Tuesday Poster Session
Category: IBD
P5503 - Colobronchial Fistula Complicating Severe Crohn’s Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Lauren Duffy, BS (she/her/hers)
Washington State University Elson S. Floyd School of Medicine
Seattle, WA
Presenting Author(s)
Award: ACG Presidential Poster Award
Lauren Duffy, BS1, Evelyn H.. Rowe, BS2, Brian McNamee, MD3, Derek Khorsand, MD4, David H. Johnson, MD5
1Washington State University Elson S. Floyd School of Medicine, Seattle, WA; 2Washington State University Elson S. Floyd School of Medicine, Spokane, WA; 3Kootenai Imaging, Coeur d'Alene, ID; 4Kootenai Imaging/Radiology Associates of North Idaho, Coeur d’Alene, ID; 5Kootenai Clinic Gastroenterology and Endoscopy, Coeur d'Alene, ID
Introduction: We report the case of a 19-year-old male with Crohn’s colitis complicated by a colobronchial fistula. He initially presented to a local emergency department (ED) with severe diarrhea and hyponatremia. Stool studies were negative for C. difficile but positive for Shigella and Campylobacter and Azithromycin was initiated.
Case Description/
Methods: He was re-evaluated 4 days later in the ED for worsening symptoms with CT scan showing colonic wall irregularity and cecal dilation up to 12.6 cm concerning for toxic megacolon. Stool studies were then positive for C. difficile toxin by PCR. Tachycardia and leukocytosis of 15,000 were noted. Oral vancomycin was initiated.
A month later he returned to the ED with diarrhea, new dyspnea, and non-productive cough. Laboratory studies showed a hemoglobin of 6.7, platelets 570, and albumin of 1.4. Repeat CT showed diffuse mucosal hyperenhancement and a new fistula tract arising from the splenic flexure trans-diaphragmatically with dense consolidation of the left lung at this location and a pleural effusion.
He was admitted to the hospital, started on broad spectrum IV antibiotics, kept NPO, and started on TPN as albumin had fallen to 0.8. A balloon occlusion retrograde barium enema showed featureless colonic mucosa and a colobronchial fistula extending from the superior portion of the splenic flexure (Image). A diverting ileostomy was recommended but initially deferred. Flexible sigmoidoscopy for tissue diagnosis was performed as well as pre-biologic testing.
Pathology showed changes consistent with primary IBD, confirming a diagnosis of Crohn’s colitis. Infliximab was initiated at 5 mg/kg and steroids were avoided. Thoracic surgery was consulted due to progression of the pleural effusion and a chest tube was placed. A second 5mg/kg dose was given on day 3. He rapidly improved, remained on oral vancomycin, and a diet was resumed. Albumin had improved to 2.1, TPN and broad spectrum antibiotics were discontinued, and azathioprine 50 mg was added.
He was transferred to a regional center where a diverting loop ileostomy was completed. At outpatient follow-up 6 weeks after transfer, he had gained 20 pounds, had normal hemoglobin and platelet counts, and albumin was 4.5. At 1 year follow-up, he maintained a normal weight, had good ileostomy function, and was attending college.
Discussion: This case underscores the importance of recognizing inflammatory colitis, aggressive medical therapy, and a multidisciplinary approach to care of complex IBD patients.
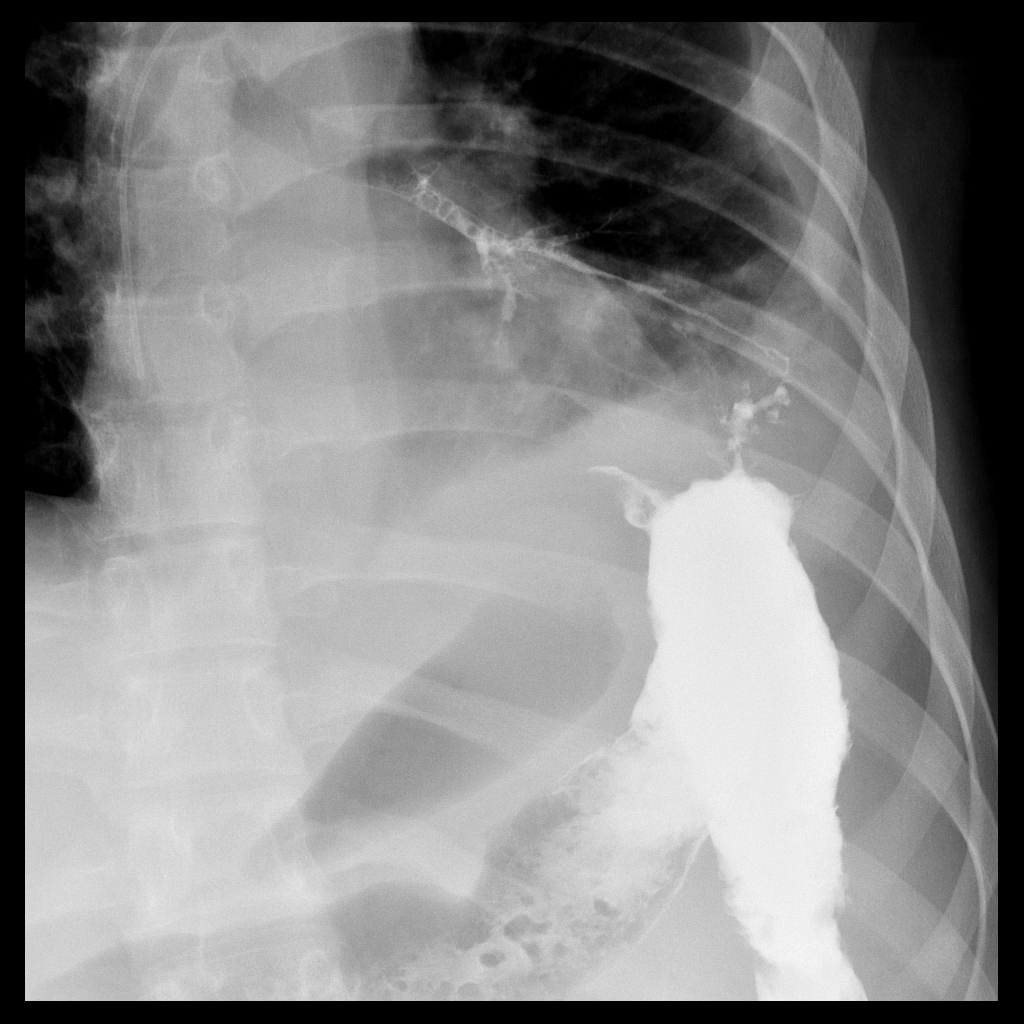
Figure: Image. Trans-diaphragmatic fistula extending from the splenic flexure to left lower lobe bronchus.
Disclosures:
Lauren Duffy indicated no relevant financial relationships.
Evelyn Rowe indicated no relevant financial relationships.
Brian McNamee indicated no relevant financial relationships.
Derek Khorsand indicated no relevant financial relationships.
David Johnson: Abbvie – Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Takeda – Advisory Committee/Board Member.
Lauren Duffy, BS1, Evelyn H.. Rowe, BS2, Brian McNamee, MD3, Derek Khorsand, MD4, David H. Johnson, MD5. P5503 - Colobronchial Fistula Complicating Severe Crohn’s Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lauren Duffy, BS1, Evelyn H.. Rowe, BS2, Brian McNamee, MD3, Derek Khorsand, MD4, David H. Johnson, MD5
1Washington State University Elson S. Floyd School of Medicine, Seattle, WA; 2Washington State University Elson S. Floyd School of Medicine, Spokane, WA; 3Kootenai Imaging, Coeur d'Alene, ID; 4Kootenai Imaging/Radiology Associates of North Idaho, Coeur d’Alene, ID; 5Kootenai Clinic Gastroenterology and Endoscopy, Coeur d'Alene, ID
Introduction: We report the case of a 19-year-old male with Crohn’s colitis complicated by a colobronchial fistula. He initially presented to a local emergency department (ED) with severe diarrhea and hyponatremia. Stool studies were negative for C. difficile but positive for Shigella and Campylobacter and Azithromycin was initiated.
Case Description/
Methods: He was re-evaluated 4 days later in the ED for worsening symptoms with CT scan showing colonic wall irregularity and cecal dilation up to 12.6 cm concerning for toxic megacolon. Stool studies were then positive for C. difficile toxin by PCR. Tachycardia and leukocytosis of 15,000 were noted. Oral vancomycin was initiated.
A month later he returned to the ED with diarrhea, new dyspnea, and non-productive cough. Laboratory studies showed a hemoglobin of 6.7, platelets 570, and albumin of 1.4. Repeat CT showed diffuse mucosal hyperenhancement and a new fistula tract arising from the splenic flexure trans-diaphragmatically with dense consolidation of the left lung at this location and a pleural effusion.
He was admitted to the hospital, started on broad spectrum IV antibiotics, kept NPO, and started on TPN as albumin had fallen to 0.8. A balloon occlusion retrograde barium enema showed featureless colonic mucosa and a colobronchial fistula extending from the superior portion of the splenic flexure (Image). A diverting ileostomy was recommended but initially deferred. Flexible sigmoidoscopy for tissue diagnosis was performed as well as pre-biologic testing.
Pathology showed changes consistent with primary IBD, confirming a diagnosis of Crohn’s colitis. Infliximab was initiated at 5 mg/kg and steroids were avoided. Thoracic surgery was consulted due to progression of the pleural effusion and a chest tube was placed. A second 5mg/kg dose was given on day 3. He rapidly improved, remained on oral vancomycin, and a diet was resumed. Albumin had improved to 2.1, TPN and broad spectrum antibiotics were discontinued, and azathioprine 50 mg was added.
He was transferred to a regional center where a diverting loop ileostomy was completed. At outpatient follow-up 6 weeks after transfer, he had gained 20 pounds, had normal hemoglobin and platelet counts, and albumin was 4.5. At 1 year follow-up, he maintained a normal weight, had good ileostomy function, and was attending college.
Discussion: This case underscores the importance of recognizing inflammatory colitis, aggressive medical therapy, and a multidisciplinary approach to care of complex IBD patients.
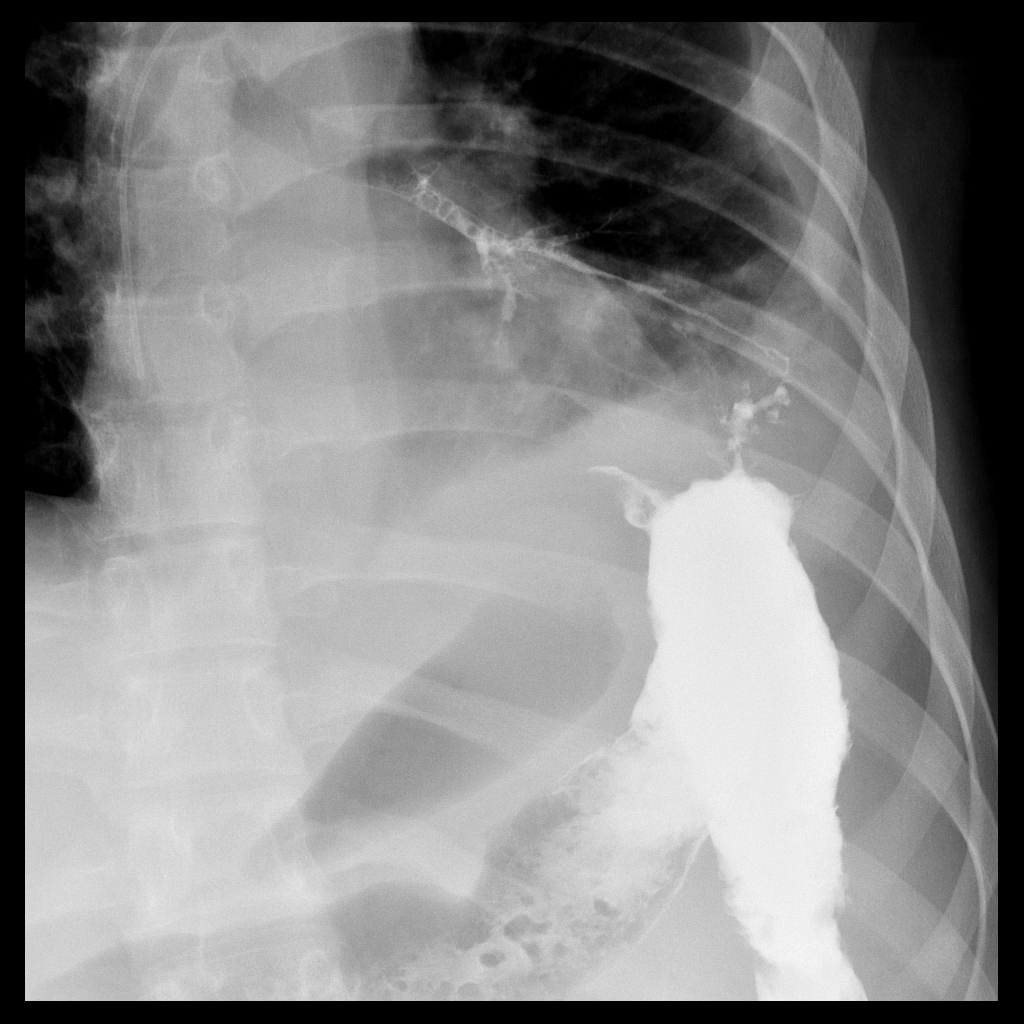
Figure: Image. Trans-diaphragmatic fistula extending from the splenic flexure to left lower lobe bronchus.
Disclosures:
Lauren Duffy indicated no relevant financial relationships.
Evelyn Rowe indicated no relevant financial relationships.
Brian McNamee indicated no relevant financial relationships.
Derek Khorsand indicated no relevant financial relationships.
David Johnson: Abbvie – Speakers Bureau. Bristol Myers Squibb – Speakers Bureau. Takeda – Advisory Committee/Board Member.
Lauren Duffy, BS1, Evelyn H.. Rowe, BS2, Brian McNamee, MD3, Derek Khorsand, MD4, David H. Johnson, MD5. P5503 - Colobronchial Fistula Complicating Severe Crohn’s Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

