Tuesday Poster Session
Category: IBD
P5420 - Tobacco Use Predicts Disease Behavior and Localization in Perianal Fistulizing Crohn’s Disease: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Isha Bhutada, MD (she/her/hers)
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Isha Bhutada, MD, Seth Bergenholtz, MD, Serre-Yu Wong, MD, PhD, Elijah Li, MD
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Although tobacco use is a well-recognized risk factor for severe Crohn’s disease (CD) phenotypes, its impact on patients with perianal fistulizing CD (PFCD) remains incompletely defined. This study aims to assess the relationship between tobacco use and disease behavior, localization, and outcomes in patients with PFCD.
Methods: We identified 182 CD patients from a quaternary care center, diagnosed with PFCD between 2005-2025. Demographics, disease features, and healthcare use data after CD diagnosis were collected via retrospective chart review. Univariate and multivariate regression models were used, adjusted for age, gender, and time observed. Disease course 1 year after diagnosis was classified as remission (no further abscess or drainage), continuous drainage (light and heavy) or ≥2 distinct flares.
Results: Mean participant age was 30.4 (SD 11.36). Of the subjects, 58.2% (n=106) were male, 68.7% (n=125) never smoked, 22.5% (n=41) formerly smoked and 8.8% (n=16) currently smoked. 95.6% (n=174) used biologics and 68% (n=123) used immunomodulators. Mean ED visits were 1.66 (SD 2.36), exams under anesthesia (EUA) 2.98 (SD 2.6), and proctectomies/diversions 1.31 (SD 0.784). Within 1 year of PAF diagnosis, 19.2% (n=35) achieved remission, 6.6% (n=12) had light drainage, 19.8% (n=10) had heavy drainage, and 48.9% (n=89) had flares. Disease localized to L1 in 22.2% (n=40), L2 in 28.1% (n=53), and L3 in 47.8% (n=87).
Univariate analysis showed an association between tobacco use and location (p=0.009), course (p=0.043) and diversions/proctectomies (p=0.011) (Table 1). In multivariate analysis, patients with tobacco exposure were more likely to have L2 over L1 disease (OR 4.31; CI 1.42–14.23; p=0.010). In year 1, smokers were likely to have ≥2 flares over remission (OR 3.56; CI 1.24–10.19; p=0.018). Active smokers exceeded the average number of EUA (OR 4.15; CI 1.39 – 12.4, p=0.010), had 1.27 more ED visits (p=0.047), and had 0.42 more diversions/proctectomies (p=0.048) than never-smokers (Table 2).
Discussion: This study shows that tobacco exposure was associated with L2 disease in our PFCD cohort, contrasting prior studies linking smoking to L1 and L3 in the general CD population. PFCD patients with tobacco exposure were more likely to have perianal disease flares in the first year, increased healthcare use and need for diversion surgery. Our findings support prior evidence linking smoking to complicated CD and highlight its role in risk stratification and expectant management of PFCD.
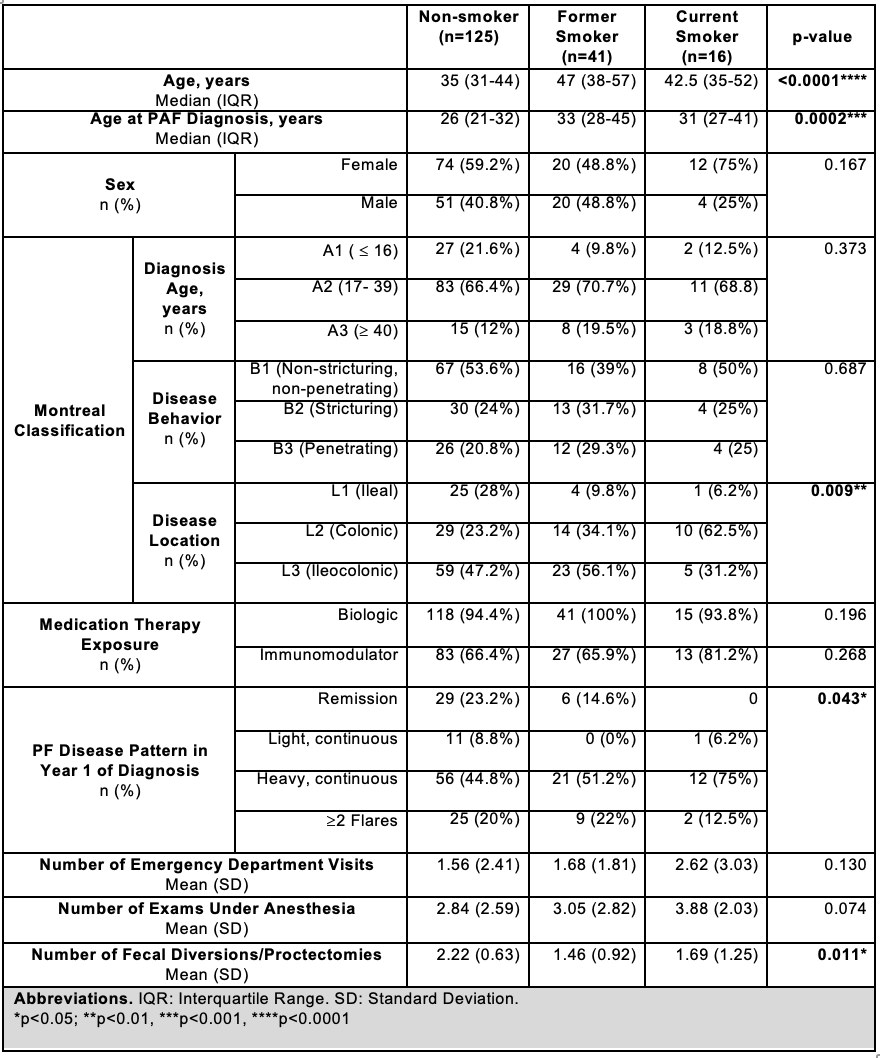
Figure: Table 1. Univariate Analyses of Participant Characteristics and CD History with Tobacco Use Status
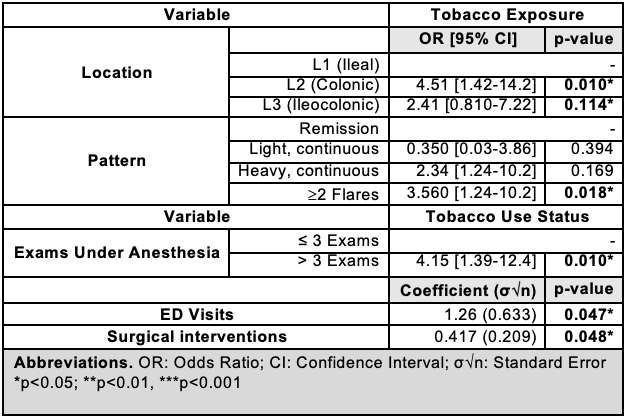
Figure: Table 2. Multivariate Analyses of CD and PAF History with Tobacco Use Status, Controlled for Age, Gender, and Observation Period
Disclosures:
Isha Bhutada indicated no relevant financial relationships.
Seth Bergenholtz indicated no relevant financial relationships.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Elijah Li indicated no relevant financial relationships.
Isha Bhutada, MD, Seth Bergenholtz, MD, Serre-Yu Wong, MD, PhD, Elijah Li, MD. P5420 - Tobacco Use Predicts Disease Behavior and Localization in Perianal Fistulizing Crohn’s Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Although tobacco use is a well-recognized risk factor for severe Crohn’s disease (CD) phenotypes, its impact on patients with perianal fistulizing CD (PFCD) remains incompletely defined. This study aims to assess the relationship between tobacco use and disease behavior, localization, and outcomes in patients with PFCD.
Methods: We identified 182 CD patients from a quaternary care center, diagnosed with PFCD between 2005-2025. Demographics, disease features, and healthcare use data after CD diagnosis were collected via retrospective chart review. Univariate and multivariate regression models were used, adjusted for age, gender, and time observed. Disease course 1 year after diagnosis was classified as remission (no further abscess or drainage), continuous drainage (light and heavy) or ≥2 distinct flares.
Results: Mean participant age was 30.4 (SD 11.36). Of the subjects, 58.2% (n=106) were male, 68.7% (n=125) never smoked, 22.5% (n=41) formerly smoked and 8.8% (n=16) currently smoked. 95.6% (n=174) used biologics and 68% (n=123) used immunomodulators. Mean ED visits were 1.66 (SD 2.36), exams under anesthesia (EUA) 2.98 (SD 2.6), and proctectomies/diversions 1.31 (SD 0.784). Within 1 year of PAF diagnosis, 19.2% (n=35) achieved remission, 6.6% (n=12) had light drainage, 19.8% (n=10) had heavy drainage, and 48.9% (n=89) had flares. Disease localized to L1 in 22.2% (n=40), L2 in 28.1% (n=53), and L3 in 47.8% (n=87).
Univariate analysis showed an association between tobacco use and location (p=0.009), course (p=0.043) and diversions/proctectomies (p=0.011) (Table 1). In multivariate analysis, patients with tobacco exposure were more likely to have L2 over L1 disease (OR 4.31; CI 1.42–14.23; p=0.010). In year 1, smokers were likely to have ≥2 flares over remission (OR 3.56; CI 1.24–10.19; p=0.018). Active smokers exceeded the average number of EUA (OR 4.15; CI 1.39 – 12.4, p=0.010), had 1.27 more ED visits (p=0.047), and had 0.42 more diversions/proctectomies (p=0.048) than never-smokers (Table 2).
Discussion: This study shows that tobacco exposure was associated with L2 disease in our PFCD cohort, contrasting prior studies linking smoking to L1 and L3 in the general CD population. PFCD patients with tobacco exposure were more likely to have perianal disease flares in the first year, increased healthcare use and need for diversion surgery. Our findings support prior evidence linking smoking to complicated CD and highlight its role in risk stratification and expectant management of PFCD.
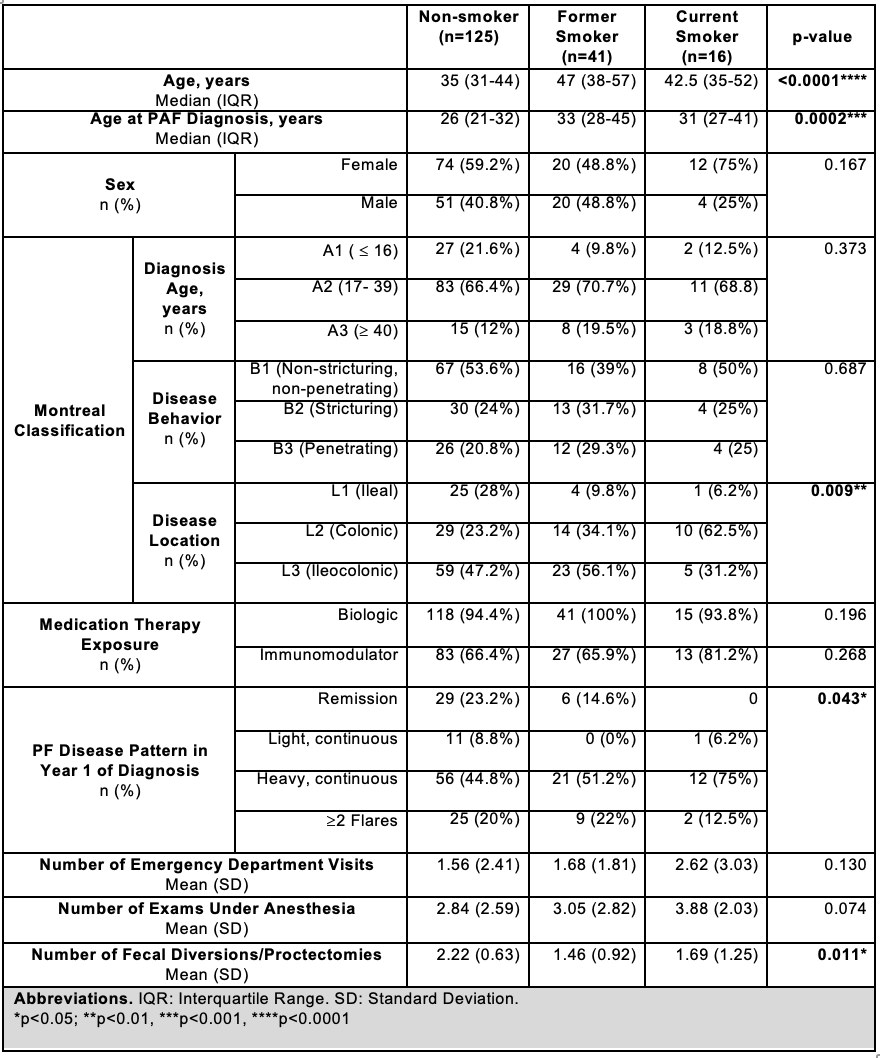
Figure: Table 1. Univariate Analyses of Participant Characteristics and CD History with Tobacco Use Status
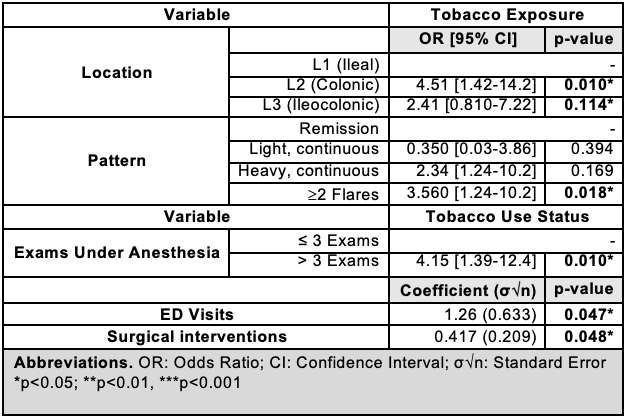
Figure: Table 2. Multivariate Analyses of CD and PAF History with Tobacco Use Status, Controlled for Age, Gender, and Observation Period
Disclosures:
Isha Bhutada indicated no relevant financial relationships.
Seth Bergenholtz indicated no relevant financial relationships.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Elijah Li indicated no relevant financial relationships.
Isha Bhutada, MD, Seth Bergenholtz, MD, Serre-Yu Wong, MD, PhD, Elijah Li, MD. P5420 - Tobacco Use Predicts Disease Behavior and Localization in Perianal Fistulizing Crohn’s Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
