Tuesday Poster Session
Category: IBD
P5423 - Does One Precede the Other? Clinical Course of Patients With Concomitant Eosinophilic Esophagitis and Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Teskey Garrett, DO
Scripps Mercy Hospital
Yorba Linda, CA
Presenting Author(s)
Garrett Teskey, DO1, Collin Mayemura, MD2, Evan Wilder, MD3, Leah Puglisi, MS4, Gauree Konijeti, MD, MPH, FACG5, Quan Nhu, MD, PhD6, Mazer Ally, MD7
1Scripps Mercy Hospital, Yorba Linda, CA; 2Scripps Green Hospital, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA; 4Scripps Clinic, San Diego, CA; 5Scripps Clinic Medical Group, La Jolla, CA; 6Scripps Clinic & Scripps Research Institute, La Jolla, CA; 7Scripps Clinic Medical Group, San Diego, CA
Introduction: Eosinophilic esophagitis (EoE) and inflammatory bowel disease (IBD) are chronic immune-mediated conditions that may co-occur, suggesting a possible shared underlying pathophysiologic mechanism. A few studies have explored the potential temporal relationship between these conditions, however, the factors influencing their sequence remain poorly characterized. This study aims to describe the clinical course of patients diagnosed with both EoE and IBD, focusing on diagnosis order, time interval, and potential demographic and clinical modifiers.
Methods: We conducted a retrospective chart review across our healthcare system from 1/1/2010 to 4/1/2023 for patients with EoE and IBD. Inclusion criteria required confirmed diagnoses of both conditions via endoscopy and histology. The primary outcomes included the predominant order of diagnosis (EoE first, IBD first, or simultaneous) and the average time interval between diagnoses. Secondary outcomes assessed associations between diagnosis timing and factors including age, sex, IBD subtype, and presence of concomitant conditions.
Results: 27 patients were identified to have both EoE and IBD. The predominant sequence was IBD diagnosed prior to EoE (77.8%, n=21), followed by EoE preceding IBD (14.8%, n=4), and simultaneous diagnosis (7.4%, n=2). The mean time interval between diagnoses was 10 (+/- 9.4yrs) years. Median age at first diagnosis was 30 (SD +/- 17). 72% of our cohort was male and 92% White.
Endoscopic findings commonly observed at EoE diagnosis included furrows (63%), edema (52%), and rings (41%). Among IBD subtypes, 37% had Ulcerative Colitis, 40% had Crohn’s disease, 18.5% with microscopic colitis and 3.7% with Indeterminate Colitis. Sex, IBD subtype, and atopic history did not show significant differences in time to secondary diagnosis, though slight trends were observed. Treatment patterns showed frequent use of aminosalicylates, anti-TNF agents, dietary therapy, and proton pump inhibitors. 29% required esophageal dilation or experienced treatment resistance, indicating severe disease burden.
Discussion: This descriptive analysis highlights IBD as the more common initial diagnosis and emphasizes the long diagnostic latency between IBD and EoE. Endoscopic features and comorbidity profiles suggest possible shared immune dysregulation. Recognition of temporal patterns and associated features may aid early detection and personalized management in patients with coexisting IBD and EoE.
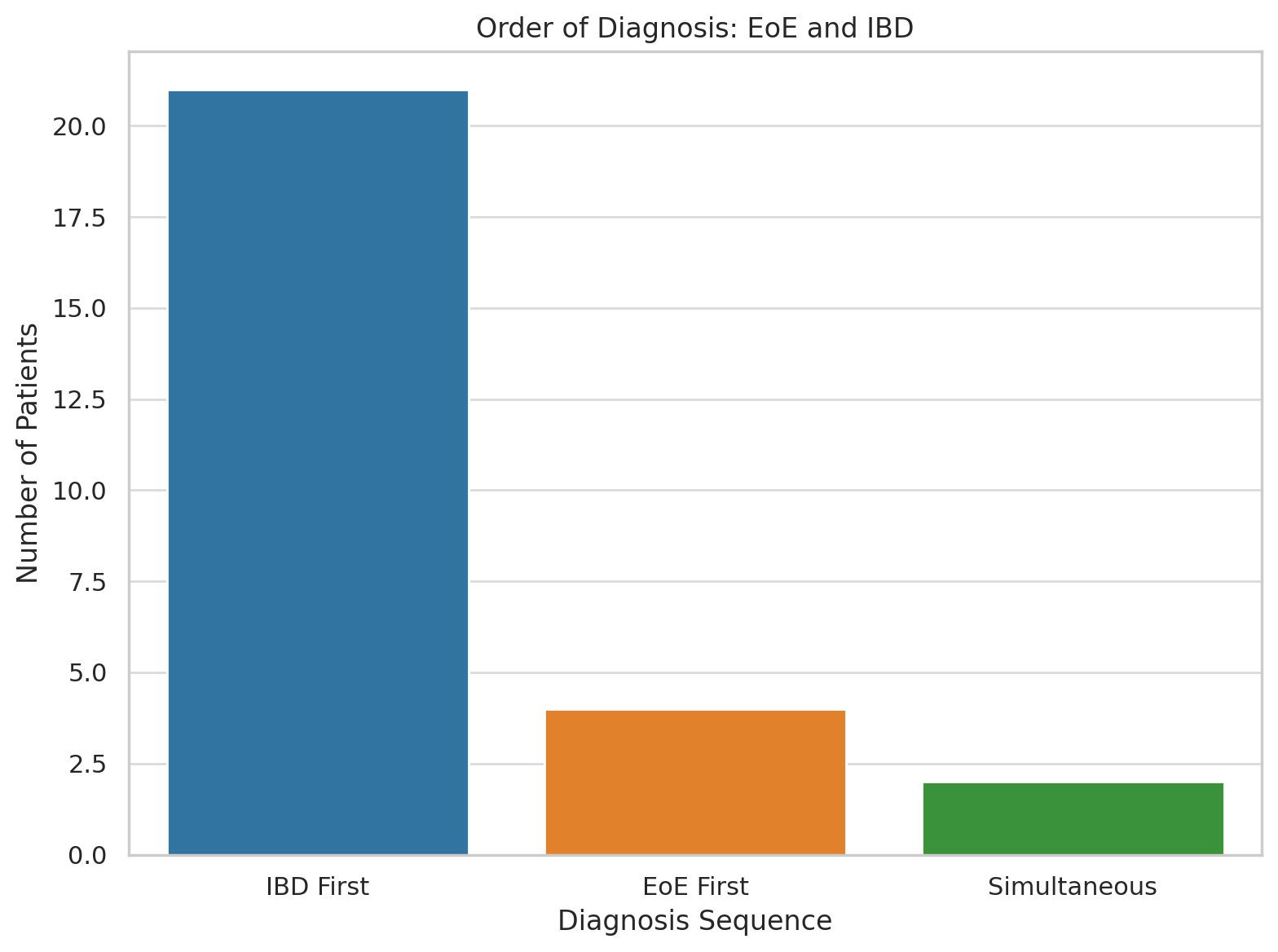
Figure: Order of diagnosis
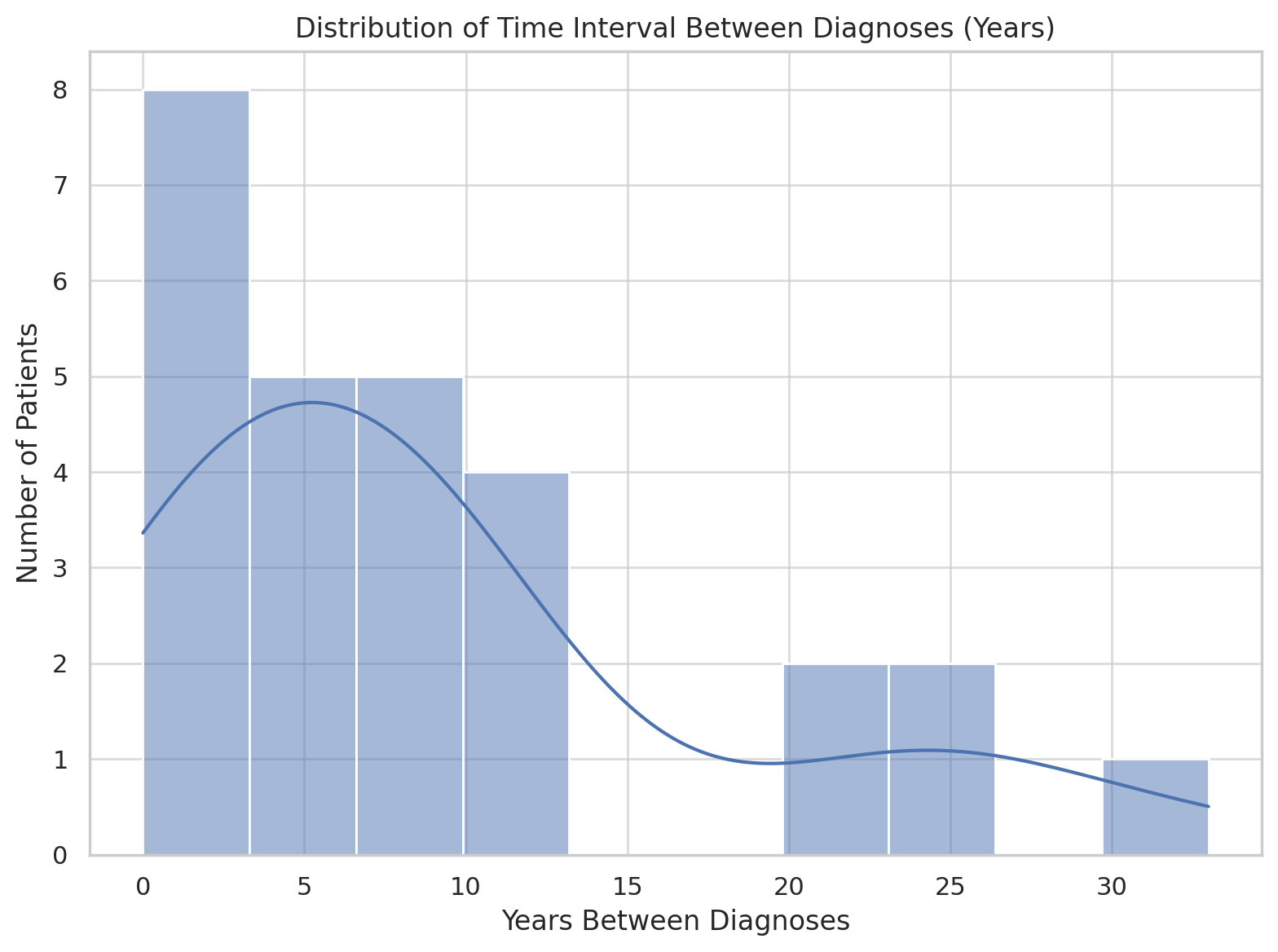
Figure: Distribution of time interval between diagnoses in years
Disclosures:
Garrett Teskey indicated no relevant financial relationships.
Collin Mayemura indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Leah Puglisi indicated no relevant financial relationships.
Gauree Konijeti: Abbvie – Advisory Committee/Board Member, Consultant. Johnson and Johnson – Consultant. Lilly – Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member. Takeda – Speakers Bureau. WellTheory – Consultant, Stock Options.
Quan Nhu: Regeneron – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Mazer Ally: Abbvie – Speakers Bureau. Lilly – Advisory Committee/Board Member.
Garrett Teskey, DO1, Collin Mayemura, MD2, Evan Wilder, MD3, Leah Puglisi, MS4, Gauree Konijeti, MD, MPH, FACG5, Quan Nhu, MD, PhD6, Mazer Ally, MD7. P5423 - Does One Precede the Other? Clinical Course of Patients With Concomitant Eosinophilic Esophagitis and Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Scripps Mercy Hospital, Yorba Linda, CA; 2Scripps Green Hospital, San Diego, CA; 3Scripps Green Hospital, La Jolla, CA; 4Scripps Clinic, San Diego, CA; 5Scripps Clinic Medical Group, La Jolla, CA; 6Scripps Clinic & Scripps Research Institute, La Jolla, CA; 7Scripps Clinic Medical Group, San Diego, CA
Introduction: Eosinophilic esophagitis (EoE) and inflammatory bowel disease (IBD) are chronic immune-mediated conditions that may co-occur, suggesting a possible shared underlying pathophysiologic mechanism. A few studies have explored the potential temporal relationship between these conditions, however, the factors influencing their sequence remain poorly characterized. This study aims to describe the clinical course of patients diagnosed with both EoE and IBD, focusing on diagnosis order, time interval, and potential demographic and clinical modifiers.
Methods: We conducted a retrospective chart review across our healthcare system from 1/1/2010 to 4/1/2023 for patients with EoE and IBD. Inclusion criteria required confirmed diagnoses of both conditions via endoscopy and histology. The primary outcomes included the predominant order of diagnosis (EoE first, IBD first, or simultaneous) and the average time interval between diagnoses. Secondary outcomes assessed associations between diagnosis timing and factors including age, sex, IBD subtype, and presence of concomitant conditions.
Results: 27 patients were identified to have both EoE and IBD. The predominant sequence was IBD diagnosed prior to EoE (77.8%, n=21), followed by EoE preceding IBD (14.8%, n=4), and simultaneous diagnosis (7.4%, n=2). The mean time interval between diagnoses was 10 (+/- 9.4yrs) years. Median age at first diagnosis was 30 (SD +/- 17). 72% of our cohort was male and 92% White.
Endoscopic findings commonly observed at EoE diagnosis included furrows (63%), edema (52%), and rings (41%). Among IBD subtypes, 37% had Ulcerative Colitis, 40% had Crohn’s disease, 18.5% with microscopic colitis and 3.7% with Indeterminate Colitis. Sex, IBD subtype, and atopic history did not show significant differences in time to secondary diagnosis, though slight trends were observed. Treatment patterns showed frequent use of aminosalicylates, anti-TNF agents, dietary therapy, and proton pump inhibitors. 29% required esophageal dilation or experienced treatment resistance, indicating severe disease burden.
Discussion: This descriptive analysis highlights IBD as the more common initial diagnosis and emphasizes the long diagnostic latency between IBD and EoE. Endoscopic features and comorbidity profiles suggest possible shared immune dysregulation. Recognition of temporal patterns and associated features may aid early detection and personalized management in patients with coexisting IBD and EoE.
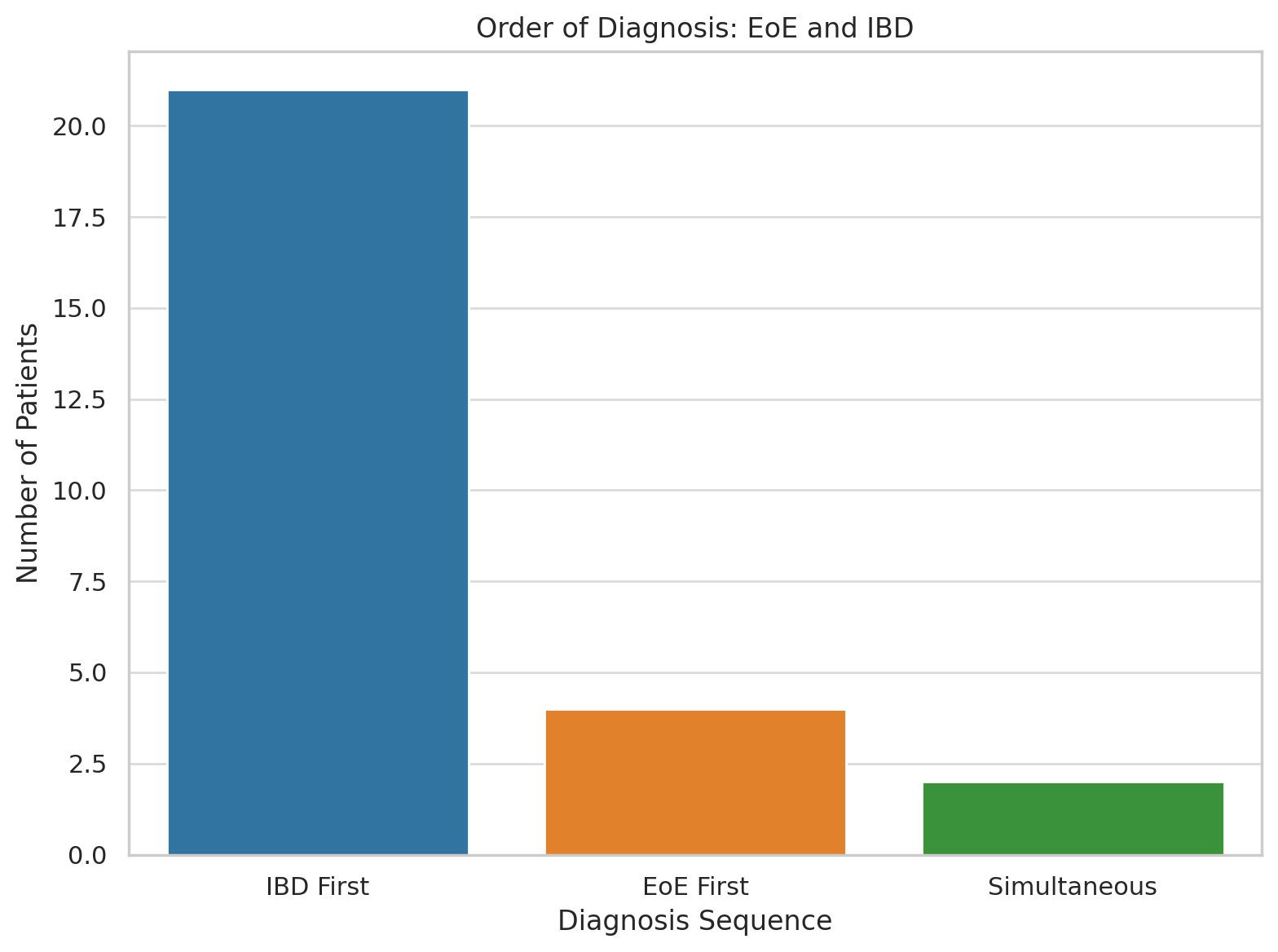
Figure: Order of diagnosis
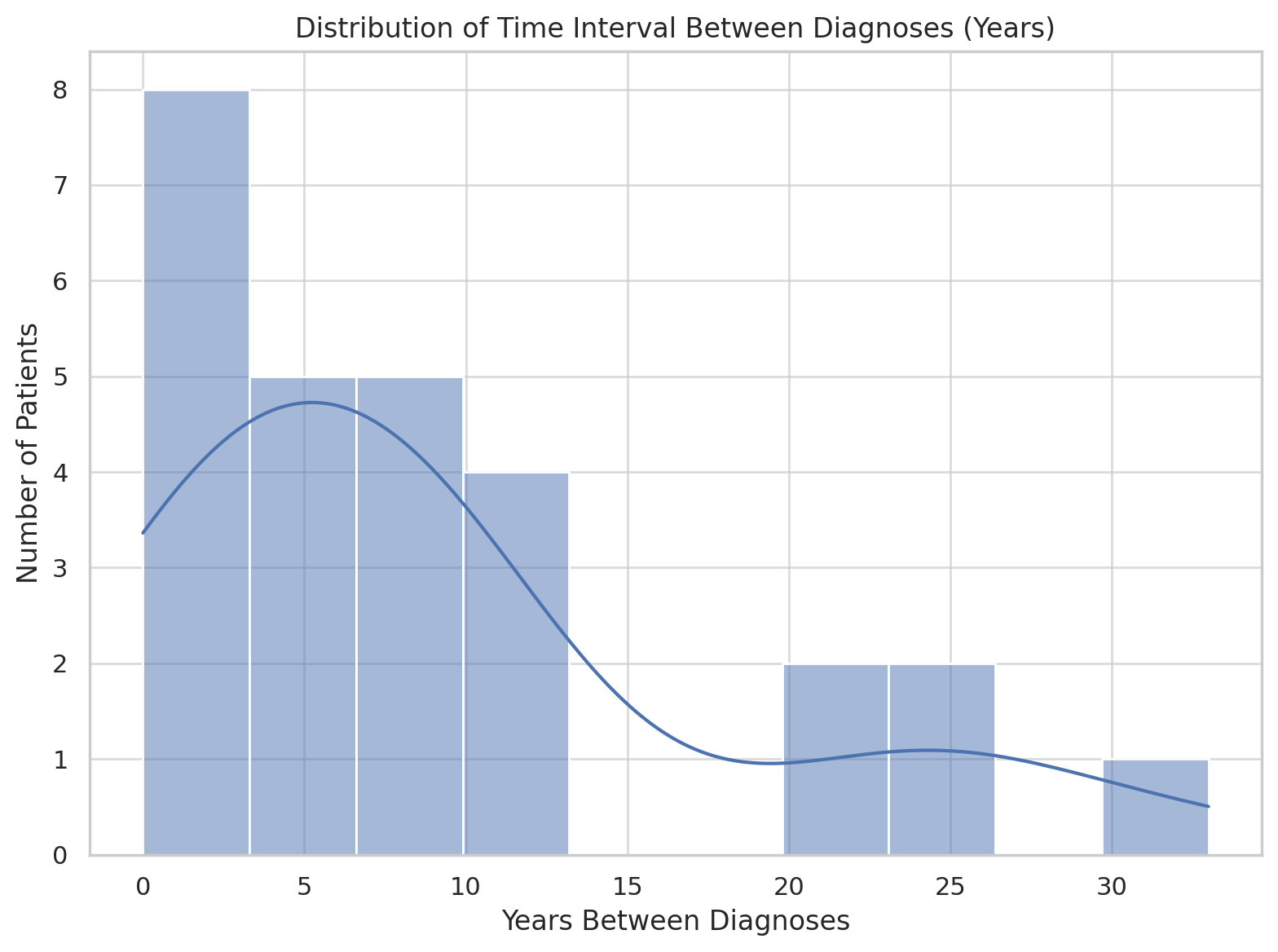
Figure: Distribution of time interval between diagnoses in years
Disclosures:
Garrett Teskey indicated no relevant financial relationships.
Collin Mayemura indicated no relevant financial relationships.
Evan Wilder indicated no relevant financial relationships.
Leah Puglisi indicated no relevant financial relationships.
Gauree Konijeti: Abbvie – Advisory Committee/Board Member, Consultant. Johnson and Johnson – Consultant. Lilly – Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member. Takeda – Speakers Bureau. WellTheory – Consultant, Stock Options.
Quan Nhu: Regeneron – Advisory Committee/Board Member, Consultant, Speakers Bureau. Sanofi – Advisory Committee/Board Member, Speakers Bureau. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Mazer Ally: Abbvie – Speakers Bureau. Lilly – Advisory Committee/Board Member.
Garrett Teskey, DO1, Collin Mayemura, MD2, Evan Wilder, MD3, Leah Puglisi, MS4, Gauree Konijeti, MD, MPH, FACG5, Quan Nhu, MD, PhD6, Mazer Ally, MD7. P5423 - Does One Precede the Other? Clinical Course of Patients With Concomitant Eosinophilic Esophagitis and Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
