Tuesday Poster Session
Category: IBD
P5418 - Therapeutic Potential of Statins in Inflammatory Bowel Disease Flares: A Retrospective Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alvin Boyd Newman-Caro, DO
HCA Healthcare
Clearwater, FL
Presenting Author(s)
Alvin Boyd. Newman-Caro, DO1, Vamsee Mupparaju, MD2, Ivan E. Rascon-Aguilar, MD3, Diego Rascon, 4, Vanessa Florival, MD5
1HCA Healthcare, Bradenton, FL; 2HCA Florida Citrus Hospital, Inverness, FL; 3HCA Florida Healthcare, Bradenton, FL; 4University of South Florida, Bradenton, FL; 5Optum Healthcare, Bradenton, FL
Introduction: There is evidence that statin use decreases the incidence of inflammatory bowel disease, but research investigating statins’ impact on reducing the rate of flares is lacking. We aimed to investigate the therapeutic benefit of statins in the treatment of inflammatory bowel disease flares.
Methods: In this retrospective study conducted across 16 HCA Hospitals, we focused on adult patients ( > 18 years-of-age) previously diagnosed with inflammatory bowel disease (IBD) who were admitted for IBD flare between January 1, 2019, and December 31, 2022. The outcome variables of interest were the length of hospital stay and the incidence of hemicolectomy. Predictor variables included statin use (classified as users vs. non-users) and statin dosage. Regression was used to determine the associations between predictor and outcome variables, including comparisons between statin users and non-users and among different statin dosage groups.
Results: Most patients were not on statins (n = 17,043, 86.9%), with a small proportion on Low (275, 1.4%), Medium (1270, 6.5%), or High (1014, 5.2%) statin doses (Table 1). Among patients with IBD, the odds of having a hemicolectomy were 1.659 times as likely for low dose statin patients than for non-statin patients (p-value=0.0013, 95% Cl: 1.220-2.256) (Table 2). Additionally, among patients with IBD, statin dose was significantly predictive of log count of hospital days, with high-, medium-, and low-dose statins increasing the count of days by factors of 1.246 (95% CI: 1.140-1.364, p< .0001), 1.170 (95% CI: 1.077-1.271, p=0.0002), and 1.339 (95% CI: 1.141-1.571, p=0.0004), respectively, compared to no statin use (Table 3).
Discussion: Statins have anti-inflammatory and antifibrotic effects, reducing proinflammatory markers like CRP, interferon-gamma, IL-6, IL-8, and NF-kappa B - key drivers of inflammation in UC and Crohn’s. However, among IBD patients admitted for disease flare, those taking statins had longer hospital stays compared to those not taking statins. Furthermore, patients on low-dose statins were 1.66 times more likely to undergo hemicolectomy than non-users. These findings suggest that statin therapy does not significantly reduce hospital length of stay or the need for surgical intervention in IBD flares. Instead, they raise concerns about potential adverse outcomes. These findings challenge the presumed benefit of statins in IBD management and highlight the need for further research to understand their effects and refine their therapeutic role.
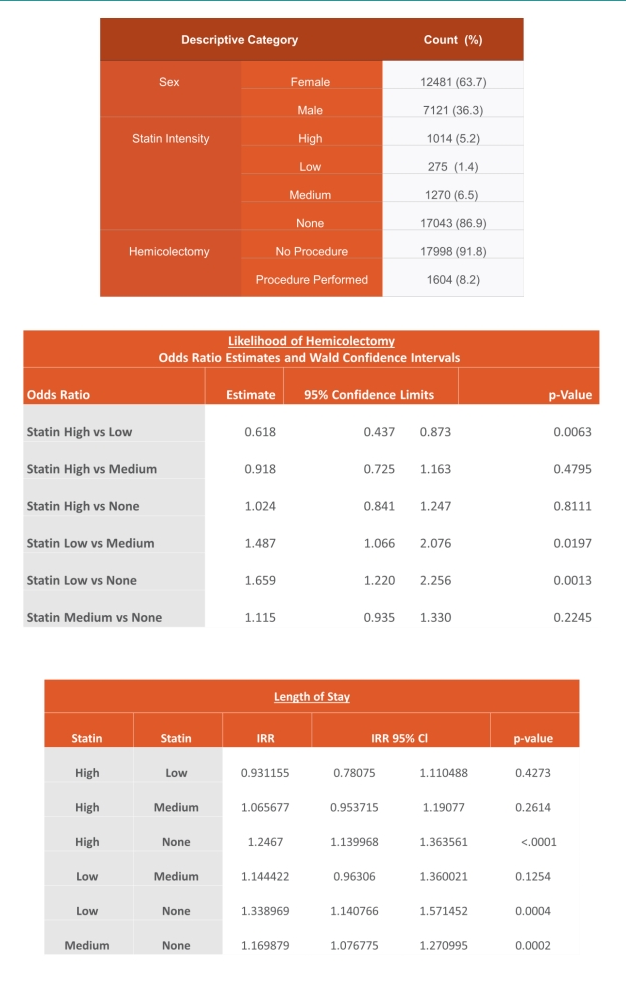
Figure: Table 1: Descriptive Statistics
Table 2: Likelihood of Hemicolectomy (Logistic Regression)
Table 3: Length of Stay (Negative Binomial Regression)
Disclosures:
Alvin Newman-Caro indicated no relevant financial relationships.
Vamsee Mupparaju indicated no relevant financial relationships.
Ivan Rascon-Aguilar indicated no relevant financial relationships.
Diego Rascon indicated no relevant financial relationships.
Vanessa Florival indicated no relevant financial relationships.
Alvin Boyd. Newman-Caro, DO1, Vamsee Mupparaju, MD2, Ivan E. Rascon-Aguilar, MD3, Diego Rascon, 4, Vanessa Florival, MD5. P5418 - Therapeutic Potential of Statins in Inflammatory Bowel Disease Flares: A Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare, Bradenton, FL; 2HCA Florida Citrus Hospital, Inverness, FL; 3HCA Florida Healthcare, Bradenton, FL; 4University of South Florida, Bradenton, FL; 5Optum Healthcare, Bradenton, FL
Introduction: There is evidence that statin use decreases the incidence of inflammatory bowel disease, but research investigating statins’ impact on reducing the rate of flares is lacking. We aimed to investigate the therapeutic benefit of statins in the treatment of inflammatory bowel disease flares.
Methods: In this retrospective study conducted across 16 HCA Hospitals, we focused on adult patients ( > 18 years-of-age) previously diagnosed with inflammatory bowel disease (IBD) who were admitted for IBD flare between January 1, 2019, and December 31, 2022. The outcome variables of interest were the length of hospital stay and the incidence of hemicolectomy. Predictor variables included statin use (classified as users vs. non-users) and statin dosage. Regression was used to determine the associations between predictor and outcome variables, including comparisons between statin users and non-users and among different statin dosage groups.
Results: Most patients were not on statins (n = 17,043, 86.9%), with a small proportion on Low (275, 1.4%), Medium (1270, 6.5%), or High (1014, 5.2%) statin doses (Table 1). Among patients with IBD, the odds of having a hemicolectomy were 1.659 times as likely for low dose statin patients than for non-statin patients (p-value=0.0013, 95% Cl: 1.220-2.256) (Table 2). Additionally, among patients with IBD, statin dose was significantly predictive of log count of hospital days, with high-, medium-, and low-dose statins increasing the count of days by factors of 1.246 (95% CI: 1.140-1.364, p< .0001), 1.170 (95% CI: 1.077-1.271, p=0.0002), and 1.339 (95% CI: 1.141-1.571, p=0.0004), respectively, compared to no statin use (Table 3).
Discussion: Statins have anti-inflammatory and antifibrotic effects, reducing proinflammatory markers like CRP, interferon-gamma, IL-6, IL-8, and NF-kappa B - key drivers of inflammation in UC and Crohn’s. However, among IBD patients admitted for disease flare, those taking statins had longer hospital stays compared to those not taking statins. Furthermore, patients on low-dose statins were 1.66 times more likely to undergo hemicolectomy than non-users. These findings suggest that statin therapy does not significantly reduce hospital length of stay or the need for surgical intervention in IBD flares. Instead, they raise concerns about potential adverse outcomes. These findings challenge the presumed benefit of statins in IBD management and highlight the need for further research to understand their effects and refine their therapeutic role.
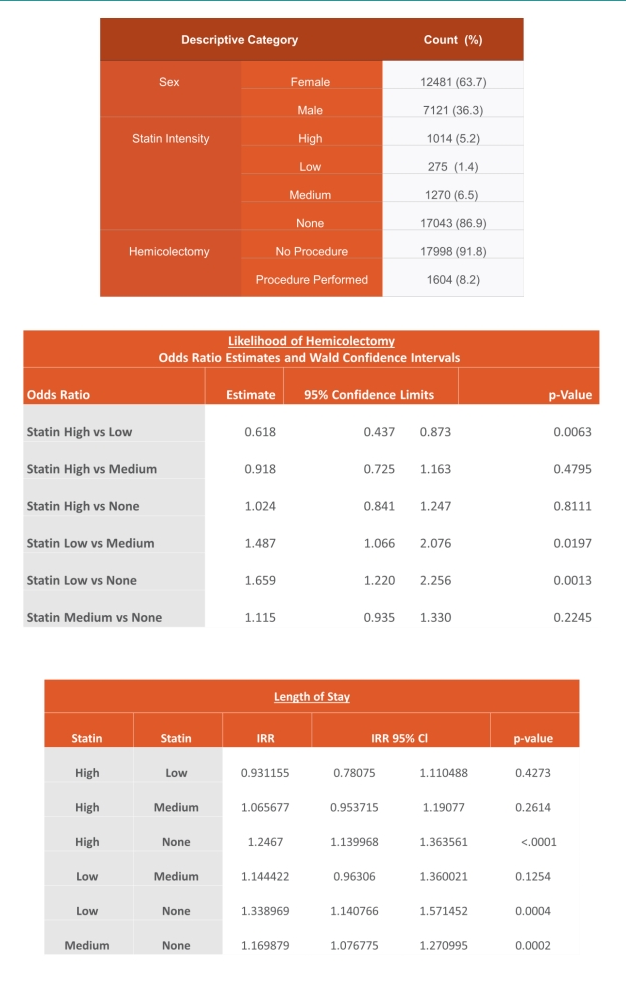
Figure: Table 1: Descriptive Statistics
Table 2: Likelihood of Hemicolectomy (Logistic Regression)
Table 3: Length of Stay (Negative Binomial Regression)
Disclosures:
Alvin Newman-Caro indicated no relevant financial relationships.
Vamsee Mupparaju indicated no relevant financial relationships.
Ivan Rascon-Aguilar indicated no relevant financial relationships.
Diego Rascon indicated no relevant financial relationships.
Vanessa Florival indicated no relevant financial relationships.
Alvin Boyd. Newman-Caro, DO1, Vamsee Mupparaju, MD2, Ivan E. Rascon-Aguilar, MD3, Diego Rascon, 4, Vanessa Florival, MD5. P5418 - Therapeutic Potential of Statins in Inflammatory Bowel Disease Flares: A Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
