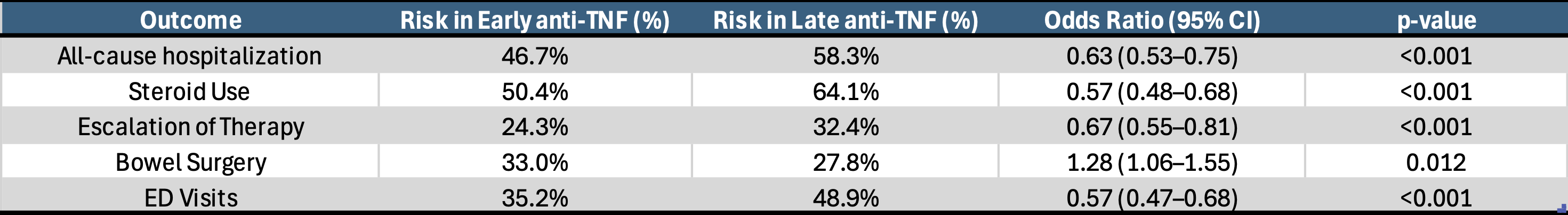
Figure: Table 1. Baseline characteristics of matched cohorts comparing early anti-TNF vs. late anti- TNF initiation following surgery for Crohn's Disease
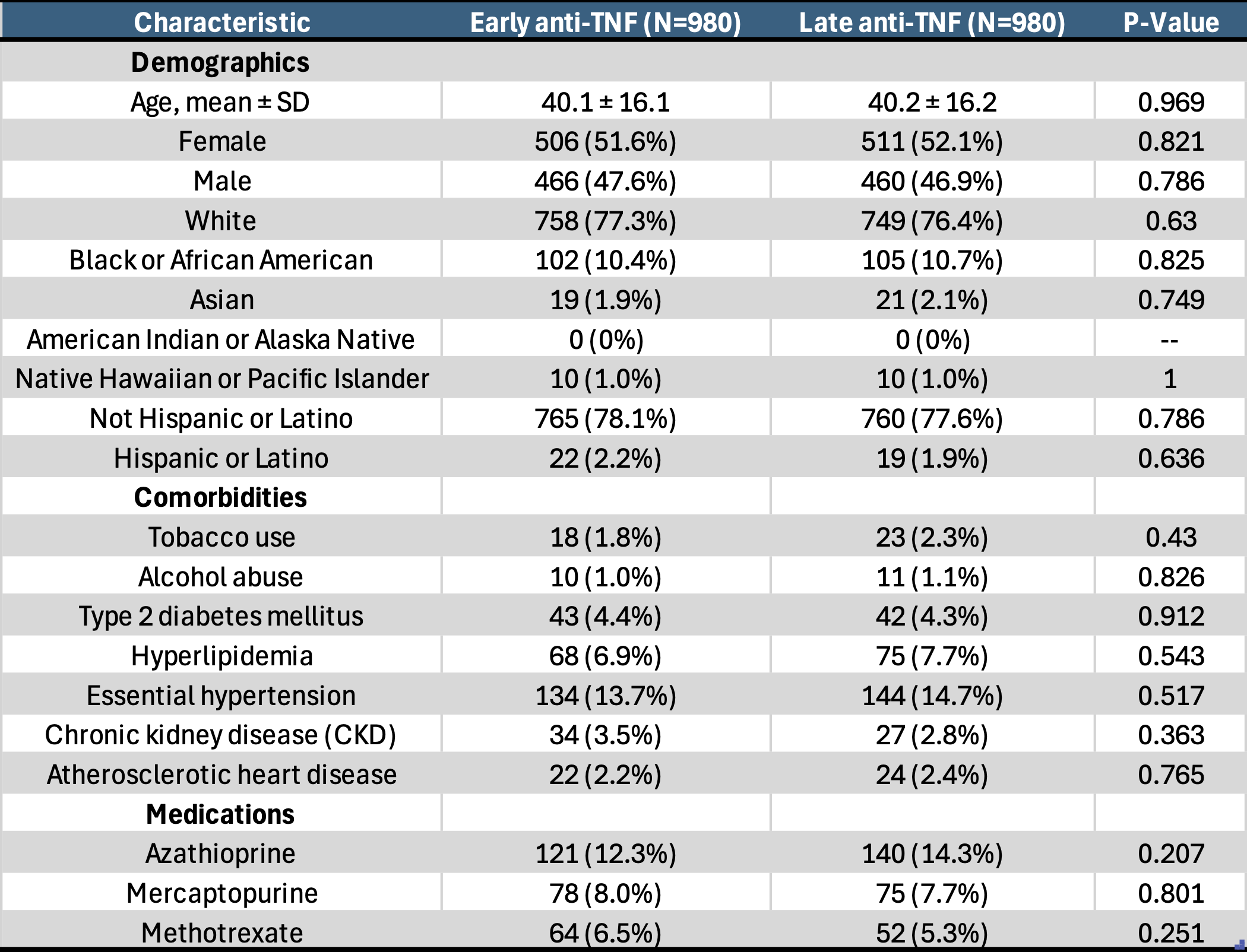
Figure: Table 2. Clinical outcomes comparing early anti-TNF vs. late anti-TNF initiation following surgery for Crohn's Disease
Disclosures:
Mohamed Nadeem indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Shilpa Junna indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Mohamed Nadeem, MD1, Prabhat Kumar, MD2, Somtochukwu Onwuzo, MD3, Shilpa Junna, MD4, Stephen J. Bickston, MD, FACG5. P5331 - Effect of Timing of Postoperative Anti-TNF Therapy on Long-Term Outcomes in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Foundation, Fairview Park, OH; 2Virginia Commonwealth University, Richmond, VA; 3Allegheny Center for Digestive Health, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5Virginia Commonwealth University Health System, Richmond, VA
Introduction: Optimal timing for initiation of anti-tumor necrosis factor (TNF) inhibitor therapy after surgery in Crohn’s disease (CD) remains uncertain. Recent data suggest that early initiation of biological therapy post-surgery, as opposed to no biological therapy, may reduce endoscopic recurrence risk and enhance long-term clinical outcomes, including lower hospitalization and repeat surgery rates. This study compares clinical outcomes associated with early (immediately post-surgery) versus late (1-year post-surgery) initiation of anti-TNFs.
Methods: We performed a retrospective cohort analysis using TrinetX database, a global health network. Propensity score matching was used to balance the two cohorts based on comorbidities and prior Crohn’s treatment. Two cohorts, early and late anti-TNF initiation, comprising of 980 patients each were identified. Early anti-TNF initiation is defined as starting anti-TNF immediately after surgery and late anti-TNF initiation is defined as starting at 1 year post bowel surgery. Anti-TNF therapy comprised of infliximab and adalimumab. Primary outcomes included all-cause hospitalization, steroid use (Methylprednisone, prednisone) escalation of Crohn’s therapy either biologics (Ustekinumab, vedolizumab, Risankizumab, mirikizumab, guselkumab) or small molecules (upadacitinib, tofacitinib), repeat bowel surgery, all emergency department (ED) visits 10 years post-surgery. Patients with ulcerative colitis were excluded. Risks, risk differences, odds ratios (OR), and confidence intervals (CI) were calculated.
Results: Early anti-TNF initiation significantly reduced risks of hospitalization (46.7% vs 58.3%; OR 0.63,CI 0.53–0.75; p< 0.001), steroid use (50.4% vs 64.1%; OR 0.57,CI 0.48–0.68; p< 0.001), escalation of Crohn’s therapy (24.3% vs 32.4%; OR 0.67,CI 0.55–0.81; p< 0.001), and ED visits (35.2% vs 48.9%; OR 0.57,CI 0.47–0.68; p< 0.001) compared to late anti-TNF initiation. However, early anti-TNF initiation increased the risk of repeat surgery (33.0% vs 27.8%; OR 1.28, CI 1.06–1.55; p=0.012).
Discussion: Early postoperative initiation of anti-TNF therapy in Crohn’s disease is associated with significantly improved long-term clinical outcomes, including reductions in hospitalizations, steroid use, therapy escalation, and emergency department visits. While a modest increase in repeat surgery rates was observed, the overall benefit supports the early, prophylactic use of anti-TNFs following bowel surgery as a potentially more effective strategy than delayed initiation.
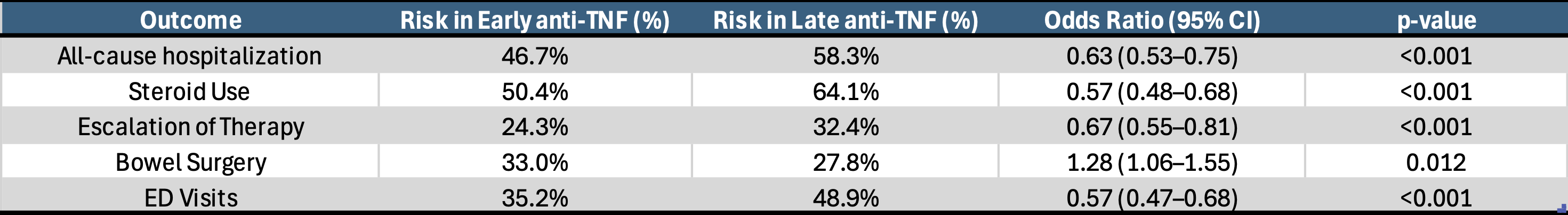
Figure: Table 1. Baseline characteristics of matched cohorts comparing early anti-TNF vs. late anti- TNF initiation following surgery for Crohn's Disease
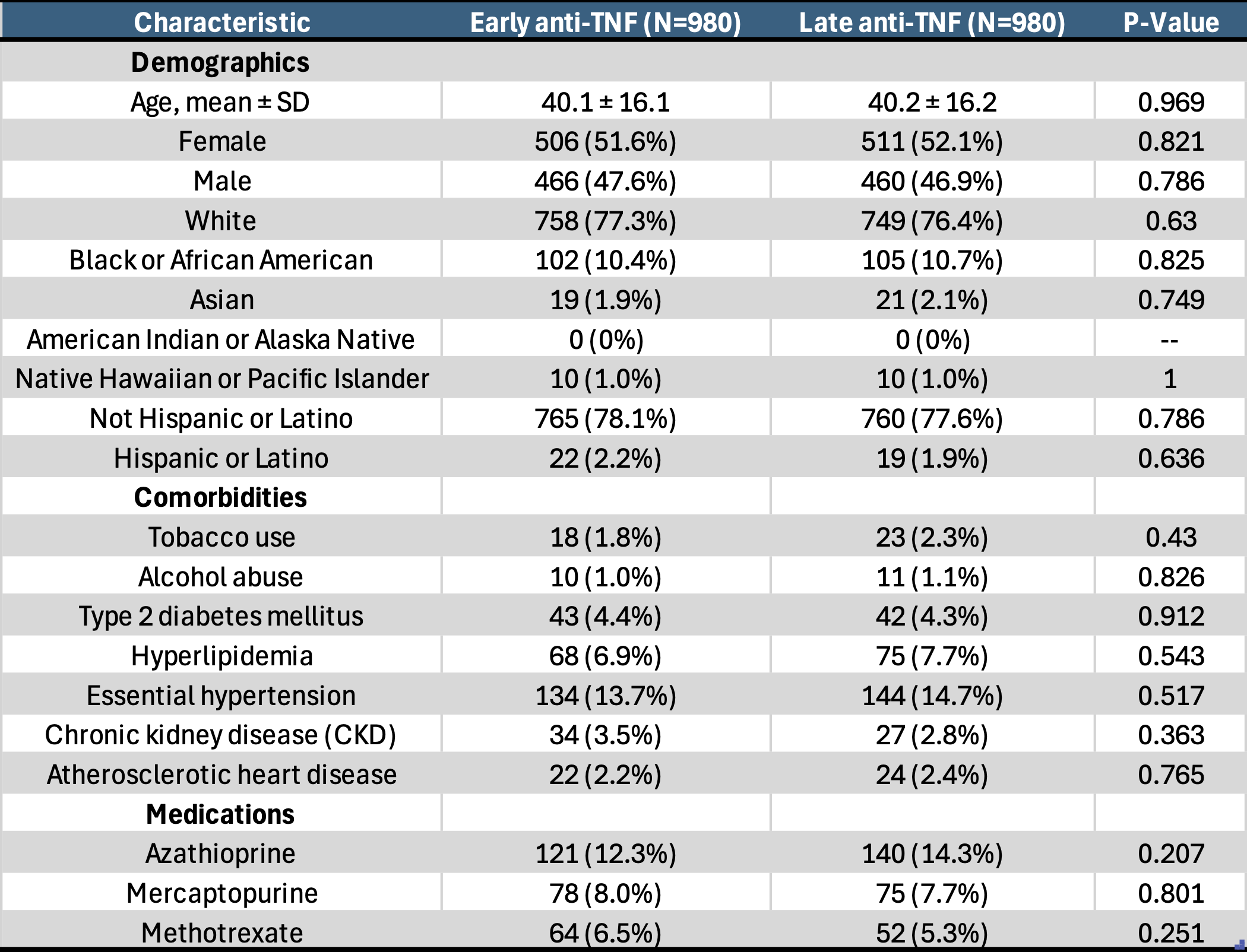
Figure: Table 2. Clinical outcomes comparing early anti-TNF vs. late anti-TNF initiation following surgery for Crohn's Disease
Disclosures:
Mohamed Nadeem indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Shilpa Junna indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Mohamed Nadeem, MD1, Prabhat Kumar, MD2, Somtochukwu Onwuzo, MD3, Shilpa Junna, MD4, Stephen J. Bickston, MD, FACG5. P5331 - Effect of Timing of Postoperative Anti-TNF Therapy on Long-Term Outcomes in Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
